Medical expert of the article
New publications
Broughton-Secker syndrome
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Among the numerous neurological diseases, Brown-Sequard syndrome stands out, which is also called hemiparaplegic syndrome or Brown-Sequard hemiplegia (from the Greek hemi – half). It occurs as a result of unilateral damage to the spinal cord, in particular, in the cervical spine. [ 1 ]
The disease is classified as a paralytic syndrome, and in ICD-10 its code is G83.81.
Causes Brown-Secker syndrome
There are various reasons for the syndrome of damage to half of the spinal cord, and most often its damage is associated with:
- blunt or penetrating spinal cord injury, fracture of the vertebrae in the neck or back;
- prolonged compression of the spinal cord;
- herniated disc, as well as spondylosis of the cervical spine (C1-C8);
- protrusion of the spinal disc in the same section; [ 4 ]
- spinal cord neoplasm, including angioma and intramedullary tumor;
- arachnoid or ganglion cyst of the spine;
- intradural spinal hernia;
- epidural hematoma of the spinal cord at the level of the thoracic spine (Th1-Th12);
- demyelination of nerve roots in the cervical spine, including in patients with multiple sclerosis.
Diseases that lead to damage to part of the spinal cord include tuberculosis of the spine. And the development of syndrome due to dissection of the vertebral artery, in which blood flow in the spinal vessels decreases with ischemic damage - spinal cord infarction, is considered an extremely rare case. [ 5 ], [ 6 ], [ 7 ], [ 8 ]
Risk factors
Based on the main causes of hemiparaplegic syndrome, the risk factors for its development are:
- injuries from gunshot or knife wounds to the neck or back, falls from a height or car accidents;
- pathological changes in the structures of the spine of a degenerative nature, as well as its lateral curvature (kyphosis);
- spinal cord tumors (primary or metastatic);
- inflammatory processes in the spine;
- hemorrhages in the spinal cord caused by vascular damage;
- bacterial or viral infections with the development of tuberculosis, neurosyphilis (tabes dorsalis), meningitis, shingles, etc.;
- manual and radiation therapy, long-term use of anticoagulants.
Pathogenesis
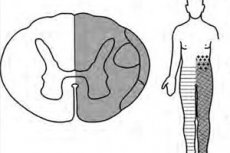
The pathogenesis of spinal hemiparaplegia is caused by a disruption of neuromuscular transmission due to damage to one side of the spinal cord with destruction of the fibers of the lateral nerve tracts: corticospinal (pyramidal), spinothalamic (extrapyramidal), as well as the medial lemniscal tract of the dorsal columns.
The fibers of the conducting nerve pathways, consisting of motor and sensory neurons and their processes - axons, do not go straight, but repeatedly cross with the transition to the opposite side. This means that unilateral damage to the spinal cord, provoking the development of Brown-Sequard syndrome, leads to its manifestations both on the same side as the alteration of nerve fibers - ipsilateral, and on the opposite, that is, contralateral side of the body.
In the absence of transmission of nerve signals along the lateral corticospinal tract, motor function is lost. And the result of the disruption of neurosensory conduction along the lateral spinothalamic and middle lemniscal tracts is the loss of nociception (pain sensations) - with persistent hypalgia, proprioception (mechanosensory sensation of body position and movement) and tactile (tactile) sensations, including temperature - with pronounced thermoesthesia.
More information in the materials:
Symptoms Brown-Secker syndrome
Depending on the location of the spinal cord injury, there are such types of Brown-Sequard syndrome as right-sided and left-sided. And according to the clinical manifestation - complete (inverted) and incomplete (partial); most patients have an incomplete form.
The first signs of this syndrome are: loss of sensation of pain, temperature, light touch, vibration and position of the leg joints – below the spinal cord alteration zone (on the same side of the body).
The main clinical symptoms reflect hemisectional damage to the spinal cord and are manifested as:
- loss of motor function – flaccid (spastic) paraparesis or hemiparesis (hemiplegia) with weakening of the ipsilateral lower limb;
- contralateral loss (below the affected area) of pain sensation, plantar reaction and temperature sensitivity;
- impaired coordination of movements - ataxia;
- loss of bladder and bowel control.
Complications and consequences
Possible complications are associated with loss of sensitivity (which increases the risk of cuts and burns) and weakening - hypotonia of muscles, which, under conditions of limited mobility, can lead to their atrophy.
The most severe consequences occur when the syndrome progresses to complete paralysis.
Diagnostics Brown-Secker syndrome
Early diagnosis plays a vital role in preventing irreversible consequences of hemiparaplegic syndrome.
Neurologists examine the patient, studying reflexes - deep and superficial, and also assess the degree of functional and neurological disorders.
Laboratory tests – biochemical and immunological blood tests, as well as cerebrospinal fluid tests – may be required in complex cases (non-traumatic origin of the syndrome) and to clarify the diagnosis.
The key diagnostic method is instrumental diagnostics: X-ray of the spine and spinal cord, computed tomography and MRI of the spine, electroneuromyography, CT myelography.
Differential diagnosis
Differential diagnosis includes motor neuron diseases (primarily amyotrophic lateral sclerosis), progressive spinal muscle atrophy, hereditary motor-sensory polyneuropathies and spinocerebellar ataxias, Mills and Horner syndromes, multiple sclerosis, [ 9 ] virtually all spinal cord-related alternating syndromes, and stroke. [ 10 ]
Who to contact?
Treatment Brown-Secker syndrome
Standard treatment for Brown-Sequard hemiplegia is directed at the underlying cause, once this has been clearly identified. Medications may be used to relieve or reduce the intensity of some symptoms.
Although high doses of corticosteroids are used in practice, their effectiveness remains controversial.
In Brown-Sequard syndrome, etiologically associated with multiple sclerosis, an immune stimulant, B-immunoferon 1a, is used.
In case of Brown-Sequard syndrome caused by a herniated cervical intervertebral disc, surgical treatment is used: discectomy, spondylodesis, laminectomy.
And the treatment of epidural hematoma of the spinal cord is carried out by its surgical drainage. Decompression surgery is recommended for patients with trauma, tumor or abscess causing compression of the spinal cord. [ 11 ], [ 12 ]
All patients with Brown-Sequard syndrome require comprehensive rehabilitation, which can help partially restore motor skills (due to the preserved functions of descending motor axons of the conducting nerve pathways). For this purpose, various physiotherapeutic procedures are used, as well as locomotor therapy using a robotic treadmill with body weight support.
Prevention
There are no special preventive measures to prevent unilateral spinal cord injury with the development of hemiparaplegic syndrome.
Forecast
In Brown-Séquard syndrome, the prognosis varies depending on its etiology and the degree of clinical manifestation, and is not good regarding functional improvement. More than half of patients with BSS recover well, and most post-traumatic patients recover motor function. Recovery slows over three to six months, and permanent neurological recovery may take up to two years. [ 13 ] If the deficit is at the level where it affects the bowel and bladder, patients can recover function in 90% of cases. Most patients recover some strength in the lower extremities, and most regain functional walking ability. When motor loss is present, recovery is faster on the contralateral side and slower on the ipsilateral side.

