Medical expert of the article
New publications
Reflex study
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

In clinical practice, deep (muscle stretching) and superficial (skin, mucous membrane) reflexes are examined.
Deep (myotatic) reflex - involuntary contraction of a muscle in response to stimulation of the muscle spindle receptors contained in it, which, in turn, is caused by passive stretching of the muscle. Such stretching in clinical practice is usually achieved by a short, abrupt blow of a neurological hammer to the tendon of the muscle.
The characteristics of deep reflexes reflect the integrity of the entire reflex arc (the state of the sensory and motor fibers of the peripheral nerve, the posterior and anterior roots of the spinal nerves, the corresponding segments of the spinal cord), as well as the ratio of inhibitory and activating suprasegmental influences. A deep reflex is evoked by a light, quick blow to the tendon of a relaxed and slightly stretched muscle. When striking, the hand should make a free oscillatory movement in the wrist joint, the handle of the neurological hammer is held loosely so that the hammer can make some additional oscillatory movement around the point of its fixation. "Pounding" movements of the hand should be avoided. The patient should be in a sufficiently relaxed state and not make efforts to maintain balance; his limbs should be located symmetrically. If the patient tenses the muscle, the reflex decreases or disappears altogether. Therefore, if the reflex is difficult to elicit, the patient's attention is diverted from the area being examined: for example (when examining reflexes from the legs), they are asked to clench their teeth tightly or clasp the fingers of both hands and forcefully pull their hands to the sides (the Jendrasik maneuver).

The intensity of deep reflexes is sometimes assessed on a 4-point scale: 4 points - sharply increased reflex; 3 points - brisk, but within normal limits; 2 points - normal intensity; 1 point - decreased; 0 points - absent. The intensity of reflexes in healthy individuals can vary significantly.
Normally, reflexes in the legs are usually expressed more clearly and are evoked more easily than in the arms. A slight bilateral increase in deep reflexes does not always indicate damage to the pyramidal system; it can also be observed in a number of healthy individuals with increased excitability of the nervous system. A sharp increase in deep reflexes, often combined with spasticity, indicates damage to the pyramidal system. A decrease or absence of reflexes should be alarming: does the patient have neuropathy or polyneuropathy? Bilateral hyporeflexia and hyperreflexia have less diagnostic value compared to asymmetry of reflexes, which usually indicates the presence of a disease.
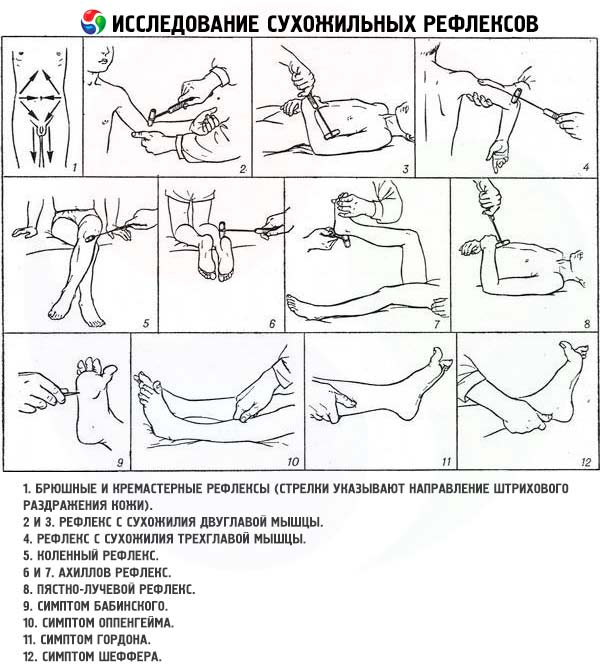
Deep reflex study
- The reflex from the biceps tendon (biceps reflex, flexion-elbow reflex) closes at the level of C5 - C6 . The doctor places the patient's arm, slightly bent at the elbow joint, on his forearm, grasps the elbow joint with four fingers from below, and places the thumb in the relaxed upper limb of the patient on the stomach, the elbow joint rests on the bed from above on the biceps tendon. They strike a short and quick blow with a hammer on the thumb of their hand. They evaluate the contraction of the biceps brachii and the degree of flexion of the patient's arm.
- The reflex from the triceps tendon (triceps reflex, elbow extension reflex) closes at the level of C7 - C8 . The doctor, standing in front of the patient, supports his half-bent arm by the elbow joint and forearm (or supports the patient's abducted shoulder directly above the elbow joint, with the forearm hanging freely down) and strikes the triceps tendon with a hammer 1-1.5 cm above the olecranon process of the ulna. The degree of reflex extension of the arm at the elbow joint is assessed.
- The carporadial reflex closes at the level of C5 - C8 . The doctor freely places the patient's hand on his wrist so that it is bent at the elbow joint at an angle of approximately 100°, and the forearm is in a position between pronation and supination. Strikes with a hammer are applied to the styloid process of the radius, assessing flexion at the elbow joint and pronation of the forearm. The examination is carried out similarly with the patient lying on his back, but the hands of his arms, bent at the elbow joints, are on the stomach. If the reflex is examined with the patient in a standing position, the hand of his arm, half-bent at the elbow joint, is held in the required (semi-prostrate) position by the doctor's hand. When examining deep reflexes on the arm, special attention should be paid to the zone of distribution of the reflex reaction. For example, when inducing a flexion-ulnar or carporadial reflex, the fingers of the hand may bend, which indicates damage to the central motor neuron. Sometimes an inversion (distortion) of the reflex is observed: for example, when inducing a biceps reflex, a contraction of the triceps muscle of the shoulder, rather than the biceps, occurs. Such a disorder is explained by the spread of excitation to adjacent segments of the spinal cord if the patient has damage to the anterior root innervating the biceps muscle of the shoulder.
- The knee reflex closes at the level of L3 - L4 . When testing this reflex in a patient lying on his back, the legs should be in a semi-bent position, and the feet should be in contact with the couch. To help the patient relax the thigh muscles, the doctor places his hands under his knees, supporting them. If relaxation is insufficient, the patient is asked to press hard with his feet on the couch or the Jendrasik maneuver is used. Hammer blows are applied to the tendon of the quadriceps femoris below the kneecap. The degree of extension in the knee joint is assessed, noting whether the reflex reaction extends to the adductor muscles of the thigh. When testing the reflex in a sitting patient, his heels must be in free contact with the floor, and the legs must be bent at an obtuse angle at the knee joints. With one hand, grasp the distal part of the patient's thigh, with the other - strike the tendon of the quadriceps femoris with a hammer. With this type of examination, the reflex contraction of the muscle can not only be seen, but also felt with the hand on the thigh. The knee reflex can also be examined when the patient is sitting in a "leg over leg" position or when he sits on a high chair so that his shins hang freely, not touching the floor. These options allow one to observe a poorly damped, "pendulum-like" knee reflex (in case of cerebellar pathology) or the Gordon reflex (in case of Huntington's chorea or chorea minor), which consists in the fact that after a blow to the tendon of the quadriceps femoris, the shin unbends and remains in this position for some time.

- The Achilles reflex closes at the level of S 1 -S 2. The essence of this reflex is that with a patient lying on his back, one hand grasps the foot of the leg being examined, bends the leg at the hip and knee joints and simultaneously extends the foot. With the other hand, strike the Achilles tendon with a hammer. To study the reflex with the patient lying on his stomach, bend his leg at a right angle at the knee and ankle joints. Hold the foot with one hand, slightly straightening it at the ankle joint (dorsal flexion), and with the other hand lightly strike the Achilles tendon. You can also ask the patient to kneel on the couch so that the feet hang freely over its edge; strike the Achilles tendon with a hammer, assessing the degree of extension in the ankle joint.

When examining deep reflexes from the legs, it is simultaneously checked for clonus of the foot or patella. Clonus is a repeated involuntary rhythmic contraction of a muscle caused by rapid passive stretching of the muscle itself or its tendon. Clonus occurs when the central motor neuron (pyramidal system) is damaged due to the loss of supraspinal inhibitory influences. Increased deep reflexes in the lower limb are often combined with clonus of the foot and patella. To induce clonus of the foot in a patient lying on his back, bend the leg at the hip and knee joints, holding it with one hand by the lower third of the thigh, and grasp the foot with the other hand. After maximum plantar flexion, suddenly and strongly straighten the foot at the ankle, and then continue to apply pressure to it, holding it in this position. In a patient with spastic muscle paresis, this test often causes clonus of the foot - rhythmic flexion and extension of the foot due to repeated contractions of the gastrocnemius muscle, which occur in response to stretching of the Achilles tendon. Several oscillatory movements of the foot are possible in healthy individuals, but persistent clonus (five or more flexion-extension movements) indicates pathology. The test to detect clonus of the patella is carried out with the patient lying on his back with straight legs. Grasping the upper edge of the patella with the thumb and index finger, move it up together with the skin, and then sharply move it down, holding it in the extreme position. In patients with severe spasticity, such a test causes rhythmic oscillations of the patella up and down, caused by stretching of the tendon of the quadriceps femoris.
Study of skin (superficial) reflexes
- Abdominal skin reflexes are evoked by stroking the abdominal skin on both sides toward the midline. To evoke the upper abdominal reflex, stroking is applied directly below the costal arches (the reflex arc closes at the level of T7 - T8 ). To evoke the middle abdominal reflex (T9 - T10 ), stimulation is applied horizontally at the level of the navel, and the lower abdominal reflex (T11 - T12 ) is applied above the inguinal ligament. Stimulation is caused by a blunt wooden stick. The response is contraction of the abdominal muscles. With repeated stimulation, abdominal reflexes decrease (“become exhausted”). Abdominal reflexes are often absent in obesity, in the elderly, in multiparous women, and in patients who have undergone abdominal surgery. Asymmetry of abdominal reflexes may be of diagnostic value. Their unilateral loss may indicate an ipsilateral spinal cord lesion (interruption of the pyramidal tract in the lateral funiculi of the spinal cord above the level of T6 - T8 ) or a contralateral brain lesion involving the motor areas of the cerebral cortex or the pyramidal system at the level of the subcortical formations or brainstem.
- The plantar reflex (closes at the level of L5 - S2 ) is caused by stroking the outer edge of the sole in the direction from the heel to the little toe, and then in the transverse direction to the base of the first toe. Skin irritation should be sufficient in strength and last for approximately 1 s. Normally, in adults and children over 1.5-2 years of age, plantar flexion of the toes occurs in response to irritation.
- The cremasteric reflex (closed at the level of L 1 -L 2 ) is caused by stroking the skin of the inner thigh, directed from the bottom up. Normally, this causes contraction of the muscle that lifts the testicle.
- The anal reflex (closed at the level of S4 - S5 ) is caused by irritation of the skin around the anus. The patient is asked to lie on his side and bend his knees, and the edge of the anus is lightly touched with a thin wooden stick. The response is normally a contraction of the external anal sphincter, and sometimes of the gluteal muscles.
Pathological reflexes appear when the central motor neuron (pyramidal system) is damaged. Reflexes evoked from the extremities are divided into extension (extensor) and flexion (flexor). Oral automatism reflexes are also considered pathological (in adults).
Pathological extensor reflexes
- The Babinski reflex (extensor plantar reflex) is the most important diagnostic symptom indicating damage to the central motor neuron. It manifests itself as an abnormal response to stroke stimulation of the outer edge of the sole: instead of the normally observed plantar flexion of the toes, there is a slow tonic extension of the first toe and a slight fan-shaped divergence of the other toes. At the same time, a slight flexion of the leg at the knee and hip joints is sometimes observed. It should be taken into account that if the Babinski symptom is weakly expressed, repeated attempts to evoke it often lead only to further fading of the reflex, therefore, in doubtful cases, it is necessary to wait a few minutes before trying again to identify the extensor plantar reflex. In children under 2-2.5 years of age, the extensor plantar reflex is not pathological, but at an older age its presence always indicates pathology. It is important to remember that the absence of the Babinski reflex does not exclude damage to the central motor neuron. For example, it may be absent in a patient with central paresis with severe weakness of the leg muscles (the big toe is unable to straighten) or with concomitant interruption of the afferent part of the corresponding reflex arc. In such patients, stroke stimulation of the edge of the sole does not cause any response - neither the normal plantar reflex, nor the Babinski symptom.
- Oppenheim reflex: with the patient lying on his back, the test is performed by pressing the pad of the thumb on the anterior surface of the shin (along the inner edge of the tibia) in a downward direction, from the knee to the ankle joint. The pathological response is extension of the patient's first toe.
- Gordon's reflex: the patient's gastrocnemius muscle is squeezed with the hands. The pathological reflex is extension of the first toe or all toes.
- Chaddock's reflex: a stroking of the skin of the lateral edge of the foot is applied just below the outer malleolus in the direction from the heel to the dorsum of the foot. The pathological response is extension of the first toe.
- Schaeffer's reflex: the patient's Achilles tendon is compressed with the fingers. The pathological reflex is extension of the first toe.
Pathological flexion reflexes
- Upper Rossolimo reflex (Tromner reflex). The patient relaxes his arm and hand. The doctor grasps the patient's hand so that its fingers hang freely, and with a quick, jerky movement strikes the palmar surface of the tips of the patient's half-bent fingers in the direction from the palm. In case of a pathological reaction, the patient flexes the distal phalanx of the thumb and excessively flexes the distal phalanxes of the fingers. A qualitative modernization of the grip of the hand for studying such a reflex was proposed by E. L. Venderovich (Rossolimo-Venderovich reflex): with the patient's hand supinated, the blow is applied to the distal phalanges of the II-V fingers slightly bent at the interphalangeal joints
- Rossolimo reflex. With the patient lying on his back, the fingers of the hand are quickly and abruptly struck on the plantar surface of the distal phalanges of the toes in the direction of its back. The pathological reflex manifests itself as a rapid plantar flexion of all toes.
- Lower Bekhterev-Mendel reflex. The patient is lying on his back and tapped with a skein on the back of the foot in the area of the III-IV metatarsal bones. The pathological reflex consists of rapid plantar flexion of the II-V toes.
Oral automatism reflexes
Some of these reflexes (for example, sucking) are observed in children in the first year of life, but as the brain matures, they disappear. Their presence in adults indicates bilateral damage to the cortico-nuclear pathways and a decrease in the inhibitory effect of the frontal lobe.
- The proboscis reflex is evoked by tapping the patient's lips. The patient is asked to close his eyes and his lips are lightly tapped with a hammer. If the patient's reflex is positive, the orbicularis oris muscle contracts and the lips are pulled forward. The same reaction, which occurs in response to a finger approaching the patient's lips, is called the Karchikyan distant-oral reflex.
- The sucking reflex is manifested by involuntary sucking or swallowing movements in response to a stroking irritation of the patient's closed lips.
- Astvatsaturov's nasolabial reflex is expressed in the extension of the lips forward in response to light tapping with a hammer on the bridge of the nose.
- The Marinescu-Radovic palmomental reflex is caused by stroking (with a match, the handle of a hammer) the skin of the palm above the eminence of the thumb; it manifests itself by pulling the skin of the chin upward (contraction of the ipsilateral mentalis muscle - m. mentalis). This reflex is sometimes detected even in the absence of any pathology.
- The glabellar reflex (from the Latin glabella - the bridge of the nose) is caused by percussion in the area of the bridge of the nose, that is, by lightly tapping with a hammer at a point located in the middle between the inner edges of the eyebrows. Normally, in response to the first blows, the patient blinks, then the blinking stops. A reaction in which the patient continues to close the eyelids with each blow of the hammer is considered pathological. A positive glabellar reflex is observed in cases of frontal lobe damage, as well as in some extrapyramidal disorders.

Protective reflexes occur in central paralysis and are involuntary movements in the paralyzed limb that occur in response to intense irritation of the skin or subcutaneous tissue. An example of protective reflexes is the Bekhterev-Marie-Foix shortening reflex, which consists of flexion of the leg at the hip and knee joints, combined with dorsiflexion of the foot at the ankle joint ("triple shortening" of the leg) in response to strong passive plantar flexion of the toes of the paralyzed leg (or other strong irritation).
The grasping reflex is observed in cases of extensive damage to the frontal lobe. The reflex is evoked by a stroke irritation of the patient's palm at the base of the fingers (above the metacarpophalangeal joints), which is imperceptible to the patient, or by touching it with the handle of a hammer or some other object. It manifests itself as an involuntary grasping of the object that irritated the skin. In extreme cases of this reflex, even touching the patient's palm can cause a grasping movement.

