Medical expert of the article
New publications
Auscultation of the heart
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Auscultation is one of the most important methods of examining the heart. It is best to use a stethoscope, which should have a membrane for the best perception of high-frequency sounds (phonendoscope). In this case, the membrane is applied to the chest quite tightly. The information content of auscultation is highest in identifying heart defects. In this case, the final diagnosis is often made based on listening to the heart. To master this method, daily practice is required, during which it is necessary to initially learn to correctly perceive the normal auscultatory picture of the heart.
The bell of the phonendoscope is applied fairly tightly to the surface of the chest in the area of the heart projection. In some patients, auscultation is hampered by excessive hair growth, which sometimes has to be shaved or moistened with soapy water. Auscultation should be performed primarily with the patient lying on his back, in some cases (see below) supplemented by auscultation in a position on the left side, on the stomach, standing or sitting, with breath holding on inhalation or exhalation, after physical exertion.
All these techniques allow us to detect a number of symptoms that have important diagnostic value and often determine the tactics of patient management.
Heart sounds
In healthy people, two tones are heard over the entire area of the heart:
- I tone, which occurs at the beginning of ventricular systole and is called systolic, and
- The second tone occurs at the beginning of diastole and is called diastolic.
The origin of heart sounds is associated primarily with vibrations that occur in its valves during myocardial contractions.
The first tone occurs at the beginning of ventricular systole already at the time when the cusps of the left (mitral) and right (tricuspid) atrioventricular valves have slammed shut, i.e. during the period of isometric contraction of the ventricles. The greatest significance in its occurrence is given to the tension of the left and right atrioventricular valves, consisting of elastic tissue. In addition, the oscillatory movements of the myocardium of both ventricles during their systolic tension play a role in the formation of the first tone. Other components of the first tone are of lesser importance: the vascular one is associated with the oscillations of the initial sections of the aorta and pulmonary trunk when they are stretched by blood, the atrial one is associated with their contraction.
The second tone occurs at the beginning of diastole as a result of the slamming of the valves of the aorta and pulmonary artery.
Under normal conditions, it is relatively easy to distinguish the first tone from the second tone, since a relatively short systolic pause is determined between them. Between the first and second tones during diastole, the pause will be significantly longer. When the rhythm increases, it may be difficult to identify the tones. It should be borne in mind that the first tone corresponds to a heart beat or an easily determined pulsation of the carotid artery.
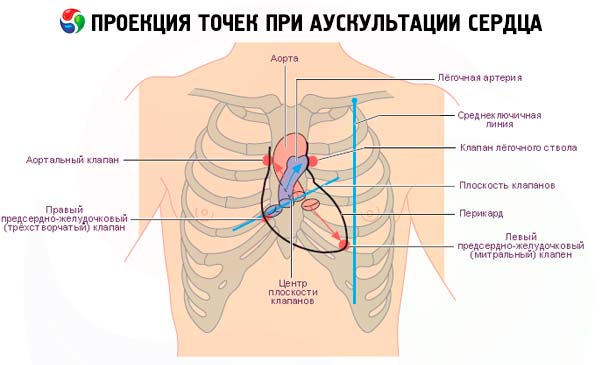
Heart auscultation points
The occurrence of tones, as well as other sounds in the heart, as already mentioned, is associated primarily with the vibrations of the heart valves, which are located between the atria and ventricles and between the ventricles and large vessels. Each valve opening corresponds to a certain point for listening. These points do not exactly coincide with the places of projection of the valves on the anterior chest wall. Sounds that occur in the valve openings are conducted along the blood flow.
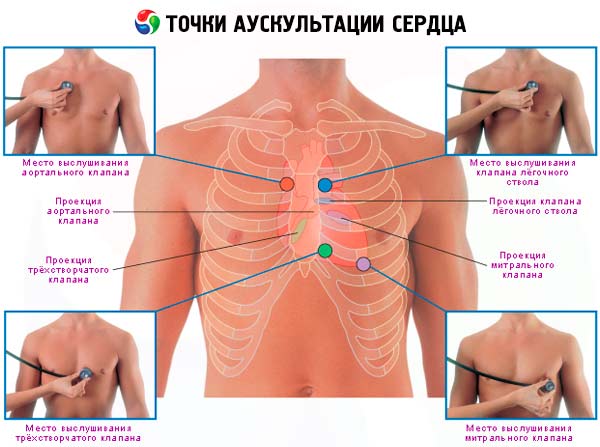
The following points have been established for the best listening to the heart valves:
- mitral valve - the apex of the heart;
- tricuspid valve - lower part of the body of the sternum;
- aortic valve - the second intercostal space on the right at the edge of the sternum;
- pulmonary valve - the second intercostal space on the left at the edge of the sternum;
- the so-called V point is the third intercostal space on the left near the sternum; auscultation of this area allows one to more clearly hear the diastolic murmur that occurs with aortic valve insufficiency.
The second heart sound and its components associated with the slamming of the semilunar flaps of the aortic and pulmonary artery valves are always better heard and assessed by the auscultatory picture in the second intercostal space on the left or right at the edge of the sternum. The first heart sound, associated primarily with the tension of the mitral valve cusps, is assessed by auscultation at the apex of the heart, as well as at the lower edge of the sternum. Thus, we speak of the strengthening or weakening of the second heart sound when listening at the base of the heart (second intercostal space), and of the strengthening or weakening of the first heart sound when listening at the apex. If the second heart sound consists of two components when listening at the base of the heart, we can speak of its bifurcation. If we listen to an additional component after the second heart sound at the apex, we should speak not of the splitting or bifurcation of the second heart sound, but of the appearance of an additional heart sound following the second heart sound and obviously associated with valve vibrations.
The volume of heart sounds may change primarily under the influence of extracardiac factors. They may be worse heard with an increase in the thickness of the chest, in particular due to greater muscle mass, with the accumulation of fluid in the pericardial cavity. Conversely, with a thinner chest in thin people and especially with a more frequent rhythm (faster movement of the valves), heart sounds may be louder.
In children and asthenics, it is sometimes possible to hear the third and fourth tones.
The third tone is heard soon (0.15 s) after the second tone. It is caused by oscillations of the ventricular muscles during their rapid passive filling with blood (from the atria) at the beginning of diastole.
The fourth tone occurs before the first tone at the end of ventricular diastole and is associated with their rapid filling due to contractions of the atria.
Pathological changes in heart sounds
Weakening of both tones can be observed with pronounced diffuse damage to the ventricular myocardium and a decrease in their contractility.
Weakening of the first tone at the apex of the heart is also observed in case of damage to the heart valves, primarily the mitral valve, as well as the tricuspid valve, which leads to the absence of the so-called period of closed valves and a decrease in the valvular component of the first tone. The first tone also weakens in case of severe heart failure due to a decrease in its muscular component.
An increase in the first tone can be observed with a decrease in ventricular filling at the beginning of systole due to its muscular component, in which case the first tone is often defined as “clapping”.
Significant fluctuations in the intensity of the first tone are observed in atrial fibrillation due to differences in diastolic pauses and, consequently, in the filling of the left ventricle.
Weakening of the second tone occurs with low pressure in large vessels, a decrease in their blood filling. Weakening of the second tone can occur with damage to the valves of the aorta and pulmonary artery, which leads to a violation of their slamming.
The second tone intensifies with an increase in pressure in large vessels - the aorta or pulmonary artery; in this case, they speak of an accent of the second tone on one or the other vessel, respectively. In this case, the second tone, for example, on the right of the sternum is heard as significantly more intense than on the left, and vice versa. The accent of the second tone is explained by a faster slamming of the corresponding valves and a louder sound that is perceived during auscultation. The accent of the second tone on the aorta is determined in arterial hypertension, as well as in pronounced sclerotic changes in the aorta with a decrease in the elasticity of its walls. The accent of the second tone on the pulmonary artery is determined by an increase in pressure in it in patients with mitral valve defects and pulmonary heart disease.
Bifurcation of tones is said to occur when their main components are detected separately. Bifurcation of the second tone is usually noted. It may be associated with non-simultaneous slamming of the aortic and pulmonary artery valves, which is associated with different durations of contraction of the left and right ventricles due to changes in the large and small circulations, respectively. With an increase in pressure, for example, in the pulmonary artery, the second component of the second tone is associated with a later slamming of the pulmonary artery valve. In addition, bifurcation of the second tone is associated with an increase in blood filling in the small or large circulation.
A slight splitting of the second tone, as always heard at the base of the heart, i.e. in the second intercostal space, can also occur under physiological conditions. During a deep breath, due to the increased blood flow to the right heart, the duration of the systole of the right ventricle can be somewhat longer than that of the left, due to which a splitting of the second tone is heard on the pulmonary artery, with its second component associated with the slamming of the pulmonary artery valve. This physiological splitting of the second tone is better heard in young people.
Late closure of the pulmonary valve compared to the aortic valve is detected with dilation of the right ventricle, for example, with stenosis of the pulmonary artery opening or with a violation of the conduction of excitation along the right leg of the atrioventricular bundle (bundle of His), which also leads to late closure of the cusps of this valve.
In the case of an atrial septal defect, the increase in blood volume in the right atrium and then in the right ventricle leads to a wide splitting of the second sound, but since the right and left atriums are in constant communication with such a defect, the blood volume of the left and right ventricles fluctuates in this connection in one direction and coincides with the respiratory cycle. This leads to a fixed splitting of the second sound on the pulmonary artery, which is pathognomonic for an atrial septal defect.
In pulmonary hypertension in patients with chronic lung diseases, the splitting of the second sound is less pronounced and distinct, since the right ventricle (although it works against increased pressure in the lungs) is usually hypertrophied, and therefore its systole is not lengthened.
Additional heart sounds occur for many reasons. The mitral valve usually opens silently at the beginning of diastole. When the mitral valve cusps are sclerosed in patients with mitral stenosis, their opening at the beginning of diastole is limited, so the blood flow causes vibrations of these cusps, perceived as an additional sound. This sound is heard shortly after the second sound, but only at the apex of the heart, which indicates its connection with vibrations of the mitral valve. A similar tone of the opening of the tricuspid valve is heard at the lower part of the sternum, but quite rarely.
Systolic ejection tones are heard shortly after the first heart sound, they arise due to vibrations of the aortic or pulmonary valve, therefore they are better heard in the second intercostal space on the left or right at the edge of the sternum. Their appearance is also associated with the appearance of vibrations of the walls of large vessels, especially during their expansion. The aortic ejection sound is best heard at the point of the aorta. It is most often combined with congenital aortic stenosis. Bifurcation of the first sound can be observed with a violation of intraventricular conduction along the legs of the atrioventricular bundle, which leads to a delay in systole of one of the ventricles.
Aortic or mitral valve transplantation is now performed quite frequently. An artificial ball valve or a biological prosthesis is used. Mechanical valves produce two tones in each cardiac cycle, an opening tone and a closing tone. With a mitral prosthesis, a loud closing tone is heard after the first heart sound. The opening tone follows the second heart sound, as with mitral stenosis.
Gallop rhythm is a three-part heart rhythm that is heard against the background of tachycardia, i.e. increased rhythm, and indicates severe damage to the ventricular myocardium. An additional tone in the gallop rhythm can be heard at the end of diastole (before the first tone) - presystolic gallop rhythm and at the beginning of diastole (after the second tone) - protodiastolic gallop rhythm. The gallop rhythm is determined either at the apex of the heart, or in the third - fourth intercostal space on the left near the sternum.
The origin of these additional tones is associated with rapid filling of the ventricles at the beginning of diastole (additional III tone) and during atrial systole (additional IV tone) under conditions of sharply changed properties of the myocardium with a violation of its elasticity. When they occur against the background of tachycardia, sounds are heard, the rhythm of which resembles the gallop of a running horse. In this case, these III and IV heart tones are often heard almost simultaneously, causing the formation of a three-member rhythm. Unlike normal III and IV heart tones, which are found in young people with a normal heart rhythm, the gallop rhythm occurs in severe myocardial damage with dilation of the left ventricle and symptoms of heart failure.
An additional tone preceding the first tone against the background of a relatively rare heart rhythm can sometimes be heard in elderly people with a slightly changed heart. The third and fourth tones, including those corresponding to the gallop rhythm, are better heard when the patient is lying on the left side.

