Medical expert of the article
New publications
Atherosclerosis of the thoracic aorta
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
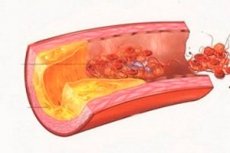
Thickening or hardening of the inner walls of the thoracic portion of the aorta (pars thoracica aortae) running in the posterior mediastinum, caused by cholesterol deposits, is diagnosed as thoracic aortic atherosclerosis. [1]
Epidemiology
Thoracic aortic atherosclerosis is common in adults of all ages, but statistically, it is more commonly identified in patients over the age of 60.
In more than 70% of patients with arterial hypertension, subclinical atherosclerosis affects the thoracic part of the aorta. In 48% of cases, the aortic arch is affected, in 44% - the descending part of the aorta, in 30% - its ascending part.
The incidence of focal calcification in thoracic aortic atherosclerosis is estimated to be approximately 8.5%. [2]
Causes of the thoracic aortic atherosclerosis.
Atherosclerotic lesion of the thoracic aorta is a local manifestation of systemic atherosclerosis, the causes of which are related to lipid metabolism disorders (dyslipidemia) in the body. And fat metabolism problems lead to elevated plasma cholesterol levels - hypercholesterolemia.
In dyslipidemia, total blood cholesterol levels are ≥240 mg/dL, low-density lipoprotein cholesterol (LDL) levels are ≥160 mg/dL, and high-density lipoprotein cholesterol (HDL) levels are <40 mg/dL. [3]
More information in the materials:
Risk factors
In addition to older age, risk factors for the development of atherosclerosis experts include:
- Smoking;
- Lack of physical activity;
- A large amount of animal fats in the diet;
- Alcoholism;
- Abdominal obesity, arterial hypertension, high blood glucose levels (in cases of type I diabetes mellitus) and insulin resistance (in cases of type II diabetes mellitus), leading to the development of metabolic syndrome - with impaired intravascular metabolism of LDL and HDL;
- Ischemic heart disease;
- Hypothyroidism;
- A chronic form of hepatitis;
- Inflammation of the pancreas (pancreatitis).
Pathogenesis
Atherosclerosis is a progressive disease whose pathogenesis is due to the accumulation of lipids and fibrotic elements in the walls of large arteries in the form of cholesterol deposits - atherosclerotic plaques.
First of all, there is a pathological change and dysfunction of the endothelium covering the inner membrane of blood vessels, which leads to an increase in the level of free radicals - oxidative stress.
At the next stage of atherogenesis, endothelial cells express intercellular adhesion molecules, which increases their permeability and further proliferation. [4]
Adaptive and innate immune responses lead to the development of an inflammatory process that is initiated by the interaction between oxidized low-density lipoproteins (LDL), macrophages that engulf them, and cellular immune lymphocytes (T cells) in the inner vascular sheath (tunica intima).
In the walls of blood vessels, oxidized LDL accumulate in lipid macrophages called foam cells. These cells, in turn, secrete a variety of proinflammatory cytokines and form cholesterol plaques that weaken the aortic wall, and their protrusion into the intima of the vessel narrows its lumen and leads to stenosis. [5]
Symptoms of the thoracic aortic atherosclerosis.
Thoracic atherosclerotic lesions can be asymptomatic, particularly in the first stage of plaque formation (fatty streak stage). Progression of the plaque may cause the first symptoms in the form of a strange sensation in the chest, pressure or pain in the mediastinum.
Symptoms with plaque enlargement may also include: sweating, dizziness or sudden weakness, confused breathing, fast or irregular heartbeat, nausea or vomiting.
There are different types of thoracic aortic atherosclerosis, such as non-stenotic, stenotic and atherosclerosis with calcification (the incidence of which increases with age, as well as in smokers and hypertensive patients).
Since atherosclerotic vascular disease is a systemic pathology, in almost 60% of cases there is atherosclerosis of several vessels, including atherosclerosis of the thoracic aorta and coronary arteries, as well as atherosclerosis of the aortic and carotid arteries. [6]
Complications and consequences
Atherosclerosis of the thoracic aorta - especially the aortic arch, its middle and distal parts - may be complicated by the formation of penetrating atherosclerotic ulcers and the development of acute aortic syndrome with intra-wall aortic hematoma and aortic dissection, as well as the formation of saccular thoracic aortic aneurysms, perforation and spontaneous rupture of the aorta.
Deep changes in the vascular wall as a result of atherosclerosis cause peripheral embolization (as a result of plaque fragment detachment with thrombus formation) - with the development of ischemic stroke or coronary circulatory failure.
Diagnostics of the thoracic aortic atherosclerosis.
The progression of atherosclerosis includes a protracted subclinical phase, with the disease often diagnosed after a cardiovascular exacerbation or at a late stage.
Laboratory tests include lipidogram: blood tests for total and LDL-CS cholesterol, triglycerides, lipids, lipoproteins and apolipoproteins. A biochemical blood test is also required.
Instrumental diagnosis is performed using aortic ultrasound, transesophageal echocardiography, thoracic aortography, CT or MR angiography.
Differential diagnosis is necessary to rule out aortitis, congenital aortic narrowing, primary aortic aneurysm, and hyperviscosity syndrome.
Treatment of the thoracic aortic atherosclerosis.
To treat symptomatic atherosclerosis, medications are used to help reduce the risk of serious complications. These are hypolipidemic drugs
Atorvastatin, simvastatin or wabadin, berlition and others. Read more:
Hypotensive drugs are used to lower BP, see - high blood pressure pills
Drugs that prevent blood clots include Aspirin, Clopidogrel (Plavix), and other platelet aggregation inhibitors.
Physiotherapeutic treatment is used, primarily water and mud therapy and exercise. It is recommended to follow diet for atherosclerosis.
Phytotherapists offer additional treatment with herbs using decoctions and infusions of common dandelion (roots and leaves), flowers of meadow clover, herbs of white milkvetch, flaxseed.
In cases of stenotic atherosclerosis, surgical treatment - endarterectomy, angioplasty, stenting of the affected part of the aorta - helps to widen the vessel lumen to normal. In extreme cases, endovascular aortic prosthesis is used. [7]
Read also - atherosclerosis - Treatment
Prevention
In order to prevent atherosclerotic lesions of blood vessels of any localization, it is recommended to stop smoking and systematic use of alcohol, reduce body weight, eat fruits, vegetables, whole grain products, fish and lean meat, low-fat dairy products, lead a more mobile lifestyle.
Forecast
In thoracic aortic atherosclerosis, the prognosis is determined by many factors, including the etiology of hypercholesterolemia and the presence of life-threatening complications.

