Medical expert of the article
New publications
Aplasia of the corpus callosum
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
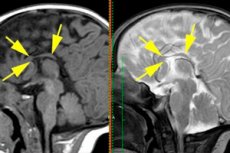
A developmental defect in the form of a complete or almost complete absence of adhesion of nerve fibers connecting the hemispheres of the brain is defined as aplasia of the corpus callosum, which is synonymous with its agenesis, that is, lack of formation in the development process. [ 1 ]
Epidemiology
Congenital malformations of the brain account for at least 25% of all anomalies of the embryonic period of ontogenesis.
According to some data, anomalies of the corpus callosum, including its agenesis (aplasia), are detected in 0.3-0.7% of patients who undergo MRI of the brain according to indications.
Isolated aplasia of the corpus callosum in children is a rare congenital defect, but as part of genetically determined syndromes it is considered a fairly common congenital anomaly, the prevalence of which is estimated at 230 cases per 10 thousand children with developmental problems.
In one third of cases of aplasia or partial agenesis of the corpus callosum, mental disorders are observed.
Causes aplasia of the corpus callosum
Aplasia of the corpus callosum, which provides communication between the hemispheres of the brain and their coordinated functioning, is a congenital defect, and in most cases, doctors cannot determine its exact causes. But most often these are chromosomal abnormalities that affect the intrauterine formation of the cerebral structures of the fetus, or a hereditary anomaly that is part of genetic syndromes with malformations of the brain. [ 2 ]
Thus, the corpus callosum is not formed in the fetus in cases of extra chromosome syndromes (trisomies), which include Warkany, Patau, and Edwards syndromes.
The absence of the corpus callosum is found in genetically determined Mowat-Wilson syndrome, Aicardi syndrome, Marden-Walker syndrome; Donn-Barrow, Anderman, Proud, Apert syndromes, X-linked hydrocephalus syndrome. And partial aplasia of the corpus callosum is characteristic of Pitt-Hopkins, Dandy-Walker, Sensenbrenner syndromes.
The formation of the corpus callosum is disrupted in cases of anomalies of the convolutions of the brain, such as schizencephaly, or in cases of congenital encephalocele and cysts of the brain structures (as in the case of Chudleigh-McCullough syndrome), as well as malformations or Arnold-Chiari syndrome. [ 3 ]
Risk factors
Among the probable risk factors for aplasia of the corpus callosum and other congenital cerebral defects are teratogenic effects on the embryo of increased radiation and various toxins; alcohol and drugs consumed during pregnancy; the use of certain medications and viral infections of the mother.
There is also an increased risk of this defect in a child if there is a family history of developmental disorders and brain dysgenesis.
Pathogenesis
The corpus callosum begins to form in the sixth to eighth week of pregnancy, but disturbances in this process can occur between the third and fifteenth weeks of gestation. In embryology, the pathogenesis of the absence of the corpus callosum is associated with two biological mechanisms.
First, it may be explained by defects in genes that regulate and coordinate dorsolateral migration—the movement of embryonic cells from the neural crest (the exodermal cell band at the edges of the neural tube) or the mesendoderm of the head to the sites of formation of brain structures. Most embryonic malformations and birth defects are the result of disruption of this process.
Another mechanism for agenesis of the corpus callosum may be that the axons of neocortical neurons do not cross the midline between the hemispheres of the embryonic brain, and instead of forming a fiber tract between the right and left hemispheres, abnormal bundles of nerve fibers are formed that are located longitudinally - without connecting the hemispheres of the brain. [ 4 ]
Symptoms aplasia of the corpus callosum
What symptoms does a disruption in communication between the hemispheres of the brain cause when there is no connection between them, which the corpus callosum should provide?
In infants, the first signs may include feeding problems and frequent seizures. However, in the presence of congenital syndromes, the clinical picture includes their symptoms, including abnormalities of the skull (microcephaly), facial skeleton (micrognathia) and facial features; oligodactyly or absence of fingers; spasticity and joint contractures, etc. [ 5 ]
With aplasia of the corpus callosum, a child may experience visual and hearing impairments, decreased muscle tone, and poor coordination of movements - with a significant delay in the onset of walking and motor development. There are also cognitive impairments (with an inability to perceive information, attention deficit, and problems with speech acquisition), and behavioral deviations (often similar to autism). [ 6 ]
Complications and consequences
Aplasia of the corpus callosum has sequelae and complications that vary depending on the associated brain abnormalities. Children with the most severe brain malformations may have seizures, spasticity, hydrocephalus, and physical and mental developmental disabilities.
Diagnostics aplasia of the corpus callosum
To establish a genetic diagnosis, molecular genetic studies, chromosomal and subtelomeric analyses are carried out. In prenatal pediatrics, genetic testing is practiced during pregnancy - using amniocentesis (analysis of amniotic fluid). [ 7 ]
Only instrumental diagnostics can detect pathology:
Visualization allows us to establish the presence of such specific structural features of partial aplasia as a rudimentary rostrum (anterior part of the corpus callosum) or aplasia of the posterior parts of the corpus callosum – radiatio corporis callosi and splenium. [ 8 ]
Differential diagnosis
To identify and differentiate other pathologies of the corpus callosum – dysgenesis (defective development), hypoplasia (partial underdevelopment), atrophy or hypoplasia of the callosum, as well as to confirm the presence of a genetic syndrome – differential diagnostics are carried out. [ 9 ]
Who to contact?
Treatment aplasia of the corpus callosum
There are no methods to restore the corpus callosum to its normal state. Therefore, treatment may consist of reducing the severity of the symptoms of this defect:
- use of anticonvulsants;
- physiotherapy, electroconvulsive therapy (to increase muscle strength and improve coordination of movements); [ 10 ]
- speech therapy;
- development of basic skills through occupational therapy.
Prevention
As a preventive measure, only the prevention of the teratogenic effects of various factors and prenatal diagnosis of congenital diseases can be considered.
Forecast
In general, the prognosis depends on the degree and severity of manifestations of aplasia of the corpus callosum and the presence/absence of concomitant developmental defects. [ 11 ]
In children with mild cases of this congenital anomaly, its negative neuropsychiatric consequences may be minimal, with almost normal functioning. And as adults, some people without a corpus callosum have average intelligence and live normal lives.

