Paralysis and paresis of facial muscles
Last reviewed: 07.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Neurological disorders in the form of inability or limitation of the ability of certain structures of the facial muscular system to perform any movements, including mimic movements (by which facial expressions externally manifest emotions), can be defined as paralysis and paresis of mimic muscles. [1]
Epidemiology
According to statistics cited in various sources, paralysis and paresis of mimic muscles are observed in 45-60% of patients even after the first ischemic stroke (this type of stroke accounts for 87% of all strokes).
Bell's palsy, with an estimated incidence of 20 cases per 100,000 people, accounts for at least 80% of all cases of facial nerve and facial muscle palsy. Approximately 15% of patients have only partial weakness of facial muscles. The incidence increases with age, from 40 to 60 years of age; compared to men, Bell's palsy is more common in women, and left-sided facial palsy is more common than right-sided palsy.
This condition develops in 10% of patients with Lyme disease, with 25% of cases of paralysis being bilateral.
Causes of the paralysis and paresis of the facial muscles
Plegia or paralysis mimic muscles of the face refers to a condition in which the possibility of voluntary muscle movements is completely lost, and paresis of the mimic muscles, that is, incomplete, flaccid or partial paralysis, manifests itself as weakness of the mimic muscles - with the ability to control the affected muscles.
Muscle contraction is "guided" by nerves, and in most cases the reasons for the absence of facial expression (amimia) and its partial disorder on one side of the face (hemiparesis) lie in damage to facial nerve, which innervates these muscles.
According to the origin of paralysis and paresis of mimic muscles are divided into central and peripheral, and the course - into temporary and permanent.Central paralysis of mimic muscles(moreover, the lower half of one side of the face) is the result of alteration of the upper motoneurons (motor neurons) of the facial nerve, which transmit bilateral input impulses to the facial motor nuclei (nucleus nervi facialis) of the pontomedullary junction (bridge) of the brainstem, as well as lesions of their descending pathways between the motor cortex and facial motor nuclei - the corticobulbar tract (pyramidal motor pathway of the CNS). At first, the paralysis may manifest itself as a flaccid paresis.
More details in the publication - motoneuron Diseases
Facial musculature immobility is provoked by brain injuries (including fracture of the skull base or temporal bones), ischemic stroke, intracranial and cerebral tumors, multiple sclerosis. Associated with central paralysis is the development of Mijar-Gubler, Brissot, Fauville syndromes, pseudobulbar syndrome, oculosympathetic syndrome (Gorner syndrome), opercular syndrome (Foix-Chavany-Marie syndrome), and other alternating syndromes.
Central paresis of mimic muscles with their unilateral or bilateral weakness is observed in muscular dystrophy (including myotonic), in amyotrophic lateral sclerosis syndrome, Landouzi-Dejerine syndrome - progressive facioscapulo-shoulder muscular (shoulder-lapulo-facial) dystrophy (genetic skeletal-muscular disease).
Metabolic disorders of neuromuscular function of idiopathic or autoimmune nature are responsible for weakness of mimic muscles in myasthenia gravis, [2] hyperkalemic periodic paralysis (occurring in people with mutations of the gene for skeletal muscle sodium ion channels, through which neurons propagate their action potential due to the movement of ions). For more information, see the publication - bilateral weakness of mimic muscles
In lesions of the lower motoneurons or their peripheral axons, facial paralysis and/or paresis refers to loss of movement, decreased muscle tone, or weakness of the affected muscles due to damage or paralysis of the facial nerve - the main trunk and its branches. Also see. - facial nerve neuropathy left, right: acute, ischemic [3]
For example, acute facial nerve palsy and prosoplegia, a peripheral paralysis of the facial muscles, also known as bell's palsy, can occur at any age. It is essentially an idiopathic peripheral neuritis with unilateral weakness of the lower motoneurons of the facial muscles innervated by the temporal and zygomatic branches of the facial nerve. But a significant number of clinical cases incline specialists to the conclusion regarding the possible viral origin of this condition, in particular due to herpesvirus infection. [4], [5]
Paralysis or peripheral paresis of the mimic muscles is noted as a complication of infectious mononucleosis, the causative agent of which is human herpes virus type 4, more commonly known as Epstein-Barr virus.
And when herpes virus type 3 (varicella zoster virus) infects the patellar ganglion of the facial nerve located in the facial canal of the temporal bone, a rather rare neurological disease - Ramsay Hunt syndrome with paresis of mimic muscles on the side of the lesion and cochleovestibular disorders develops. More information in the material - herpetic and postherpetic ganglioneuritis
Possible causes of peripheral paralysis of the facial nerve and facial muscles include bacterial infection: middle ear inflammation - acute otitis media, as well as tick-borreliosis - lyme disease, in which the muscles are paralyzed not immediately, but several days or months after the bite of a tick carrying the spirochete Borrelia burgdorferi. [6]
Cranial nerve damage, including facial nerve damage with paralysis of part of mimic muscles, occurs in patients with Bezier-Beck-Schaumann disease (neurosarcoidosis), which is autoimmune in nature. Bilateral paralysis of the mimic muscles due to damage to the myelin sheath protecting the axons of cranial nerves is seen in cases of postinfectious autoimmune guillain-Barré syndrome, which is classified as a demyelinating polyneuropathy.
An epidermoid cyst compressing the facial nerve and its branches - cholesteatoma, paraganglioma of the temporal bone and parotid salivary gland neoplasms (adenoma, carcinoma, sarcoma) can lead to paralysis.
Risk factors
In addition to the above causative factors of mimic muscle paralysis/paresis, experts cite such risk factors for its development as:
- Viral infections, meningitis, tick-borne encephalitis, brain-affected syphilis;
- Facial neuralgia;
- Ischemic encephalopathy and ischemic nerve neuropathy;
- Brain tumors, including schwannomas and hemangiomas;
- Neurodegenerative diseases, particularly Steele-Richardson-Olszewski syndrome (progressive supranuclear palsy), frontotemporal dementia, and others;
- Muscle tone disorders of various etiologies;
- Diabetes;
- Damage to the facial nerve or its branches during surgical interventions, including tonsil and adenoidectomy, mastoidectomy, parotid salivary gland tumor removal, cervical-facial rhytidectomy (facelift), etc.;
- Poisoning with ethylene glycol, dichloromethane, organophosphorus compounds, carbon monoxide (carbon monoxide), arsenic, heavy metals;
- Long-term deficiency of cyanocobalamin - vitamin B12 in the body.
Pathogenesis
Dysfunction of at least one of the four dozen facial muscles is usually due to nerve damage, and mimic muscles - facial nerve (nervus facialis), whose motor and sensory fibers originate from the nucleus of the facial nerve (nucleus nervi facialis) in the ventral part of the pontomedullary junction (bridge) of the brainstem. The nerve passes through the posterior cranial fossa and then through the facial canal of the temporal bone (canalis facialis), where it forms the patellar ganglion (ganglion geniculi).
After the nerve leaves the canalis facialis, its extravisceral part begins; behind the parotid gland (through which the nerve also passes) there is a nerve plexus (plexus parotideus) with terminal branches (temporal, zygomatic, cheek, mandibular and cervical) coming out of it. Nerve impulses, which are carried along these branches, ensure the activation of motor neurons and the mobility of mimic muscles.
As a result of the inflammatory process, excessive compression and any other alteration affecting the facial nerve or its branches, increased capillary permeability, impaired blood and lymph flow, swelling of the surrounding tissues lead to deterioration of their trophism, which adversely affects the state of nerve fibers and the protective coating of the nerve - myelin sheath. As a result, the conduction of nerve signals deteriorates, and the pathogenesis of paralysis and paresis of the mimic muscles is due to disruption of neuromuscular transmission.
The mechanism of development of central paralysis of mimic muscles is associated with degenerative changes in the neurons of the basal nuclei and brainstem, as well as damage to the white (subcortical) matter of the cerebral hemispheres, which affects the corticobulbar, cortical-nuclear or pyramidal tract, responsible for the arbitrary control of skeletal muscles, whose movements are provided by upper motoneurons and efferent pyramidal fibers.
Symptoms of the paralysis and paresis of the facial muscles
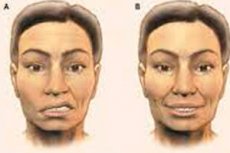
In paralysis/paresis of the mimic muscles, the first signs are most often manifested by unilateral facial misalignment: asymmetry of the nasolabial (nasolabial) folds and lowering of the corner of the mouth on the affected side.
Peripheral Bell's palsy usually has a sudden onset, often preceded by dysesthesia (discomfort on one side of the face) and paresthesia (sensory disturbance) on the same side, as well as neck stiffness and pain in the behind-the-ear area. Then, within a few hours, other symptoms begin to appear: headache, hyperacusis (hypersensitivity to sudden loud sounds), inability to close the eye, i.e. To close the eyelids (and when attempting to do so, the eye rolls behind the upper eyelid), indicating inactivity of the orbicularis oris muscle.
There is also a violation of parasympathetic functions in the form of epiphora (increased lacrimation, especially during eating), dysgeusia (distortion of taste sensations), increased salivation on one side of the mouth, which indicates a unilateral violation of the secretion of parotid and submandibular salivary glands.
Stroke develops central paralysis and affects the lower face with weakening and sagging of the cheek muscles (m. Buccinator), unilateral facial numbness and curvature of the mouth (due to damage to the circular perioral muscles) with dysarthria - impaired articulation (which makes speech unintelligible). Also read - paralysis after stroke
In case of changes in the excitability of denervated muscle fibers or abnormal activity of damaged lower brainstem motoneurons, as well as in amyotrophic lateral sclerosis, there are spasms of mimic muscles in the form of spontaneous twitching of individual fibers - fibrillations or fascializations.
Cochleovestibular symptoms in Ramsay Hunt syndrome are manifested by ringing in the ears, decreased hearing acuity, dizziness, problems with body balance, as well as involuntary eye movements, i.e. Violation of fixation of the eyeballs by the oculomotor muscles - nystagmus.
When central facial muscle paresis is combined with brainstem dysfunction, a contralateral paresis of the upper extremity may be observed.
Complications and consequences
Paresis and paralysis of the mimic muscles can have complications and consequences. In particular, the inability to close the eyelids on the affected side leads to xerophthalmia (dry eye) with a high likelihood of developing otophalmologic inflammatory diseases such as conjunctivitis or keratitis.
Prolonged denervation and immobilization of the affected facial muscles causes their degradation - muscle atrophy.
So-called post-paralytic contracture of facial mimic muscles can develop, for more information see. - neurogenic muscle contracture
If there are degenerative changes in the axons of the facial nerve in facial paralysis, the consequences will be manifested by synkinesia (involuntary movements of other muscles accompanying arbitrary ones), myokia (involuntary contractions of the eyelid muscle), and facial dyskinesia.
Diagnostics of the paralysis and paresis of the facial muscles
The diagnosis of peripheral paralysis of facial muscles and facial nerve is based on the presence of typical symptoms and signs detected by history taking and physical examination.
It is necessary to examine the cranial nerves. VII pair: facial nerve
Blood tests are taken: general clinical; for the level of lactate, lactate dehydrogenase, creatine phosphokinase, pyruvate, calcium (total and ionized), folic acid and vitamin B12; for monoclonal antibodies MAG, for antibodies to acetylcholinesterase, to herpes virus, for antibodies to autoantigens of myelin and others. Cerebrospinal fluid analysis is also required. [7]
The main methods by which instrumental diagnosis is performed include: cranial radiography, electroencephalography (EEG), electroneuromyography, nerve ultrasound, magnetic resonance and computed tomography of the brain. [8]
Differential diagnosis
The most important task to be solved by differential diagnosis is to determine the nature of paralysis/paresis of mimic muscles - peripheral or central, as well as to identify syndromal neurological conditions and conditions with loss of facial muscle tone, such as facial oromandibular dystonia. Postneuritic contracture of mimic muscles after neuritis (or neuralgia) of the facial nerve requires differentiation.
Who to contact?
Treatment of the paralysis and paresis of the facial muscles
In many cases, treatment of these neurological conditions is reduced to the use of systemic corticosteroids (Prednisolone - 80 mg per day for five days), immunomodulatory antiviral agents (with interferon), for example, avonex.
(interferon beta-1a) or b-immunoferon 1b (although their effectiveness is not yet well evidenced).
Other medications are used depending on the underlying diagnosis, for example, nootropic drugs; cholinomimetics Proserpine. Pyridostigmine. ubretide or Neostigmine. Preparations of α-lipoic (thioctic) acid with antioxidant properties - berlithion (Dialipon, Alpha-lipon) - are taken orally in the form of capsules (tablets). Possible side effects include allergic reactions, headache, taste disturbance, hot flushes and sweating, hypoglycemia, nausea and vomiting, abdominal pain, diarrhea.
Vitamin B12 (injections of 500-1000 mcg every other day) can have a positive effect. [9]
Potential improvement of the function of the facial nerve and mimic muscles gives physiotherapeutic treatment with the use of drug electrophoresis, magnetotherapy, with long-standing paresis - electrical stimulation of muscles, therapeutic massage, acupuncture. [10]
LFK is prescribed - orofacial exercises or gymnastics for mimic muscles in paresis and paralysis (mainly peripheral), which is aimed at stimulating the affected muscles, increasing muscle strength and restoring the coordination of their movements. It can be done independently - three or four times a day, repeating each exercise 25-30 times (sitting in front of a mirror):
- Opening and closing your mouth.
- Puff out your cheeks.
- Clenching and unclenching your lips.
- Stick out your tongue, pointing it toward your chin.
- Lift each corner of the mouth separately (you can use your fingers to lift the affected side).
- Raising and lowering the eyebrows (you can raise the eyebrow on the affected side with your fingers).
- Alternately open wide and then close your eyes.
- While trying to wrinkle your nose, use your fingers to gently push up the skin near the nose on the affected side.
- Take deep breaths through the nose with the nostrils dilated.
If residual weakness of mimic muscles persists for several months, surgical treatment may be applied by surgical decompression of the nerve (in the external opening of the canalis facialis); transfer of a branch of another nerve to this area - to reinnervate the affected muscle; transfer of the tendon of the temporalis muscle; creation of a static sling (transfer of a flap of fibrous tissue sheet from the inner surface of the thigh); eyebrow lift, etc. [11]
Prevention
To date, prevention of most alteration syndromes is not possible.
For stroke prevention, see. - how can I prevent ischemic stroke?
But to prevent the activation of lifelong herpesviruses affecting the ganglia of nerves will help to strengthen immunity.
Forecast
Bell's facial palsy is most often temporary and its prognosis is satisfactory, as 15% of patients have moderate weakness of facial muscles or irreversible nerve damage.
After treatment for neurosarcoidosis, almost 75% of patients recover completely, but some have periodic worsening of symptoms.
In general, paralyses and paresis of facial muscles do not go away without a trace, and in 50% of centrally paralyzed/paresis cases it is not possible to restore their normal function.
List of books and studies related to the study of paralysis and paresis of facial muscles
- "Facial Nerve Disorders and Diseases: Diagnosis and Management" - by Robert L. Van De Graaff, James Tysome (Year: 2016)
- "Facial Nerve Disorders: Diagnosis and Management" - by Kofi D. Boahene, Sam J. Marzo (Year: 2007)
- "Facial Paralysis: Rehabilitation Techniques" - by William M. DeMayo (Year: 2002)
- "Bell's Palsy - A Medical Dictionary, Bibliography, and Annotated Research Guide to Internet References" - by James N. Parker, Philip M. Parker. Parker (Year: 2004)
- "Facial Palsy: Management and Rehabilitation" - by D.J. Denny, T.J. Cawthorne (Year: 2002)
- "Facial Nerve: Clinical and Surgical Management" - by Barry M. Schaitkin, William H. Slattery (Year: 2007)
- "The Facial Nerve: May's Second Edition" - by William H. Slattery, Barry M. Schaitkin (Year: 2000)
- "Peripheral Facial Nerve Paralysis: A Comprehensive Guide to Diagnosis and Management" - by Tessa Hadlock (Year: 2017)
- "Facial Palsy and Facial Rehabilitation: A Practical Guide to the Management of Facial Nerve Disorders" - by Jonathan Cole (Year: 2011)
Literature
Gusev, E. I. Neurology: national guide: in 2 vol. / ed. By E. I. Gusev, A. N. Konovalov, V. I. Skvortsova. - 2nd ed. Moscow: GEOTAR-Media, 2021. - Т. 2.

