Holter monitoring
Last reviewed: 07.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Holter monitoring (or Holter) is an immediate technique used to continuously record a patient's electrocardiogram (ECG) over a period of time, usually 24 hours. It allows physicians to assess the heart's electrical activity in real time and detect various arrhythmias and abnormalities that may not be noticeable with standard short-term ECGs. [1]
Here are some key points about Holter monitoring:
- Purpose and Purpose: The purpose of Holter monitoring is to detect and record arrhythmias, irregular heart rhythms, and other cardiac abnormalities. This can be useful in diagnosing conditions such as atrial fibrillation, tachycardia, bradycardia, and other cardiac problems.
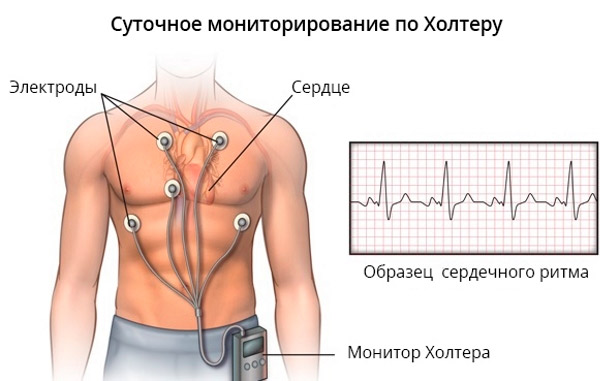
- Procedure: The patient is fitted with a small portable monitor that records an ECG. Electrodes are attached to the skin on the chest and connected to the monitor. The patient should lead a normal life during the monitoring period.
- Duration of monitoring: Monitoring is usually done for 24 hours, but longer options, such as 48 or 72 hours, may also be used.
- Results: After the monitoring is complete, the data is analyzed by a specialist (usually a cardiologist) who evaluates the ECG for abnormalities and arrhythmias. The results help the physician make an accurate diagnosis and decide whether to start treatment or correct existing treatment.
- Preparation: The patient does not require any special preparation before monitoring. However, it is important to keep records of physical activity, symptoms, and medication times during the monitoring period to allow for more accurate interpretation of the data.
Holter monitoring is a useful method for diagnosing cardiac arrhythmias and abnormalities that may not always show up in an inpatient setting. This test helps doctors to more accurately determine the condition of the heart and choose the appropriate treatment.
Indications for the procedure
Holter ECG monitoring is prescribed in the following cases:
- Diagnosis of cardiac arrhythmias: Holter monitoring is used to detect and diagnose various cardiac arrhythmias such as atrial fibrillation, atrial fibrillation, tachycardia, bradycardia and extrasystole.
- Assessing the cause of unclear symptoms: If a patient experiences symptoms such as dizziness, fainting, shortness of breath, chest pain or pressure, monitoring can help doctors identify electrical abnormalities of the heart that may be associated with these symptoms.
- Monitoringthe effectiveness of treatment: If heart arrhythmias or other heart problems are present, monitoring may be used to evaluate the effectiveness of treatment and adjust medication dosage.
- Evaluation of long-term arrhythmias: Holter monitoring allows arrhythmias to be recorded over long periods of time, usually 24 hours or more, which can be useful for detecting recurrent or random arrhythmias that might go undetected on short-term ECGs.
- Investigation of suspected coronaryheart disease: If coronary heart disease (narrowing of the coronary arteries) is suspected, Holter can be used to look for ischemic episodes (lack of blood supply to the heart muscle) and their association with arrhythmias.
- Monitoring after myocardial infarction: After myocardial infarction or other cardiac events, Holter monitoring can help in monitoring the patient's condition and detecting recurrence of arrhythmias.
- Investigation of rapid heartbeats: If a patient complains of frequent and irregular heartbeats (such as extrasystoles), monitoring can help physicians assess the nature and source of these contractions.
The approach to scheduling Holter monitoring depends on the patient's symptoms and clinical history. The physician decides when and for how long monitoring will be performed to obtain the most informative data for diagnosis and treatment of cardiac problems. [2]
Preparation
Here are some general guidelines for preparing for Holter monitoring:
- Medication information: Tell your doctor or health care provider about any medications you are taking. Some medicines may affect your monitoring results, and your doctor may decide if you need to temporarily stop taking any medicines.
- Maintain normalactivity: You are advised to maintain your normal lifestyle during monitoring. Try not to change your activity or lifestyle in order to record real-life heart data.
- Daily recordings: You will be given a portable monitor to carry with you during monitoring. Make sure the monitor is properly secured and follow the instructions of the medical staff regarding its use.
- Activity diary: You may need to keep an activity diary, recording the time and type of activity, your symptoms and how you feel. This can help your doctor associate events with ECG data.
- Avoid water and moisture: While wearing the monitor, try to avoid getting water on the monitor. This is usually warned when using the monitor.
- ElectrodeCare: If you are given instructions on how to care for the electrodes and where they are attached to the skin, follow them. This will help ensure a good ECG recording.
- Time adherence: It is important to return the monitor at the set time after the end of monitoring.
- Follow your doctor's recommendations: If you have any specific instructions from your doctor about preparing for and performing Holter monitoring, follow them exactly.
These guidelines may vary slightly depending on your physician's medical practice and instructions. It is important to discuss all questions and requirements with your physician or medical staff to ensure that the Holter monitoring procedure is performed correctly and accurate results are obtained. [3]
The device for carrying out the procedure
A special device called a Holter monitor is used to perform the Holter monitoring procedure. It is a portable electrocardiographic device that is worn by the patient for an extended period of time (usually 24 hours or more) and records the electrical activity of the heart during that period. These recordings are then analyzed by medical staff to detect abnormalities and arrhythmias. [4]
A Holter monitor typically consists of the following components:
- Monitor: This is a device worn by the patient. It is usually a small, portable device that can be attached to a belt or worn in a special case around the neck.
- Electrodes: Electrodes are small attachable skin electrodes that are placed on the patient's chest. They make contact with the skin and record the electrical activity of the heart.
- Wires: The wires connect the electrodes to the monitor. They carry signals from the electrodes to the monitor to record data.
- Battery: The monitor is usually powered by a battery that provides power to the device for the duration of the monitoring period.
- Display or control panel: Many modern Holter monitors have a display or control panel that allows patients to monitor the device and, if necessary, note cardiac events.
- Data Storage: Holter monitoring devices have built-in memory or means for storing recorded cardiac activity data.
Technique of the holter monitoring
The technique of Holter ECG monitoring includes the following steps:
-
Patient Preparation:
- The patient is explained how the monitor works and that he or she should lead a normal life during the monitoring.
- The skin in the chest area where the electrodes will be attached should be clean and dry. If the hair is long, it can be trimmed to better adhere the electrodes to the skin.
-
Attachment of electrodes:
- Medical personnel attach electrodes to the patient's skin. Usually 3 to 5 electrodes are used and placed at different locations on the chest and sometimes on the abdomen.
- The electrodes are connected to a small portable monitor that the patient must wear for a specified period of time (most often 24 hours).
-
Wearing a monitor:
- The patient should lead a normal lifestyle, including work, physical activity, and sleep, during monitoring. It is important to keep records of symptoms, physical activity, and time of medication.
- The monitor can be worn on your belt, around your neck, or in your pocket. It is important to avoid strong magnetic fields and exposure to water to prevent damage to the monitor.
-
Completion of monitoring:
- At the end of the specified monitoring period (most often 24 hours), the patient returns to the clinic or hospital where medical staff removes the electrodes and retrieves the data from the monitor.
- The data is then analyzed by a specialist (usually a cardiologist) who evaluates the ECG for arrhythmias and abnormalities.
The patient should follow the instructions of the medical staff and keep records of symptoms and activity during monitoring to ensure more accurate test results. [5]
Types of Holter monitoring
Depending on the purpose of monitoring and typical tasks, there are different types of Holter monitoring:
- Standard 24-hour monitoring: This is the most common type of Holter monitoring. The patient wears a small portable monitor with electrodes attached for 24 hours. During this time, heart activity during normal activities and sleep is recorded. This type of monitoring is used to detect a variety of arrhythmias and assess the electrical activity of the heart in different situations.
- 48-hour and 72-hour monitoring: In some cases, physicians may decide to extend monitoring to 48 or 72 hours for more detailed analysis. This may be useful in identifying rare or intermittent arrhythmias that might be missed with standard 24-hour monitoring.
- Event monitoring: This type of monitoring is used to record an ECG only at times when the patient experiences symptoms such as chest pain, fainting, or dizziness. The patient activates the monitor himself when symptoms occur. This helps identify arrhythmias associated with specific symptoms.
-
Daily blood pressure (BP) monitoring: The monitor worn by the patient during the day records not only the ECG but also the blood pressure. This allows the relationship between arrhythmias and changes in BP to be assessed.
The choice of Holter monitoring type depends on clinical goals, patient symptoms, and physician recommendations. Each type of monitoring has its advantages and limitations, and the physician decides which type of monitoring is most appropriate for a particular situation. [6]
Holter ECG monitoring in children
The use of Holter monitoring in children may be particularly useful in the following cases:
- Arrhythmias: If a child has symptoms of an arrhythmia, such as frequent or unusual heartbeats, Holter monitoring can help the doctor diagnose and determine the nature of the arrhythmia.
- Unexplained symptoms: If a child has unexplained heart-related symptoms such as dizziness, fainting, or feeling short of breath, Holter monitoring can help identify arrhythmias or changes that may be associated with these symptoms.
- Holtermonitoring: Sometimes Holter monitoring may be used to monitor the effectiveness of treatment for arrhythmias or heart problems in children.
The Holter monitoring procedure in children is similar to the procedure in adults. The child will have electrodes attached to the skin of the chest that will be connected to a portable monitor. The monitor will record heart activity data for a certain period of time, usually 24 hours or more. After the monitor is removed, the data will be analyzed by a doctor or cardiologist for diagnosis and to determine further treatment or monitoring.
It is important that the parent and child follow the instructions of the doctor or medical staff regarding the preparation and wearing of the monitor. If you have any questions or concerns, discuss them with your physician, who will be able to provide the necessary information and guidance. [7]
Contraindications to the procedure
Holter monitoring is a relatively safe procedure and usually has no serious contraindications. However, there are a few circumstances in which caution or alternative diagnostic methods may be necessary. Contraindications to Holter monitoring include:
- Severe allergy to electrode components: If the patient has a known allergy to the materials used for the electrodes, this may be a contraindication.
- Excessive skin damage to the area where the electrodes are to be attached: If the skin on the chest or other areas where the electrodes are to be attached has severe abrasions, burns, or infections, monitoring may be difficult or cause additional discomfort.
- Psychologic problems: Patients with serious psychological or neurologic problems that may pose a danger to themselves or others (e.g., tendency to tear or damage the monitor) may require special caution or alternative monitoring methods.
- Inability to follow instructions: If the patient is unable to follow instructions and is unable to wear the monitor or record symptoms and activity during monitoring, it may make it difficult to interpret the data.
The physician should always assess the patient and consider their individual circumstances before performing Holter monitoring. If there are doubts or concerns, the physician may consider alternative diagnostic methods to obtain the necessary information about the patient's heart condition. [8]
Normal performance
Normal Holter monitoring (ECG-Holter) values may vary depending on the patient's age, gender, and general condition. The readings may be different for adults and children. A physician or cardiologist will usually interpret Holter monitoring results based on individual patient characteristics and clinical context.
However, in general terms, normal Holter monitoring values include the following:
- Heart Rhythm: The normal heart rate in adults is usually 60-100 beats per minute at rest. In children and adolescents, the normal heart rate may be higher.
- Cardiac arrhythmias: Only physiologic arrhythmias such as nocturnal bradycardia (slowing of the heart rate) and sinus arrhythmia (normal variability in the RR interval between heart beats) can be detected normally.
- Segments and intervals: ECG recordings should reflect normal values for the PR, QRS and QT intervals; changes in these may indicate cardiac conduction problems.
- ST segment: ST segment changes may indicate myocardial ischemia (insufficient blood supply).
- Arrhythmias: Holter monitoring can also detect different types of arrhythmias, such as ventricular or atrial extrasystole.
It is important to understand that interpreting Holter monitoring results requires specialized knowledge and experience, and only a physician or cardiologist can make a definitive diagnosis and recommendations based on these data. If you have questions or concerns about Holter monitoring results, discuss them with your physician for more information and counseling.
Evaluation and interpretation of Holter monitoring
Evaluation and interpretation of Holter monitoring (ECG) data is performed by a physician with specialized skills in analyzing cardiac activity. Such evaluation includes the following aspects:
- Heart rhythm analysis: The doctor analyzes the heart rhythm and identifies the presence of arrhythmias such as atrial fibrillation, atrial fibrillation, tachycardia, bradycardia, extrasystole, and others. It is important to determine if there are any abnormalities or inconsistencies in the rhythm.
- Examining segments and intervals: The doctor also analyzes segments and intervals on the ECG, such as the PQ interval (PR), QRS interval, and QT interval. Changes in these parameters may indicate problems with the conduction of impulses in the heart.
- Heart rate count: The doctor determines the average heart rate (pulse) over the monitoring period and assesses whether there are fluctuations in the rate at different times of the day and night.
- Analysis of rhythm pauses: Holter monitoring records pauses between heartbeats. Normally, pauses in the heart rhythm may be short and may not cause any symptoms. However, the doctor pays attention to long or unusual pauses because they may indicate heart abnormalities.
- Relationship to symptoms: It is also important to establish the relationship between the reported arrhythmias and the symptoms reported by the patient (e.g., chest pain, dizziness, or fainting).
Regarding pauses in Holter monitoring, normal pauses between heartbeats can vary and their duration depends on the age and physiologic characteristics of the patient. Usually short pauses (up to a few seconds) may be normal and not cause concern.
However, if monitoring reveals long pauses in heart rhythm, especially if accompanied by symptoms such as fainting or dizziness, this may require further attention and evaluation by a physician. Prolonged pauses may be associated with impulse conduction abnormalities in the heart and may require additional testing and treatment.
It is important to remember that only a doctor is able to correctly assess the results of Holter monitoring and give recommendations for further treatment and follow-up.
Complications after the procedure
Holter monitoring (ECG) is a relatively safe procedure and complications are rare. However, in rare cases, the following complications may occur:
- Irritation or allergic reaction to electrodes: Some patients may experience skin irritation or allergic reaction to the materials used to attach the electrodes. This may manifest as itching, redness or rashes. In such cases, it is important to seek prompt medical attention to evaluate and correct the problem.
- Discomfort while wearing the monitor: Some patients may experience discomfort or discomfort when wearing the monitor for long periods of time. This may include a feeling of heaviness, itching, or discomfort on the skin. These symptoms usually disappear when the monitor is removed.
- Electrode Damage: In rare cases, electrodes may come off or be damaged during monitoring. This may result in incorrect data collection and may require a repeat procedure.
- Monitor failure or data loss: Although modern monitors are generally reliable, sometimes equipment failure or data loss may occur. This may require re-monitoring.
- Psychological discomfort: Some patients may experience psychological discomfort associated with wearing a monitor, especially during the night. This can cause insomnia or additional stress.
In general, complications from Holter monitoring are extremely rare, and most patients tolerate the procedure without any problems. It is important to inform your doctor of any unusual symptoms or problems that might occur during or after monitoring so that you can get appropriate help and advice.
Care after the procedure
There are no special restrictions or care requirements after a Holter monitoring (ECG-Holter) procedure. However, there are some general guidelines that may help you after the monitor is removed:
- Removing the electrodes: After the treatment is complete, remove the electrodes from the skin. This can be done gently to avoid skin irritation. If there are residues of electrode adhesive left on the skin, they can be removed using a mild oil or special adhesive remover.
- Skin care: Check the skin where the electrodes have been attached. In some cases, there may be slight irritation or redness. If you have irritations, you can use a mild cream or lotion to soothe the skin.
- Maintain normal activity: Once the monitor is removed, you can return to normal activity. There is no need to restrict physical activity.
- Informing your doctor: After the procedure, the Holter monitoring results will be analyzed by your doctor or cardiologist. After receiving the results, your doctor may provide you with feedback and recommendations based on the data obtained during the monitoring.
- Compliance with recommendations: If your doctor has given you any recommendations or prescribed treatment based on Holter monitoring results, follow these instructions. This may include taking medications or making lifestyle changes.
- Data storage: Holter monitoring data is usually stored electronically. If you have access to this data, save it or discuss the results with your doctor at your appointment.
Clinical recommendations for Holter monitoring
May vary depending on the specific clinical situation and study objectives. However, there are general guidelines for different scenarios of Holter monitoring use:
- Arrhythmia diagnosis: Holter monitoring is often used to detect and classify cardiac arrhythmias. This may include analyzing the type of arrhythmia, duration, frequency, and its relationship to the patient's symptoms. Holter monitoring is recommended if arrhythmias such as atrial fibrillation or atrial fibrillation are suspected.
- Evaluating Treatment Effectiveness: After starting treatment for arrhythmias or other heart conditions, doctors may recommend Holter monitoring to evaluate the effectiveness of treatment and determine if symptoms and arrhythmias have decreased.
- Identifying symptoms: If a patient experiences symptoms such as chest pain, dizziness, or fainting that may be related to heart problems, doctors may recommend Holter monitoring to record them and analyze them later.
- Cardiac monitoring throughout the day: In some cases, especially if nocturnal arrhythmias or changes in cardiac activity at different times of the day are suspected, monitoring may be recommended to obtain information on heart rate and rhythm for 24 hours or more.
- Tracking monitoring: Patients with previously diagnosed arrhythmias or other cardiac problems may be recommended regular tracking monitoring for long-term follow-up of heart health and treatment effectiveness.
The decision to perform Holter monitoring and its duration should be made by the physician based on the patient's specific clinical symptoms and history. It is also important to follow the physician's instructions regarding preparation for monitoring and wearing the monitor for the specified period of time.
What should not be done during Holter monitoring?
Holter monitoring is a procedure that usually has no severe limitations in the patient's normal daily activities. However, there are some recommendations on what should be avoided or taken into account during monitoring to ensure accurate data:
- Moistureand keeping the monitor dry: Try to avoid exposing the monitor to water, as moisture can damage the device. If you take a shower, be sure to keep the monitor dry or use a special bag to protect it from moisture.
- Avoid electromagnetic sources: Strong electromagnetic fields, such as from powerful magnets or magnetic resonance imaging (MRI) equipment, can affect the performance of the monitor. If you are scheduled to have an MRI, tell your doctor and medical staff in advance.
- Avoid cross signals: Some devices, such as cordless phones or metal detectors, may create interference with the monitor. Avoid close contact with such devices.
- Wear the monitor correctly: Make sure the monitor is properly attached to your body so that it securely attaches the electrodes to your skin.
- Pay attention to notes: If you experience heart-related symptoms (e.g., chest pain, palpitations, dizziness), try to make notes about the timing and nature of these symptoms in a journal, if provided.
- Follow yourdoctor's recommendations: If your doctor has given you any instructions or recommendations about monitoring, follow them exactly.
It is important to realize that Holter monitoring is designed to record the electrical activity of the heart in the real conditions of daily life. Therefore, try to maintain a normal lifestyle and activity pattern to get the most accurate results. If you have any specific questions or concerns, discuss them with your doctor before your Holter monitoring procedure.
Literature used
Axelrod A.S., Chomakhidze P.Sh., Syrkin A.L. - Holter ECG monitoring: opportunities, difficulties, errors. 2010
Holter monitoring. 4th ed. Makarov L.M. 2016

