Fibrous osteodysplasia
Last reviewed: 12.03.2022

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Bone dysplasia, Liechtenstein-Britzev disease, fibrous osteodysplasia - all these are names for the same congenital non-hereditary pathology, in which bone tissue is replaced by fibrous tissue. Patients have bone curvature - mainly in childhood and adolescence. Almost any of the skeletal bones can be damaged, but the bones of the skull, ribs and long tubular bones (metaphyseal and diaphyseal parts, without involving the epiphysis) are most often affected. Multiple lesions are often associated with McCune-Albright syndrome. Clinical symptoms depend on which bones are affected and to what extent. Treatment is mainly surgical.
Epidemiology
Cases of fibrous osteodysplasia account for approximately 5% of all benign bone pathologies. However, there is no clear data on the true incidence rate, since the disease is often asymptomatic (in about 40% of cases, patients do not present any complaints). At the same time, localized fibrous osteodysplasia is spoken about in approximately 78% of cases.
The course of fibrous osteodysplasia is slow, progressive, manifesting itself mainly during increased bone growth. That is why pathology is more often found in adolescents aged 13-15 years (30% of the examined patients). However, it happens that the problem is first detected in old age. If the disease simultaneously affects several bones (and this happens in about 23% of cases), then the anomaly can be detected much earlier - in patients of preschool and school age.
Almost half of the patients, along with fibrous osteodysplasia, also have other diseases of the musculoskeletal system.
Not all patients have obvious symptoms of the disease. The risk of manifestation of pathology increases during puberty, in women - during pregnancy, as well as when exposed to harmful external and internal factors.
Both females and males get sick equally (according to other sources, girls get sick a little more often, in a ratio of 1: 1.4).
The most commonly observed lesions are the femur (47%), the bones of the lower leg (37%), the bones of the shoulder (12%) and the forearm (2%). Fibrous osteodysplasia can appear with the same frequency, both on the left and on the right. The polyostotic type of pathology often extends to the bones of the skull, pelvis, and also to the ribs (25% of cases).
Causes of the fibrous osteodysplasia
Fibrous osteodysplasia is a systemic skeletal bone disease that is congenital but not hereditary. The processes of dysplasia resemble the formation of a tumor, while not being a real tumor process. Pathology appears as a result of a violation of the development of the progenitor of bone tissue - skeletal mesenchyme.
The first description of fibrous osteodysplasia took place at the beginning of the 20th century by the Russian doctor Braitsov. Subsequently, information about the disease was supplemented by the American endocrinologist Albright, orthopedic doctor Albrecht and other specialists (in particular, Lichtenstein and Jaffe).
In medicine, these types of pathology are divided:
- monoosseous (when one bone of the skeleton is affected);
- polyosseous (when two or more bones of the skeleton are affected).
The first pathological type can first appear at almost any age, usually not accompanied by hyperpigmentation and disruption of the endocrine system.
The second pathological type is found in pediatric patients and usually occurs in the form of Albright's syndrome.
Most often, specialists use the following clinicopathological classification of fibrous osteodysplasia:
- Intraosseous lesion, with the formation of single or numerous fibrous foci inside the bone. Less often, the entire bone is affected, with structural preservation of the cortical layer and the absence of curvature.
- Total osteodysplasia, involving all segments in the process, including the cortical layer and the zone of the bone marrow cavity. The lesion is accompanied by bone curvature, pathological fractures. Mostly long tubular bones are damaged.
- Tumor lesion is characterized by focal spread of fibrosis. Such growths often differ in pronounced size.
- Albright's syndrome is manifested by multiple bone pathology against the background of endocrine disorders, early onset of puberty, incorrect body proportions, skin hyperpigmentation, and pronounced bone curvatures.
- Fibrocartilaginous lesions are accompanied by the transformation of cartilage tissue, which is often complicated by the development of chondrosarcoma.
- A calcifying lesion is characteristic of fibrous osteodysplasia of the tibia.
Risk factors
Since fibrous osteodysplasia is not a hereditary disease, intrauterine disorders in the laying of tissues from which the bone skeleton develops are considered as causative factors.
Perhaps the causes can be various pathologies of pregnancy - in particular, vitamin deficiency, endocrine disorders, as well as environmental factors such as radiation, infectious effects.
In general, risk factors are described as follows:
- toxicosis in a woman in the first half of pregnancy;
- viral and microbial infections in a woman up to the 15th week of pregnancy;
- unfavorable ecological situation;
- vitamin deficiency (vitamins B and E), as well as a lack of iron, calcium, iodine.
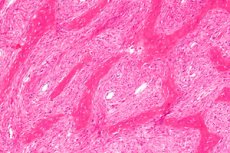
Pathogenesis
The development of fibrous osteodysplasia is due to a change in the DNA sequence of somatic cells in the GNAS1 gene located on chromosome 20q13.2-13.3. This gene is responsible for encoding the α-subunit of the activating protein G. As a result of mutational changes, the amino acid arginine R201 is replaced by the amino acid cysteine R201C or histidine R201H. Under the influence of an abnormal type of protein, G1 cyclic AMP (adenosine monophosphate) and osteoblast cells are activated to accelerate DNA production, which is different from the norm. As a result, fibrous unorganized bone matrix tissue and primitive bone tissue are formed, devoid of the property of maturation into a lamellar structure. Pathological changes also affect mineralizing processes. [1]
Skeletal stem cells that carry this mutation have an impaired ability to differentiate into mature osteoblasts and instead retain a fibroblast-like phenotype. [2]The mutant cells [3] proliferate and replace normal bone and marrow, typically with demineralized and structurally immature fibro-osseous tissue. [4], [5]
The basic pathogenetic characteristics of the development of fibrous osteodysplasia also include the formation and growth of cysts due to a local disorder of the venous outflow in the bone metaphysis. The pathological process leads to an increase in intraosseous pressure, a change in the cellular composition of the blood, the removal of lysosome enzymes that affect the bone tissue and provoke its lysis. At the same time, the coagulation process is disturbed, local fibrinolysis is noted. The accumulation of decomposition products of the bone matrix causes an increase in oncotic pressure inside the cystic formation. A pathological cycle of mutual reinforcement of disorders is formed.
Symptoms of the fibrous osteodysplasia
Fibrous osteodysplasia often manifests itself in early childhood and adolescence. The humerus, ulna, radius, femur, tibia, fibula are predominantly affected.
The initial stage of the disease is not accompanied by any severe symptoms, sometimes there are slight pulling pains. [6]In many patients, [7] the first "bell" is manifested by a pathological fracture. In general, early signs are often absent or go unnoticed.
When probing, pain is usually not observed: pain is more characteristic of significant physical exertion. If the pathological process affects the proximal femoral diaphysis, the patient may experience lameness, and with pathology of the shoulder bone, the patient may notice discomfort during a sharp swing and lifting of the limb. [8], [9]
The clinical picture of fibrous osteodysplasia is not always found in children, since in many patients congenital anomalies and curvatures are most often absent. But the polyosseous type of pathology manifests itself precisely in young children. Bone disorders are combined with endocrinopathy, skin hyperpigmentation, disorders of the cardiovascular apparatus. Symptoms of the disease can be diverse and diverse. In this case, the main symptom is pain against the background of increasing deformity.
In many patients, the diagnosis of fibrous osteodysplasia is made after the discovery of a pathological fracture.
The severity of bone curvature depends on the location of the pathological lesion. If the tubular bones of the hands are affected, their club-shaped increase is possible. If the finger phalanges are affected, then their shortening, "chopping" is observed.
Complications and consequences
The most common consequences of fibrous osteodysplasia are pain and progressive deformities of individual bones and limbs, as well as pathological fractures.
The bones of the legs are often deformed due to the pressure of body weight, typical curvatures appear. The most pronounced is the curvature of the femur, which in some cases is shortened by several centimeters. With a deformity of the femoral neck, a person begins to limp.
With fibrous osteodysplasia of the ischium and ilium, the pelvic ring is bent, which causes corresponding complications from the spinal column. Kyphosis or kyphoscoliosis is formed. [10]
Monoosseous dysplasia is considered more favorable in terms of prognosis, although the risk of pathological fractures is present.
Malignant degeneration of fibrous osteodysplasia is rare, but it should not be completely ruled out. It is possible to develop such tumor processes as osteosarcoma, fibrosarcoma, chondrosarcoma, malignant fibrous histiocytoma.
Diagnostics of the fibrous osteodysplasia
Diagnosis is carried out by an orthopedic specialist, based on the characteristics of clinical manifestations and information obtained in the course of instrumental and laboratory diagnostics.
Without fail, the traumatological and orthopedic status is studied, the dimensions of the affected and healthy limbs are measured, the amplitude latitude of articular movements (active and passive) and the condition of soft tissue structures are assessed, indicators of curvature and cicatricial changes are determined.
An orthopedic examination consists of the following steps:
- external examination of the affected area, detection of redness, swelling, muscle atrophy, skin damage, ulcerative processes, curvature, shortening of the bone;
- palpation of the affected area, detection of seals, tissue softening, fluctuating elements, palpation pain, excessive mobility;
- taking measurements, detecting latent edema, muscle atrophy, changing the length of the bone;
- volumetric measurements of articular movements, identification of joint diseases.
Thanks to an external examination, a doctor can suspect a particular disease or injury, note its localization and prevalence, and describe pathological signs. After that, the patient is assigned laboratory tests.
Analyzes may include clinical, biochemical blood tests, coagulogram, urinalysis, assessment of immune status. The leukocyte formula, the level of total protein, albumin, urea, creatinine, alanine aminotransferase, aspartate aminotransferase are necessarily determined, the electrolytic composition of the blood is examined, histology of biopsy specimens and punctates is carried out. If indicated, genetic studies are prescribed.
Instrumental diagnostics is necessarily represented by radiography (lateral and direct). Sometimes oblique projections with a rotation angle of 30 to 40 degrees are additionally prescribed to determine the deformation characteristics.
In many cases, computed tomography of the damaged bone is recommended. This allows you to specify the location and size of defects.
Magnetic resonance imaging helps to assess the condition of surrounding tissues, and ultrasound examination of the extremities determines vascular disorders.
Radionuclide technique - biphasic scintigraphy - is necessary to identify affected lesions that are not visualized with conventional radiography, as well as to assess the extent of the operation.
X-ray is considered a mandatory diagnostic technique for patients with suspected fibrous osteodysplasia, as it helps to identify the stage of pathology. For example, at the stage of osteolysis, the image shows an unstructured sparse metaphysis touching the growth zone. At the stage of differentiation, the picture shows a cellular cavity with a dense-walled environment, separated from the growth zone by a part of healthy bone tissue. At the stage of restoration, the image shows an area of compacted bone tissue, or a small residual cavity formation. In patients with fibrous osteodysplasia, the normal metaphyseal image is replaced by a zone of enlightenment: such a zone is localized longitudinally, sharpens towards the bone center and expands towards the growth disc. It is characterized by uneven, fan-shaped shading of the bone septa towards the epiphyses.
X-rays are always performed in different projections, which is necessary to clarify the distribution of fibrous areas.
A nonspecific radiological sign is a periosteal reaction, or periostitis (periostosis). The periosteal reaction in fibrous osteodysplasia is the response of the periosteum to the action of an irritating factor. The periosteum is not detected on the x-ray: the reaction occurs only in the case of ossification of the periosteal layers.
Differential diagnosis
Differential diagnosis of osteoarticular diseases is multifaceted and quite complex. According to clinical and diagnostic recommendations, it is considered appropriate to use a multiple approach, using information obtained as a result of radiography, computed tomography, magnetic resonance imaging, and ultrasound. If possible, all available methods of radiation diagnostics should be used:
- polypositional, comparative radiography;
- bone mode with computed tomography, etc.
Fibrous osteodysplasia should be distinguished from such pathologies:
- osteofibrous dysplasia (ossifying fibroma);
- parosteal osteosarcoma;
- giant cell reparative bone granuloma;
- Paget's disease;
- well-differentiated central osteosarcoma. [11]
Who to contact?
Treatment of the fibrous osteodysplasia
Medical therapy for patients with fibrous osteodysplasia is practically ineffective. Quite often there are relapses of the disease, as well as the increasing dynamics of curvature and changes in the length of the bones. [12]
A positive effect of puncture therapy in the development of cystic formations was noted, but such treatment does not solve the general problem, which is associated with severe deformities and changes in the length of the bone.
Thus, the only sure way to stop fibrous osteodysplasia is surgical intervention, which is recommended for patients with tubular bone dysplasia with underlying deformities.
In the absence of deformation of the bone diaphysis and the presence of 50-70% damage to the bone diameter, an intralesional resection is performed. The intervention is performed taking into account the information obtained during computed tomography and radioisotope diagnostics. The defect is replaced with longitudinally split cortical grafts. In case of severe damage to the bone diameter (more than 75%), it is recommended to perform a radical removal of the altered tissues. [13] The defect is replaced with cortical grafts, simultaneously using different types of osteosynthesis:
- metal osteosynthesis with the use of external fixation devices is recommended for patients with deformities of the femur and the transition of the pathological process to the trochanter and segmental neck;
- metal osteosynthesis using straight periosteal plates is recommended for patients with tibial curvature.
The operation of osteosynthesis is planned and may have its own contraindications:
- acute course of infectious and inflammatory pathologies;
- exacerbation of chronic pathologies;
- states of decompensation;
- psychopathology;
- dermatopathologies affecting the area affected by fibrous osteodysplasia.
The essence of the surgical intervention is a complete segmental resection of the damaged bone tissue and the installation of a bone implant. In the presence of a pathological fracture, a transosseous compression-distraction Ilizarov apparatus is used.
In case of polyostotic lesions, it is recommended to start surgical intervention as early as possible, without waiting for the appearance of curvature of the damaged bones. In this situation, we can talk about a preventive (preventive) operation, which is technically easier, and also has a milder rehabilitation period.
Cortical grafts can resist dysplasia for a long period of time, and, together with bone fixation devices, help prevent re-deformation of the operated limb and prevent the occurrence of a pathological fracture.
Operated patients with fibrous osteodysplasia need systematic dynamic monitoring by an orthopedic doctor, since the disease tends to re-exacerbate. With the development of recurrence of osteodysplasia, a second operation is usually prescribed. [14]
The postoperative recovery period is long. It includes exercise therapy to prevent the appearance of contractures, as well as spa treatment.
Prevention
There is no specific prevention of the development of fibrous dysplasia, which is associated with an insufficiently understood etiology of the disorder.
Preventive measures consist in adequate management of pregnancy and the implementation of the following recommendations:
- optimization of a woman's nutrition throughout the childbearing period, ensuring the necessary intake of trace elements and vitamins;
- exclusion of alcohol and tobacco use;
- prevention of the negative effects of teratogenic substances (heavy metal salts, insecticides, pesticides and some medicines);
- improving somatic women's health (maintaining normal body weight, preventing diabetes, etc.);
- prevention of intrauterine infections.
After the birth of a child, it is important to think in advance about the prevention of both fibrous osteodysplasia and pathologies of the musculoskeletal mechanism in general. Doctors suggest using the following recommendations:
- monitor your weight;
- be physically active and meanwhile, do not overload the musculoskeletal system;
- avoid constant excessive stress on the bones and joints;
- ensure adequate intake of vitamins and minerals in the body;
- give up smoking and alcohol abuse.
In addition, it is necessary to timely seek medical help for injuries and pathologies from the musculoskeletal system. Injury management should be complete, and treatment should not be completed on one's own without medical advice. It is important to regularly undergo medical examinations - especially if a person is at risk or experiences discomfort in the bones, joints, and spinal column.
Forecast
The prognosis for the life of patients with fibrous osteodysplasia is favorable. However, in the absence of treatment, or with inadequate therapeutic measures (especially with polyostotic lesions), there is a risk of developing gross curvatures leading to disability. In some patients, fibrous osteodysplasia leads to the fact that dysplastic foci are transformed into benign and malignant tumor processes - for example, there have been fixed cases of giant cell neoplasm, osteogenic sarcoma, and non-ossifying fibroma.
Fibrous osteodysplasia tends to recur frequently. Therefore, it is very important that the patient, even after the surgical intervention, be under the constant supervision of orthopedic specialists. Formation of new pathological foci, lysis of allografts, pathological fractures are not excluded.

