Malignant tumors of the eyelids
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

In the 60-70s of the XX century. In ophthalmology was allocated an independent clinical direction - ophthalmo oncology, which should solve the problems of diagnosis and treatment of tumors of the organ of vision. Tumors of this localization are characterized by large polymorphism, the unique nature of the clinical and biological course. Diagnosis of them is difficult, for its implementation requires a set of instrumental research methods, which are owned by ophthalmologists. Along with this, knowledge is needed on the application of diagnostic measures used in general oncology. Significant difficulties arise in the treatment of eye tumors, its adnexa and orbit, since a small number of important anatomical structures are concentrated in small volumes of the eye and orbit, which complicates the implementation of therapeutic measures with preservation of visual functions.
Epidemiology
The annual incidence of tumors in the organ of vision for the treatment of patients is 100-120 per 1 million of the population. The incidence among children reaches 10-12% of the rates set for the adult population. Taking into account the localization, tumors of the adnexa of the eye (eyelids, conjunctiva), intraocular (vascular membrane and retina) and orbits are isolated. They differ in histogenesis, clinical course, professional and life prediction.
Among the primary tumors, the first place in frequency is occupied by tumors of the adnexa of the eye, the second by the intraocular and the third by the tumors of the orbit.
Tumors of the skin of the eyelids account for more than 80% of all neoplasms of the organ of vision. Age of patients from 1 year to 80 years and more. Prevalent tumors of epithelial genesis (up to 67%).
Causes of the malignant tumors of the eyelids
Malignant tumors of the eyelids are mainly represented by skin cancer and meibomian adenocarcinoma. In the development play the role of excessive ultraviolet irradiation, especially in persons with sensitive skin, the presence of non-healing ulcerative lesions or the influence of human papillomatous virus.
Symptoms of the malignant tumors of the eyelids
Basal cell carcinoma of the eyelids
Basal cell carcinoma of the eyelid is 72-90% among malignant epithelial tumors. Up to 95% of cases of its development occur at the age of 40-80 years. The preferred localization of the tumor is the lower eyelid and the internal adhesion of the eyelids. Isolate nodal, erosive-ulcerative and scleroderm-like forms of cancer.
Clinical signs depend on the shape of the tumor. With the nodular form, the boundaries of the tumor are sufficiently clear; it grows over the years, as the size increases in the center of the node, a crater-like appendage appears, sometimes covered with a dry or bloody crust, after removal of which a wet, painless surface is exposed; margins of ulcers are callous.

With a corrosive-ulcerative form, at first appears a small, almost unnoticeable, painless sore with raised edges in the form of a shaft. Gradually, the area of the ulcer increases, it is covered with a dry or bloody crust, it bleeds easily. After removing the crust, a coarse defect is exposed, along the edges of which there are bumpy growths. The ulcer is more often localized near the marginal edge of the eyelid, capturing its entire thickness.
Scleroderm-like form in the initial stage is represented by erythema with a wet surface covered with yellowish scales. During the growth of the tumor, the central part of the wetting surface is replaced by a fairly dense whitish rumen, and the progressive edge extends to healthy tissues.
 [17]
[17]
Scaly-cell cancer of the eyelids
Scaly-cell cancer of the eyelids is 15-18% of all malignant tumors of the eyelids. Mostly elderly people with insolation sensitive skin are affected.
Predicting factors are pigment xeroderma, oculocutaneous albinism, chronic skin diseases of the eyelids, long-term healing ulcers, excessive ultraviolet irradiation.
In the initial stage, the tumor is represented by a mild erythema of the skin, often the lower eyelid. Gradually, in the erythema zone, there is a condensation with hyperkeratosis on the surface. Around the tumor appears perifocal dermatitis, develops conjunctivitis. The tumor grows for 1-2 years. Gradually, in the center of the node a depression is formed with an ulcerated surface, the area of which gradually increases. The edges of the ulcers are dense, tuberous. When localized at the edge of the eyelids, the tumor quickly spreads into the orbit.

Treatment of cancer of the eyelids is planned after obtaining the results of a histological examination of the material obtained from tumor biopsy. Surgical treatment is possible with a tumor diameter of not more than 10 mm. The use of microsurgical techniques, laser or radiosurgical scalpel increases the effectiveness of treatment. Contact radiation therapy (brachytherapy) or cryodestruction can be carried out. When the tumor is localized in the vicinity of the intermarginal space, only external irradiation or photodynamic therapy can be performed. In the case of tumor growth, the conjunctiva or the orbit shows the subperiosteal exenteration of the tumor.
With timely treatment, 95% of patients live more than 5 years.
Adenocarcinoma of the meibomian gland (cartilage gland age)
Adenocarcinoma of the meibomian gland (cartilage gland age) is less than 1% of all malignant tumors of the eyelids. Usually the tumor is diagnosed in the fifth decade of life, more often in women. The tumor is located under the skin, usually the upper eyelid in the form of a node with a yellowish tinge, reminiscent of chalazion, which recurs after removal or begins to grow aggressively after drug treatment and physiotherapy.
After the removal of the chalazion, histological examination of the capsule is mandatory.
Adenocarcinoma can be manifested by blepharoconjunctivitis and meibomitis, grows rapidly, extends to cartilage, palpebral conjunctiva and its arches, tear ducts and nasal cavity. Given the aggressive nature of tumor growth, surgical treatment is not indicated. For tumors of small size, limited to the tissues of the eyelids, external irradiation can be used.
In case of appearance of metastases in regional lymph nodes (parotid, submaxillary), their irradiation should be carried out. The presence of signs of the spread of the tumor to the conjunctiva and its vaults necessitates the exenteration of the orbit. The tumor is characterized by extreme malignancy. In 2-10 years after radiation therapy or surgical treatment relapses occur in 90% of patients. From distant metastases within 5 years 50-67% of patients die.
Melanoma of the eyelids
Melanoma of the eyelids is not more than 1% of all malignant tumors of the eyelids. The peak incidence falls on the age of 40-70 years. Women are more often ill. Risk factors for the development of melanoma are identified: nevi, especially borderline, melanosis, individual hypersensitivity to intense sun radiation. It is believed that in the development of melanoma skin sunburn is more dangerous than with basal cell carcinoma. Risk factors are also unfavorable family history, age over 20 years and white skin color. The tumor develops from transformed intracutaneous melanocytes.
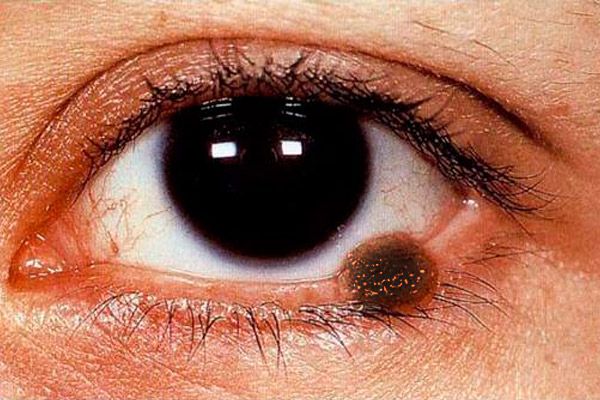
The clinical picture of the melanoma of the eyelids is polysymptomatic. Melanoma of the eyelids can be represented by a flat lesion with uneven and indistinct edges of light brown color, over the surface - nest more intense pigmentation.
The nodular form of melanoma (more often observed with skin localization on the eyelids) is characterized by a marked proneness over the skin surface, there is no skin pattern in this zone, the pigmentation is more pronounced. The tumor rapidly increases, its surface is easily ulcerated, spontaneous bleeding is observed. Even with the lightest touch of a gauze pad or cotton swab, a dark pigment remains on the surface of such a tumor. Around the tumor, the skin is hyperemic as a result of the expansion of the perifocal vessels, the whisk of the sprayed pigment is visible. Melanoma early spreads to the lining of the eyelids, teardrop, conjunctiva and its arches, into orbital tissues. The tumor metastasizes into regional lymph nodes, skin, liver and lungs.
Treatment of the melanoma of the eyelids should be planned only after a complete examination of the patient in order to detect metastases. In melanomas with a maximum diameter of less than 10 mm and the absence of metastases, it can be surgically excised using a laser scalpel, a radial scalpel or an electron knife with mandatory cryomixing of the tumor. Remove the focus of the lesion through, retracting at least 3 mm from the visible (under the operating microscope) boundaries. Cryodestruction in melanomas is contraindicated. Nodal tumors with a diameter of more than 15 mm with the corolla of dilated vessels are not subject to local excision, as in this phase, as a rule, metastases are already observed. Radiation therapy using a narrow medical proton beam is an alternative to the exenteration of the orbit. Regional lymph nodes should also be irradiated.
The prognosis for life is very difficult and depends on the depth of spread of the tumor. With the nodal form, the prognosis is worse, since early infection with tumor cells of tissues along the vertical occurs. The prognosis worsens in the spread of melanoma to the costal edge of the century, intermarginal space and conjunctiva.
What do need to examine?
How to examine?
Who to contact?

