Allergic vasculitis - causes, symptoms and treatment
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Allergic vasculitis is an inflammatory process of the walls of blood vessels, resulting from an allergic reaction. Allergic vasculitis is characterized by the predominant involvement of small-caliber blood vessels in the pathological process. Both men and women are subject to it, regardless of age.
Predisposing factors for allergic vasculitis are:
- Disorders of metabolic processes:
- overweight,
- the presence of diabetes
- gout,
- atherosclerosis.
- Diseases of autoimmune nature:
- systemic lupus erythematosus,
- rheumatoid arthritis.
- Pathology of the cardiovascular system:
- hypertonic disease,
- heart failure.
- Liver diseases and other comorbidities:
- cirrhosis of the liver,
- inflammatory bowel disease,
- immunodeficiency virus (HIV),
- malignant tumor, etc.
Classify vasculitis by clinical and histological manifestations, the size of the affected blood vessels and the depth of the pathological process.
From the diameter of the affected blood vessels, allergic vasculitis is divided into:
- superficial (dermal vasculitis), when arterioles, venules and capillaries of the skin are affected,
- deep (dermo-hypodermal vasculitis), when the arteries of medium and large caliber are affected, and the veins (the so-called muscle vessels).
In the formation of allergic vasculitis play an important role infectious-toxic agents that stimulate the production of circulating immune complexes (CIC), which are deposited on the vascular endothelium (walls). Eventually, the endothelium of the blood vessels is damaged, the inflammatory process develops and the permeability increases - an allergic vasculitis is formed. The severity of vasculitis depends on the number of CICs in the bloodstream.
 [1],
[1],
Causes of Allergic Vasculitis
There are such causes of allergic vasculitis.
- Infectious nature of occurrence:
- bacterial flora (ẞ - hemolytic streptococcus group A, tuberculosis mycobacterium, Staphylococcus aureus, leprosy);
- viral flora (influenza, herpes, hepatitis A, B and C);
- fungal diseases (genus Candida).
- Reaction to taking drugs:
- antibacterial drugs (penicillins, sulfonamides, streptomycin);
- insulin use;
- vitamin complexes;
- taking oral contraceptives;
- the introduction of streptokinase, etc.
- Exposure to food allergens - dairy protein, gluten.
- The influence of compounds of chemical origin - oil refining substances, insecticides, household chemicals.
 [2]
[2]
Symptoms of Allergic Vasculitis
The leading clinical symptom of allergic vasculitis with the defeat of small-caliber vessels is palpable purpura. Palpable purpura is a hemorrhagic rash slightly elevated above the skin (at the initial stage of the disease, you can not feel it).
In the case when blood clotting is impaired and thrombocytopenia is noted, hemorrhages (petechiae) are clinically presented as spots and cannot be felt. Allergic vasculitis is distinguished by the occurrence of inflammatory infiltrates in connection with which papules are presented which can be palpated.
The magnitude of the rash in allergic vasculitis varies from a few millimeters to several centimeters. A characteristic feature is the symmetry of the rash.
With a strong inflammatory process, palpable purpura is transformed into a blistering rash filled with hemorrhagic contents. Subsequently, necrosis and ulcers form at the site of such blisters. In connection with what these forms of allergic vasculitis are distinguished:
- papular
- vesicular,
- bullous,
- pustular,
- ulcerative.
Sometimes with allergic vasculitis, a feeling of itching and soreness in the area of the affected areas is possible. After the healing of the eruptions, hyperpigmentation remains, the formation of atrophic scars is also possible.
Most often, the rash is located on the legs, although it is possible that it spread to other areas (usually not affected - the face area, mucous membranes, palms and soles).
Allergic skin vasculitis
Allergic Skin vasculitis - polietiologichesky set of diseases and a clinical symptom of a very diverse. But the main clinical symptom is skin damage from spots to ulcers (that is, rash polymorphism is characteristic). The rash is often accompanied by itching, burning or pain. In parallel with the defeat of the skin, there is a worsening of general well-being: high fever, lethargy, myalgia and arthralgia, loss of appetite, vomiting and the presence of pain in the abdomen.
As such, the classification of allergic vasculitis of the skin is not, their separation comes from the depth of the damaging process. In this connection, superficial and deep vasculitis are distinguished.
Superficial allergic vasculitis is divided into:
- Hemorrhagic vasculitis (Schönlein – Genoch disease).
- Allergic arteriolitis Ruiter.
- Hemorrhagic leucoclastic microbid Misher - Blind.
- Necrotic vasculitis of Werther Dümling.
- Acute smallpox-like lichenoid parapsoriasis.
- Hemosiderosis (capillaries)
- annular telangiectatic purpura,
- eczematoid purpura,
- Shamberg's disease,
- the wicked purple,
- purple pigment lichenoid dermatitis,
- arcuate telangiectatic purpura,
- white skin atrophy,
- purple pigment angiodermitis,
- orthostatic purpura,
- netted senile hemosiderosis.
- Hemosiderosis (capillaries)
- Among the deep allergic vasculitis are distinguished:
- Every form of periarteritis nodosa.
- Erythema nodosum - acute and chronic forms.
Hemorrhagic vasculitis (Schönlein – Genoch disease)
Determined by systemic damage to the vascular endothelium, with the formation of erythema on the skin surfaces, which soon transform into hemorrhagic elements. This form of vasculitis is characterized by damage to the joints and vital organs (mainly the stomach, intestines and kidneys). Most often develops in children as a result of an infectious disease (ten to twenty days). It is characterized by acute onset, increased temperature, intoxication syndrome.
There are (conditionally) the following types of hemorrhagic vasculitis :
- simple kind of purpura,
- necrotic,
- rheumatic (articular),
- abdominal,
- lightning look.
The rash with hemorrhagic vasculitis is symmetrical, located on the legs and buttocks, does not pass when pressed. Rashes have a wave-like character, appear on average once a week. Damage to the joints occur simultaneously with the defeat of the skin or after a couple of hours. Characterized by damage to the joints of a large size (knee, galeoustope).
With simple purpura, only skin eruptions are noted. The general state of health is not disturbed and the internal organs are not affected, and if they are involved in the pathological process, it is insignificant. The acute course is characteristic of a child’s body. The duration of the disease can vary from a couple of days to a couple of weeks. Rashes in the form of erythematous spots can be up to two millimeters in size, but sometimes reach two centimeters. Simultaneously with the spots, urticaria elements are formed, accompanied by itching of the skin. Usually with a simple purpura, the rash disappears without a trace, only in rare situations can hyperpigmentation remain.
Necrotic purpura is characterized by polymorphism of rash, when on the skin at the same time there are spots (erythema), nodular rash, blisters (with hemorrhagic or serous filling) and necrotic changes of the skin, ulcers and crusts of hemorrhagic nature. After healing of ulcers, scars often remain.
For rheumatic purpura characteristic simultaneous damage to the skin and joints. Large joints (knee and galeous feet) are often damaged, their soreness occurs and swelling is visible above their surface. The joints are affected simultaneously with the defeat of the skin, but may also precede vasculitis or vice versa - after a couple of hours, and then weeks. The skin over the area of the joints acquires a yellow-green color, which indicates that there was a hemorrhage.
Abdominal hemorrhagic vasculitis often occurs at an early age and adolescence. Difficult to diagnose, because skin rashes can be absent and manifest only in symptoms of lesions of the digestive tract - the presence of pain in the epigastrium and intestines, vomiting, during palpation - the anterior abdominal wall is tense and painful. Kidney damage is characterized by a variety of manifestations from minor disorders to a picture of acute glomerulonephritis, which may disappear or take a chronic course.
Fulminant form - it proceeds very hard, with a high temperature, with a generalized rash, located on the surface of the skin and mucous membranes. For the lightning form is characterized by damage to the joints, vital organs. Extremely unfavorable course for life.

Allergic Arteriolitis Ruiter
Infectious - allergic vasculitis of the skin. It develops during an infectious pathology, in the presence of chronic infectious foci (tonsillitis, sinusitis, adnexitis, etc.). It is characterized by polymorphism of rash - erythematous and hemorrhagic spots, vesicular and nodular rash, necrotic changes, ulcers, serous or hemorrhagic crusts. At the end of the disease, hyperpigmentation and scarring remain. The general state of health is disturbed: weakness, lethargy, increase in temperature, poor appetite. Characterized by a long course of the disease with remissions and exacerbations.
 [5], [6], [7], [8], [9], [10], [11], [12]
[5], [6], [7], [8], [9], [10], [11], [12]
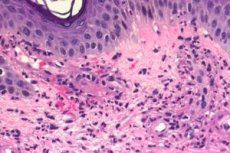
Hemorrhagic leucoclastic microbide Misher - Blind
Occurs acutely due to a chronic infectious process. The rash is represented by erythematous and hemorrhagic spotty elements on the surface of the skin of the hands and feet, extremely rarely on the front and in the mucous membranes. During exacerbations, general well-being changes - the temperature rises, appetite decreases, and weakness appears. The intradermal bacterial filtrate test (streptococcal antigen obtained from the tonsils) is positive. During the histological study, significant leukoclasia is observed, characterized by the disintegration of the nucleus of granular leukocytes.
Necrotic vasculitis of Werther Dümling
The main manifestation of this disease is brownish - bluish dermal-hypodermal flat papules (nodules), of a stagnant nature, palpable when probing, have the size of a pea. Simultaneously with papules, spots of erythematous character are noted, often transforming into hemorrhagic elements. Over time, papular rashes become necrotic and ulcerative defects form in the scar tissue (atrophic or hypertrophic scars). Burning and soreness are usually absent. Symmetry is characteristic of a rash, it appears in the region of the extensor surfaces of the arms and legs, sometimes located around the joints (the location of the rash on the torso and genitals is possible). The disease proceeds for a long time with periods of exacerbations and remissions. During the exacerbation the general state of health also changes, the temperature rise is possible.
 [13]
[13]
Acute oppen-shaped lichenoid parapsoriasis
Papulosquamous skin disease with an acute course and an unknown etiology. It is assumed to occur as a reaction to the infection. Often occurs in the adolescent and young periods. On the skin small follicular papules form, which are transformed into pustules with necrosis in the center. The general state of health is broken: the temperature rises, lymphadenitis usually joins.
Hemosiderosis (capillaries)
Occur as a result of deposition on the inner walls of blood vessels (precapillaries and capillaries) hemosiderin. Hemosiderin is a pigment containing iron and formed as a result of the breakdown of hemoglobin. When hemosiderosis appear: petechial rash, small spots of brown-yellow color and spider veins. There is a rash in the arms and legs (distal parts of them), more in the legs and is accompanied by burning of different severity. General well-being and vital organs do not suffer.
Skin form of periarteritis nodosa
Allergic vasculitis of generalized nature, accompanied by a lesion of the arteries of the muscular type (medium and large). Capillaries are not included in the pathological process. Most often, this pathology is characteristic of men. It develops on the introduction of drugs - vaccines, serums, antibiotics, as well as a reaction to bacterial and viral infections. The disease occurs more often acute, less subacutely. The temperature rises, weakness and loss of appetite appear. Along the course of the arteries nodules are formed (thickenings) in the form of aneurysmal vascular protrusions. Vascular occlusion, thrombosis, followed by hemorrhage, ulceration and possible secondary infection occurs. In the future, vital organs (kidneys, digestive system, etc.) are affected. Rashes on the surface of the skin are represented by a nodular rash - single or grouped, dense, mobile and painful. The rash is prone to necrosis and ulceration. Ulcerative defects bleed and heal for a long time.
Erythema nodosum
A variety of allergic vasculitis, characterized by the formation of dense painful nodules and nodes, which are usually located in the region of the legs (on the front surface) symmetrically. After the nodular rash has healed, the induration is long lasting; ulcers and scars are not characteristic. It is often observed in women at a young age. There are acute and chronic. During the period of acute erythema nodosum, there is an increase in temperature, the occurrence of weakness, headache, myalgia and arthralgia.
Allergic vasculitis in children
Allergic vasculitis in children is characterized by a more acute onset, and it is difficult to develop with severe symptoms than in adults. Skin rashes are prone to generalization. General well-being suffers - there may be a high temperature reaction, lethargy, weight loss, lack of appetite, nausea, vomiting, pain in the epigastrium and intestines, arthralgia and myalgia, the symptoms of the inflammatory process are more pronounced. Especially severe allergic vasculitis is transferred if vital organs and systems are involved in the process. A distinctive feature of allergic vasculitis in children are more frequent relapses. In the childhood period, hemorrhagic vasculitis (Schönlein-Genoch disease) and periarteritis nodosa are found.
Risk factors in the formation of allergic vasculitis in children are.
- Genetic susceptibility to cardiovascular and rheumatic diseases.
- Frequent acute infectious diseases.
- Chronic infectious process in the body.
- The occurrence of hyperergic reactions to drugs, food, insect bites.
- Vaccination.
- Hypothermia
- Helminths often trigger vasculitis.
- Impaired immunity.
Infectious-allergic vasculitis
Infectious - allergic vasculitis - a disease of a hyperergic nature that occurs during infectious diseases due to concomitant toxic-allergic reactions. The cause of vasculitis is the damaging effect of infectious agents and their toxins on the walls of blood vessels. Skin rashes are polymorphic, overall well-being suffers significantly. Infectious-allergic vasculitis most often occurs with streptococcal and staphylococcal lesions of the body, with viral infections (influenza, hepatitis), with tuberculosis, etc.
 [37]
[37]
Toxic allergic vasculitis
Toxic - allergic vasculitis - the defeat of the skin that occurs as a response to the action of substances that are allergens and have a toxic effect (drugs, food, chemicals). These substances can get into the body:
- when taken orally (through the digestive system),
- through the respiratory tract,
- during intravenous, intradermal or intramuscular administration.
The disease usually occurs acutely. The rash may be polymorphic - urtikarnogo nature, core-like, scralatino- or rubella-like, in the form of purpura, lichenoid, eczematous nature, etc. The rash is located on the skin and mucous membranes. Rashes are accompanied by a worsening of general well-being: an increase in temperature response, itching and burning of the affected areas, dyspepsia (nausea, vomiting, abdominal pain), muscle and joint pain, and the nervous system are affected. In the case of repeated contact with the factor that caused the vasculitis, the rash usually appears in the same place, although the occurrence of a new one is possible. A very severe course of toxic-allergic vasculitis is also possible - Lyell and Stevens-Johnson syndrome.
Syndrome is a severe course of allergic bullous skin lesions. It begins acutely, the general state of health is progressively deteriorating, and the intoxication syndrome is rapidly increasing. Rash on the skin is corpeal or scarlet-like, painful. After a couple of hours, the rash transforms into blisters filled with serous or serous-hemorrhagic contents. Quickly being opened, form erosion of bright red color. Light rubbing of healthy skin is accompanied by desquamation of the epidermis and exposure of the weeping surface (Nikolsky's symptom). Often affects the internal organs - the heart, liver, kidneys, intestines. Lyell syndrome requires immediate medical attention.
syndrome Stevens-Jones syndrome is the most severe exudative erythema. It starts suddenly and acutely with a rise in temperature. On the conjunctiva, a false film of yellowish or white-yellow color is formed, which can be removed. This film disappears on average in a month. If the course of the disease is complicated, there is a corneal sting and conjunctival scarring. In parallel with the defeat of the conjunctiva, the skin is also affected; they are formed on it - spots of erythematous character, blisters, tubercles, edema and serous-bloody exudation on the lips, oral mucosa. An unpleasant smell of purulent discharge from the mouth, external genital organs.
Systemic allergic vasculitis
Systemic allergic vasculitis is a disease resulting from inflammatory damage to the walls of blood vessels of an autoimmune nature with a variety of clinical manifestations. Systemic allergic vasculites include:
- Nodular polyarteritis.
- Wegner's giant cell granulomatosis.
- Arteritis Takayasu (non-specific aortoarteritis).
- Hamman-Rich syndrome, Goodpcacher, Kawasaki, Cherje-Strauss, Lyell, and Stevens-Johnson.
- Burger, Horton, Behcet, Christian-Weber, Moshkovits.
- Vasculitis in large and small collagenoses (systemic scleroderma, systemic lupus erythematosus, rheumatism, rheumatoid arthritis).
Systemic allergic vasculitis is characterized by the simultaneous involvement of many organs and systems in the pathological process. A distinctive feature is the presence of a pronounced exudative component, cyclicity during the process and signs of sensitization, as well as the presence of histo-morphological criteria for fibrinoid degeneration of the main substance of the connective tissue of the vascular walls.
Diagnosis of Allergic Vasculitis
The diagnosis of allergic vasculitis is based on:
- case history
- complaints,
- clinical picture
- additional survey methods:
- general clinical laboratory tests (complete blood count, urine test, biochemical blood test, blood test for sugar),
- determination of ASL-O in case of suspected disease caused by beta - hemolytic streptococcus,
- quantitative analysis of blood immunoglobulins,
- determination of CIC (circulating immune complexes),
- bacteriological examination of nasopharyngeal swabs, as well as urine and feces,
- examination of women by a gynecologist,
- PCR study to identify various infections
- ECG and angiography, X-ray,
- ultrasound diagnostics of blood vessels
- Consultations of narrow specialists: dermatologist, phthisiologist, cardiologist, vascular surgeon, rheumatologist, venereologist.
 [38]
[38]
What do need to examine?
Who to contact?
Treatment of Allergic Vasculitis
Treatment of allergic vasculitis complex.
- It is necessary to prevent exposure of the allergen to the body, which contributed to the development of allergic vasculitis: stop taking the drug or some product, exposure to chemical agents, etc.
- Bed rest is necessary, especially in the acute period of the disease.
- A diet with plenty of vegetables, fruits, and protein foods (limit salty, fried, fatty). In the diet, exclude products that cause allergies (this may be citrus fruits, honey, nuts, chocolate, red fish, etc.).
- Plentiful drink, for the purpose of detoxification therapy (at least 1.5-2 liters per day). In severe cases, intravenous drip management of physiological solutions with drugs.
- Identification and treatment of chronic infection. When it is possible to prescribe antibacterial drugs (from the macrolide groups - sumamed, cephalosporins - cefoxime, etc.).
- Often, especially in severe cases, glucocorticosteroids are prescribed, which have anti-inflammatory, antihistamine, immunosuppressive effects (prednisone, dexamethasone).
- In the complex therapy are used:
- antiplatelet drugs - reduce blood clots (pentoxifylline, acetylsalicylic acid, clopidrogel, chimes, trental),
- vascular protectors that increase vascular tone, reduce their prolinkability, reduce bleeding (askorutin, dicine, etamzilat),
- inhibitors of proteolytic enzymes, contribute to the improvement of microcirculation, respiratory depression and reduce thrombosis (aminocaproic acid),
- antihistamines (Erius, tavegil, suprastin),
- nonsteroidal anti-inflammatory drugs (dicloberl, movalis).
- Appointment of vitamins C and P (have an antioxidant effect, strengthen the walls of blood vessels, improve immunity).
- It is possible to use drugs for topical use, especially during the healing period - solcoseryl, troxevasin (improve and accelerate healing).
- Extracorporeal methods of treating allergic vasculitis are widely used:
- plasmapheresis (using this method removes part of the plasma with harmful substances - toxins, antigens, etc.),
- hemosorption (using this method removes toxins, antigens, immune complexes from the blood).
The complex of therapeutic measures is assigned strictly individually for each case of allergic vasculitis. This takes into account the causes of its occurrence, the clinical picture, the severity and severity of the process and age.
Prevention of allergic vasculitis
Prevention of allergic vasculitis is as follows.
- Timely and correct treatment of diseases against which vasculitis may develop.
- Sanitation of chronic foci of infection.
- Avoid contact with known allergies.
- To exclude unreasonable medication and vaccination.
- Lead a healthy lifestyle (do not drink alcohol, do not smoke).
- Eat right - more fruits, vegetables, proteins (exclude salty, fatty and fried).
- Doing sports - swimming, running, walking, etc.
- Do not overcool and overheat, as This all negatively affects the state of immunity, worsens the properties of the skin.
 [39]
[39]

