Cytomegalovirus hepatitis
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Epidemiology
CMV infection is widespread. In 70-80% of adults, viral neutralizing antibodies are found in the blood. In 4-5% of pregnant women, the virus is excreted in the urine, in scrapings from the cervix, it is determined in 10% of women, in milk - in 5-15% of nursing mothers. Among newborns who died from various causes, signs of generalized CMV infection are detected in 5-15%. Cytomegalovirus hepatitis is 1% in the etiological structure of acute icteric hepatitis of viral etiology. However, the prevalence of cytomegalovirus hepatitis as a whole has not been studied to date.
The source of CMV infection is only a person, a patient or a virus carrier. Transmission is carried out by contact, less often - by airborne and enteral. In addition, infection can occur parenterally, including when transfusing blood products. This transmission pathway appears to be more likely than commonly believed, which is confirmed by the frequent detection of cytomegalovirus in donors (up to 60%). The transplacental route of transmission of infection has been reliably proven. Infection of the fetus occurs from the mother - carrier of the virus. Infection is transmitted directly through the placenta or ingranatally during the passage of the child through the birth canal. Newborns can become infected through the mother's milk.
With cytomegalovirus hepatitis, the primary routes of infection are parenteral and perinatal, when cytomegalovirus enters the bloodstream directly, bypassing the patient's lymphoid apparatus.
Causes of the cytomegalovirus hepatitis
Cytomegalovirus, a representative of the family Nepresviridae, was isolated in 1956 by M. Smith. According to modern classification, it is called the human herpesvirus type 5 (HHV5). Currently, there are two serotypes of cytomegalovirus. By morphology, it is similar to the herpes simplex virus. The virion contains DNA and has a diameter of 120-140 nm, is well cultivated in human embryo fibroblast culture. The virus is well preserved at room temperature, sensitive to ether and disinfectants. Has a weak interferonogenic effect. Cytomegalovirus causes disease only in humans. The fetus and newborns are especially sensitive to the virus.
Pathogens
Pathogenesis
The pathogenesis of cytomegalovirus hepatitis is still unclear. Traditionally, it is believed that CMV primarily affects the bile ducts with the development of cholestatic hepatitis. However, the direct cytopathic effect of CMV directly on the liver parenchyma is allowed. Some consider cytomegalovirus an undoubted hepatotropic agent. In this case, liver damage can be noted both with congenital and with acquired CMV infection.
In the formation of an isolated lesion of hepatocytes in cytomegalovirus hepatitis, an immediate entry of the causative agent into the blood (parenteral mechanism of infection) can play an important role. In this case, the virus does not enter the lymphatic system, and consequently - into the regional lymph nodes, and especially does not multiply in them. The causative agent immediately appears in the general circulation, from where it enters the parenchyma of the liver. This phase of the pathogenetic chain can be conditionally called parenchymatous diffusion. In this case, the virus can immediately penetrate into hepatocytes, where it finds conditions for reproduction.
In the pathogenesis of isolated cytomegalovirus hepatitis, the role of different cytomegalovirus genotypes as well as the polymorphism of candidate histories of the main histocompatibility complex (HLA system) on chromosome 6 of a susceptible individual can not be ruled out.
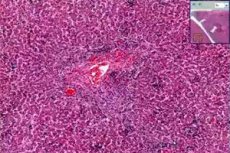
Pathomorphology
Morphological changes in acute cytomegalovirus hepatitis in healthy adults are characterized by a combination of intralobular granulomas with infiltration of sinusoids by mononuclears and periportal inflammation. The phenomena of necrosis of hepatocytes can be expressed only slightly.
In adults immunocompromised (with renal transplantation) with chronic cytomegalovirus hepatitis, periportal and perisinusoidal fibrosis, mixed cell infiltration, hepatocyte balloon dystrophy, and cholestasis are observed. In the earliest periods of the disease, cytomegalovirus antigens in the liver are detected in sinusoidal cells as a result of hematogenous spread of the virus. Necrotic, dystrophic changes on the part of hepatocytes, lymphocytic infiltration, activation of Kupffer cells are noted, whereas specific cell transformation is rare. Cytomegalovirus hepatitis in these patients is accompanied by a cholestatic syndrome and a syndrome of extinction of the bile ducts. In this case, pp65-antigenemia and CMV DNA in hepatocytes are detected, and signs of liver cirrhosis can be observed.
In addition to the classical changes characteristic of viral hepatitis, small aggregates of neutrophilic polymorphonuclear leukocytes, often located around an infected hepatocyte with intranuclear inclusions of CMV, can be found in patients with cytomegalovirus liver disease. Immunohistochemistry methods revealed that the basophilic granularity of the cytoplasm in cells without classical intranuclear inclusions of CMV is caused by the presence of a cytomegalovirus material. Thus, not only the intranuclear inclusion of the virus, but also the basophilic granularity of the cytoplasm serve as a characteristic feature of CMV-hepatitis.
In general, in immunocompromised patients, CMV infection has a more pronounced cytopathogenic effect and has a more extensive lysis of hepatocytes than in immunocompetent patients with CMV-hepatitis.
Morphological changes in liver tissue in children with congenital CMV-hepatitis are characterized by giant cell transformation of hepatocytes, phenomena of cholestasis, portal fibrosis, proliferation of the epithelium of the bile ducts, and in cases of fulminant forms - massive necrosis of the liver.
Symptoms of the cytomegalovirus hepatitis
Cytomegalovirus hepatitis can have both acute and chronic course.
 [23]
[23]
Acute acquired cytomegalovirus hepatitis
Acquired acute CMV-hepatitis in children, adolescents and young adults can be diagnosed within the symptom-complex of infectious mononucleosis. However, in some cases, isolated liver damage is observed. In this case, the disease occurs in anicteric, mild, moderate or severe form. In isolated cases, fulminant hepatitis can form.
The incubation period for CMV-hepatitis is not exactly established. Presumably it is 2-3 months.
Pre-zheltushny period. Clinical manifestations and laboratory indices in acute CMV-hepatitis do not fundamentally differ from those in viral hepatitis of other etiology. The disease begins gradually. In patients, there is a decrease in appetite, weakness, headache, abdominal pain. In some cases, body temperature rises to 38 ° C,
The duration of the pre-jaundiced period of acute CMV-hepatitis a usually ranges from 3 to 7 days.
Clinical manifestations of the pre-jaundiced period may be absent. In such cases, the manifest initial form of cytomegalovirus hepatitis debuts with the appearance of jaundice.
The icteric period. In patients after the appearance of jaundice, the symptoms of intoxication, observed in the pre-zhelth period, persist or even increase.
Clinical and laboratory manifestations of acute cytomegalovirus hepatitis do not fundamentally differ from those in viral hepatitis of other etiology.
The duration of icteric period with acute cytomegalovirus hepatitis is from 13 to 28 days.
Post-jelly period of the disease is characterized by a normalization of the patient's well-being, a decrease in the size of the liver and spleen, a significant decrease in the activity of enzymes.
Chronic cytomegalovirus hepatitis
Chronic cytomegalovirus hepatitis often develops in immunocompromised patients (infected with HIV, receiving immunosuppressive therapy, undergoing liver transplantation, etc.). So. Cytomegalovirus lesion of the graft is noted in 11-28.5% of patients who underwent liver transplantation for various reasons (autoimmune liver diseases, viral hepatitis, etc.). The DNA of CMV is found in hepatocytes of 20% of liver transplant recipients with a clinical, biochemical and histological picture of hepatitis.
However, the formation of chronic cytomegalovirus hepatitis is possible in immunocompetent children and adults. In this case, chronic hepatitis can form as a primary chronic process or in the outcome of the initial manifest cytomegalovirus hepatitis.
Clinical and laboratory indicators in patients with acquired chronic CMV-hepatitis do not differ fundamentally from those observed in chronic viral hepatitis of another etiology.
Patients with acquired chronic CMV-hepatitis are dominated by low and moderate activity of the process. In this case, in almost 3/4 cases, moderate and severe liver fibrosis is diagnosed.
In the remission period, symptoms of intoxication in patients with acquired chronic CMV-hepatitis are practically absent. In most patients, extrahepatic manifestations disappear. Dimensions of the liver and spleen are reduced, but complete their normalization is not observed. Usually the edge of the liver protrudes from under the costal arch not more than 1-2 cm. The spleen is palpated less than 1 cm below the edge of the costal arch. In the blood serum, the activity of the enzymes does not exceed normal values.
Clinical manifestations of acquired cytomegalovirus hepatitis correspond to those in acute and chronic viral hepatitis of varying severity. In 3/4 cases of acquired chronic cytomegalovirus hepatitis, moderate and severe liver fibrosis is diagnosed.
Congenital cytomegalovirus hepatitis
Congenital CMV infection can occur both in a generalized form with the defeat of many organs and systems, and in localized forms including the hepatic. Liver involvement is characteristic of congenital CMV infection and occurs in 40-63.3% of patients. Changes in the liver include chronic hepatitis, cirrhosis, cholangitis, intralobular cholestasis. The lesions of extrahepatic bile ducts, from inflammation to atresia, are recorded. To date, the role of cytomegalovirus in the genesis of lesions of extrahepatic bile ducts (atresia, cysts) remains unclear.
Congenital cytomegalovirus hepatitis is mainly registered in children of the first months. It proceeds in life, either in anicteric form with hepatosplenomegaly and biochemical activity, or in icteric form with icterism, dark urine, hepatosplenomegaly, hypertransaminase, increased level of alkaline phosphatase and GGTP, formation of liver cirrhosis in half patients. At the same time, congenital cytomegalovirus hepatitis can take the form of acute and protracted forms with one- or two-wave jaundice, mild manifestations of intoxication, activity of hepatocellular enzymes, increased by 2-3 times, with cholestatic syndrome (in 1/3 of patients), rarely taking chronic the course that in these cases develops as a primary chronic process that occurs without jaundice and with moderate or high pathological activity.
 [31], [32], [33], [34], [35], [36], [37],
[31], [32], [33], [34], [35], [36], [37],
Congenital primary-chronic cytomegalovirus hepatitis
Among children with congenital chronic CMV-hepatitis, in 1/4 of cases minimal is diagnosed, in 1/3 cases - low, in 1/3 patients - moderate activity of the pathological process in the liver.
The process has a pronounced fibrogenic orientation. In 1/3 of patients, severe fibrosis is diagnosed, in 1/3 - signs of liver cirrhosis.
Clinical manifestations and laboratory indices with congenital chronic CMV-hepatitis do not differ in principle from viral hepatitis of other etiology.
In the remission period, the symptoms of intoxication are virtually absent in patients with congenital chronic CMV-hepatitis. In most children, extrahepatic manifestations disappear. Dimensions of the liver and spleen are reduced, but complete their normalization is not observed. Usually the edge of the liver protrudes from under the costal arch not more than 1-2 cm. The spleen is palpated less than 1 cm below the edge of the costal arch in most patients with splenomegaly. In the blood serum, the activity of the enzymes does not exceed normal values.
Cytomegalovirus hepatitis in patients with liver transplantation
Cytomegalovirus hepatitis is the most frequent manifestation of CMV infection on the background of immunosuppressive therapy. In such cases, the diagnosis of cytomegalovirus hepatitis is established by the results of liver biopsy and is confirmed by the method of viral culture, ppb5 antigen, by PCR, immunohistochemical method. The majority of patients with CMV-hepatitis form isolated liver damage, and only in single patients - generalized CMV infection. Patients are prescribed ganciclovir intravenously. With AIDS, cytomegalovirus hepatitis occurs in 3-5% of patients.
In patients who underwent orthotopic liver transplantation and with AIDS, the development of the stricture of extrahepatic bile ducts of cytomegalovirus etiology is possible, which is confirmed by the detection of the B virus in the epithelium of the bile ducts. The infiltration of the donor and the liver recipient before transplantation with cytomegalovirus is considered as a factor contributing to the rejection of the graft.
 [41], [42], [43], [44], [45], [46]
[41], [42], [43], [44], [45], [46]
The course of cytomegalovirus hepatitis
The course of the disease can be acute (35%) and result in recovery with a complete restoration of the functional state of the liver in terms of 1 to 3 months. In 65% of patients in the outcome of the manifest cytomegalovirus hepatitis the disease takes a chronic course.
Where does it hurt?
Diagnostics of the cytomegalovirus hepatitis
Cytomegalovirus hepatitis is diagnosed by a combination of clinical, biochemical and serological data. The disease, as a rule, begins with astheno-dyspeptic manifestations: malaise, weakness, deterioration of appetite, accompanied by an increase in liver size and hyperfermentemia. The patient may have an indication in the history of parenteral manipulations for 2 to 3 months before the present disease, there are no markers of hepatitis A, B, C, U, G, and other viruses in the blood serum.
It is important to consider that for cytomegalovirus hepatitis is characterized by a pronounced cytolysis syndrome. For its indication, the activity of aminotransferases (ALT, ACT) and LDH fractions (LDG-4, LDG-5) is widely used. An increase in the activity of liver-celled, enzymes is characteristic for acute hepatitis and the stage of exacerbation of chronic cytomegalovirus hepatitis. The degree of increase in activity of hepatic cell enzymes in various forms of cytomegalovirus hepatitis corresponds to that of viral hepatitis of another etiology.
In the presence of jaundice, it is important to determine the level of total bilirubin and the ratio of conjugated and unconjugated fractions.
The activity of the inflammatory process in the liver to a certain extent reflects the protein spectrum of blood serum. In most cases, patients with chronic CMV-hepatitis maintain a normal level of total protein in the serum - 65-80 g / l. In patients with chronic high-activity CMV-hepatitis, disproteinemia is formed by lowering albumin levels and increasing the fraction of y-globules and new ones. The nature of disproteinemia is moderate and reaches a significant extent only in some patients, when the albumin level falls below 45%, and the level of y-globulin exceeds 25%.
With exacerbation of chronic cytomegalovirus hepatitis, the decrease in the parameters of the protein-synthetic function is the greater, the heavier the inflammatory process in the liver. Violations in the blood coagulation system (hypocoagulation) of varying degrees develop in patients with chronic hepatitis mainly by reducing the synthetic function of the liver.
The ultrasonic picture in the liver with acute and chronic CMV-hepatitis does not differ from that in viral hepatitis of another etiology.
The method of Doppler ultrasonography is used to determine blood flow in the portal vein system and the presence of portocaval anastomoses, which allows to diagnose portal hypertension, including in cirrhotic patients with cytomegalovirus etiology.
Morphological studies allow an objective assessment of the nature of the pathological process in the liver, its orientation, and also serve as one of the mandatory criteria for the effectiveness of the therapy.
The results of puncture biopsies can have a decisive differential-diagnostic significance. With a sufficient amount of punctate liver, the obtained morphological information is of decisive importance in assessing the activity, the degree of fibrosis of chronic hepatitis, and in the choice of therapeutic tactics.
What do need to examine?
Who to contact?
Treatment of the cytomegalovirus hepatitis
For the treatment of cytomegalovirus hepatitis, ganciclovir and preparations of recombinant interferon are used.
Below are the results of a single clinical trial in which 85 children who received viferon therapy for chronic cytomegalovirus hepatitis were treated. Among them 31 children with acquired and 54 with congenital CMV-hepatitis. In 49 children, congenital cytomegalovirus hepatitis was associated with a lesion of the bile excretory system (in 44 - atresia and in 5 - cysts of bile ducts), and in five - with lesions of the central nervous system.
Among the observed patients, 47 boys and 38 girls. 55 children were under the age of 1 year, 23 - from 1 to 3 years and 7 - older than 3 years.
For the course of chronic viral hepatitis, 45 children received monotherapy with viferon in rectal suppositories, 31 - viferon in combination with intravenous immunoglobulins, 9 children - combination therapy consisting of viferon and ganciclovir. The dose of interferon is 5 million / m 2, 3 times a week.
The duration of treatment was 6 months in 67 patients, 9 in 11 and 12 months in 7 children. Criteria for the effectiveness of interferon therapy were determined in accordance with the consensus of EUROHEP.
The control group consisted of 43 children. It included 29 patients with congenital and 14 - chronic hepatitis of cytomegalovirus etiology. These children received basic therapy, including only choleretic, vitamin preparations and hepatoprotectors.
In addition to clinical and biochemical control, the replication activity of the cytomegalovirus was verified in the disease dynamics.
The proportion of children with chronic CMV-hepatitis, who had complete remission with viferon therapy, was low and did not reach 20%. However, the combined group of children who had any remission was 78.8% of the total number of children treated. In this remission was absent in almost 1/4 of patients. It should also be noted that at the same time, no one in the control group had spontaneous remission.
A comparative analysis of the effectiveness of viferonotherapy in children with congenital and acquired CMV hepatitis showed that there were no significant differences in the percentage of remission with viferon therapy. The values of p varied from p> 0.05 to p> 0.2.
In order to answer the question about the dependence of the frequency of achieving remission in cytomegalovirus hepatitis against the background of therapy from the treatment regimen, three groups were identified. The first included patients who received monotherapy with viferon, the second - children who received viferon in combination with intravenous immunoglobulins, and the third - received combination therapy with viferon and ganciclovir.
There were no significant differences in the results of treatment in patients from different groups. Only a trend towards a lower cytolysis in children was observed against a background of combined treatment with viferon and intravenous immunoglobulins. The values of p varied from p> 0.05 to p> 0.1.
This pattern is also observed when evaluating the replicative activity of CMV in chronic cytomegalovirus hepatitis in children who received various treatment regimens. The frequency of detection of CMV DNA in the course of dynamic observation was practically unchanged in children from all three groups. Only slightly lower replicative activity of CMV was observed in patients on the background of treatment with viferon in combination with intravenous immunoglobulins. The values of p varied from p> 0.05 to p> 0.2.
More information of the treatment
Prevention
Specific prevention of CMV infection is not developed. Experimental work is underway to create the vaccine.
Anti-epidemic measures in the foci of infection are not carried out. Given the potential role of the parenteral mechanism of infection in the formation of cytomegalovirus hepatitis, measures to curb all parenteral, including transfusion, infections are particularly important. The use of disposable needles, adherence to sterilization rules for surgical instruments can completely prevent infection with parenteral manipulation.
To prevent infection with cytomegalovirus during blood transfusions and its components, it is necessary to solve the problem of testing donated blood for CMV DNA.

