Skin hemangioma
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Causes of Hemangioma Skin
In most cases, a hemangioma tumor of the skin develops from birth as a result of the proliferation of blood vessels.
 [6]
[6]
Pathomorphology
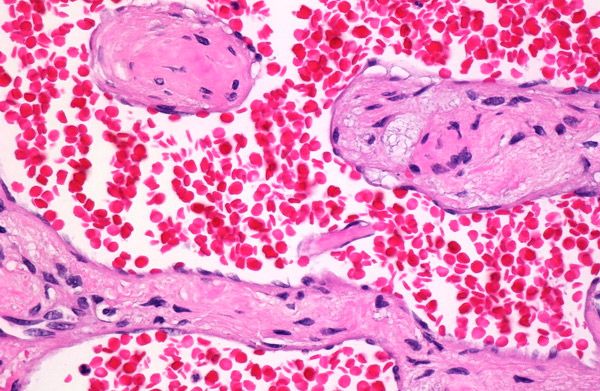
The site consists of a different number of capillaries, sometimes closely adjacent to each other, and therefore the tumor acquires a solid structure. In the initial period of growth, the tumor consists of cords of proliferating endotheliocytes, in which in places very narrow gaps can be found. In mature foci, the capillary gaps are wider, and the endothelium lining them is flattened. Subsequently, in the stage of regression, fibrous tissue grows in the stroma of the tumor, which squeezes and replaces the newly formed capillaries. This leads to wrinkling and complete disappearance of lesions. Sometimes among the capillaries there are vessels of another type, mostly venous. In such cases, such a tumor is called mixed hemangioma.
Juvenile granuloma occurs in one of 200 newborns. It manifests itself in the first weeks of a child's life in the form of a red spot, which increases, protruding above the skin level. Within 6 months it reaches its maximum development. The number of lesions varies from single to multiple. Usually by 6-7 years of life in most patients (70-95%) the hemangioma is significantly or completely resolved.
Cavernous hemangioma - a limited tumor of the color of normal skin with a deep location, red with a bluish tinge - with an exophytic nature of the formation. The surface of the tumor is smooth, but may be lobed with hyperkeratosis or verrucous. There is a spontaneous regression of the tumor before puberty, but the course can also be progressive with the destruction of the adjacent tissues. Cavernous hemangioma can be combined with capillary hemangioma. In some cases, one-sided localization of this tumor has been described. Furthermore, there is a combination with osteolysis (Mafuchchi syndrome), thrombocytopenia (Kazabaha-Merritt syndrome) as well as a combination of multiple cavernous hemangiomas with diskhondroplaziey resulting defect ossification, brittle bones, their deformation and formation of osteochondritis, which can be converted in chondrosarcoma (syndrome Mafucci).
There are two types of cavernous hemangioma: with arterial and venous differentiation of the vascular walls.
Hemangioma with arterial differentiation (arterial cavernoma) is less common, occurs mainly in adults. Because of the thick walls of the vessels forming it, it has a livid blue color. At the same time in the entire thickness of the dermis a large number of newly formed arterial-type vessels are found. In the process of tumor growth, all elements of the vascular wall take part. Hyperplasia of the muscular elements of the vessels, which, however, retain their lumen, is especially pronounced and uneven.
Hemangioma with venous differentiation (venous cavernoma, cavernous hemangioma) is characterized by the presence in the dermis and subcutaneous tissue of large, irregular-shaped cavities lined with one layer of flattened endotheliocytes separated from each other by fibrous cords. Sometimes, as a result of the proliferation of adventitial cells, these cords become sharply thickened.
Skin Hemangioma Symptoms
There are capillary, arterial, arteriovenous and cavernous (juvenile) forms.
Capillary hemangioma is a vascular tumor, which is based on the proliferation of endotheliocytes with the formation of capillaries. It is clinically characterized by bluish-red or purple spots, sometimes slightly protruding above the surface of the skin, turning pale when pressed. Its variant is a stellate angioma in the form of a dotted red spot with capillary vessels extending from it. Appears in early childhood (from 4 to 5 weeks), increases in size up to a year, and then begins to regress, which is observed in 70% of cases, as a rule, up to 7 years of age.

Sometimes the capillary hemangioma is combined with thrombocytopenia and purpura (Kazabah-Merritt syndrome).
What do need to examine?
How to examine?

