Bartholin gland abscess
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
There are true and false Bartholin gland abscess.
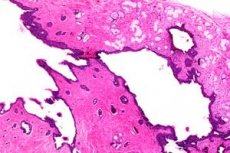
Large vestibule gland (Bartholin gland) - pair formation. It belongs to the complex-tubular glands, has a rounded shape and size with a large pea. The glandular acini is lined with a single-row cylindrical epithelium secreting mucus.
The main excretory duct of the great gland vestibule is formed from the confluence of several ducts. It opens on the eve of the vagina from the front and outside of the hymen. The duct is lined with transitional epithelium, its length is 1.5-2 cm.
What causes a Bartholin gland abscess?
A true Bartholin gland abscess is characterized by the involvement of an acute purulent melting tissue of the entire gland and its surrounding tissue in the process. True bartholinitis is caused by pyogenic cocci, often gonococcus, having a tropism for the cylindrical epithelium lining the gland. In gonorrhea of the lower parts of the genital tract, Bartholin gland ducts are involved in the process in 20-30% of cases, and often indirectly due to the presence of abundant purulent discharge in the vagina.
False abscess (primary - as a result of infection and abscess first formed as a result of occlusion of the duct or secondary retention cysts - suppuration long existing cyst Bartholin gland) often called associative flora (staphylo-, streptococci, kolibatsillyarnaya flora, anaerobes, fungi).
Currently, false abscess formation is more common. The formation of a "false" abscess of the gland is facilitated by certain anatomical prerequisites, namely a significant narrowing of the duct along its length. In the place where the small ducts flow into the main duct, a kind of ampoule containing a secret is formed in the gland; then the main duct narrows, and at the exit to the outside it is already a pinhole. The presence of inflammatory edema in the area of its external opening with vulvitis, colpitis, as well as inflammation of the mucosa of the duct itself (canaliculitis), contributes to its rapid closure, delay and infection of the secretion of abundantly septenant gland, which leads to the formation of a false abscess (primary) or cysts.
Symptoms of a Bartholin gland abscess
The clinical picture of the disease does not depend on the type of abscess formation (true or false) and has the following symptoms:
- The process is often one-sided.
- Infection of the excretory duct (canaliculitis) around its outer opening is determined by the redness - the so-called "gonorrheal spot"; on palpation of the gland appear poor purulent discharge; infiltration and tenderness in the area of the duct projection are also determined.
- When the infection spreads directly to the gland or cyst of the gland, edema of the middle and lower third of the labia majora appears and quickly grows, which passes to the skin of the labia majora, the mucosa of the labia majora and the mucous membrane of the vagina, which is due to the laxity of the subcutaneous tissue in the area; further appears hyperemia of the relevant departments.
- An inflammatory infiltration of the gland and adjacent tissues (cellulose) appears, and a clear zone of fluctuation begins to be determined later on in the infiltration, usually along the lower pole. It should be noted that with a true Bartholin gland abscess (when the tissue of the gland itself melts, and not accumulation of pus in the cyst cavity), the general and local inflammatory reaction is more pronounced: there is a sharp pain and swelling of the surrounding tissues; in contrast to the false skin over a true abscess is immobile, signs of concomitant inguinal lymphadenitis are determined.
- For Bartholin's abscess is characterized by severe pain of education. A sharp increase in pain is observed in a sitting position, when walking, defecating, and therefore patients often assume a forced position (lying down). The use of analgesics gives only a short-term effect.
In the stage of suppuration and abscess formation, hectic temperature and other signs of intoxication take place - weakness, lack of appetite, sleep disturbance. Characteristic of a surgical pathology, the sign of a “sleepless night” indicates suppuration and the need to open an abscess.
In contrast to the acute, chronic purulent Bartholinitis is characterized by a relapsing course with periods of remission and exacerbations. Palpation in the lower third of the labia majora is determined by the cystic formation of an uneven, mostly dense consistency, soldered to the underlying tissues, slightly painful, the size of the plum. An abscess is periodically opened through the exit duct of the gland on the inner surface of the labia or on the eve of the vagina (it is extremely rare to empty it into the rectum). Therefore, in such patients, deformity of the labia, vagina, or perineum is often observed as a result of repeated scarring of the spontaneous and / or surgical opening of the abscess. In some cases, a functioning fistulous course is determined on the skin or mucous membrane of the labia, in the vagina or on the perineum (the result of repeated spontaneous or artificial (marsupilization of the gland) opening of the abscess.
In remission, patients are worried about dyspareunia and leucorrhoea, due, among other things, to the presence of concomitant chronic vulvovaginitis.
In the event of an exacerbation of the process when an infection is activated and (or) an outflow disturbance (the perforation hole often closes), all the signs of acute inflammation described above appear.
Diagnosis of the Bartholin's gland abscess
Diagnosis of the Bartholin gland abscess is simple and consists of examination and palpation. Additional research methods are usually not required.
The area of the opening of the excretory duct is carefully inspected, paying attention to the nature of the discharge, the presence of spots, swelling (edema), hyperemia around the opening, asymmetry. To do this, divorce the labia to the thumb and index fingers of his left hand. Then the gland is palpated, determining the signs of inflammation (edema, hyperemia), localization and size of the inflammatory formation, its consistency (dense or uneven consistency with areas of fluctuation), as well as soreness. Bartholin gland abscess is characterized by the presence of pronounced asymmetry - the genital slit has a crescent shape, its convex side faces the healthy side. Sometimes the tumor completely or partially closes the genital slit.
The state of the regional (inguinal) lymph nodes is assessed, with a complication of the process, signs of inguinal lymphadenitis appear on the appropriate side.
When specific (gonorrheal) Bartholinitis should be aware of metastatic lesions, and in particular of gonorrheal arthritis.
 [7], [8], [9], [10], [11], [12], [13]
[7], [8], [9], [10], [11], [12], [13]
Differential diagnosis of Bartholin's gland abscess
As a rule, recognition of the Bartholin gland abscess is not difficult. However, some purulent diseases can occur, ignoring the symptoms of which leads to diagnostic errors. First of all, they should include furunculosis of the skin of the large genital lips.
The furuncle is an acute purulent inflammation of the hair follicle and surrounding tissues (sebaceous gland and connective tissue). Often caused by Staphylococcus aureus and is found in individuals with metabolic disorders and decreased immunity (diabetes, vitamin deficiencies, chronic infections). When viewed on the labia majora, an inflammatory cone-shaped infiltrate is defined, with a pus with a black dot (necrosis) under the epidermis on top. Furunculosis of this area is accompanied by a significant swelling of the surrounding tissues. In advanced cases with large sizes of the boil, the patients have signs of purulent intoxication (weakness, fever), lymphangitis and regional lymphadenitis, and in the most severe cases, acute thrombophlebitis.
Carbuncle - acute purulent-necrotic inflammation of several hair sacs and sebaceous glands with the formation of general and extensive necrosis of the skin and subcutaneous tissue. The patient is worried about strong, "tearing" pain, there is a high fever, other symptoms of intoxication are pronounced (weakness, loss of appetite, nausea, headache). On examination, infiltration is determined in the region of the labia majora, the skin over it is of a purple tinge, with a multitude of thinning, from which thick greenish-gray pus is secreted (a “sieve” symptom). Often the holes merge to form a large defect in the skin. The disease is often complicated by lymphangitis and regional lymphadenitis.
Suppurative cyst gartnerovogo course. Typical localization of the cyst - the upper or middle third of the lateral vaginal wall, extremely rarely - the lower sections; while the cyst is always located above the lower third of the labia majora. The cyst has the shape of an elongated oval, the upper pole "goes" deep into the paravaginal, and sometimes into the paravesicular fiber. Contamination of the contents (yellow mucinous liquid) is rare.
Complications of bone tuberculosis (in particular, tuberculosis of the arc of the pubic bone). With this disease, the "chickens" can spread to the pararectal and paravaginal tissue and the labia, simulating a Bartholin gland abscess. Recognizing this disease is helped by a thorough collection of anamnesis, as well as X-ray examination (X-ray or CT scan of the lungs and pelvic bones).
Bartholin gland cancer. On palpation in the corresponding area, a dense, uneven, painless mass is formed, welded to the underlying tissues. Discharge - hemorrhagic, serous or purulent. Ulcerations appear late. Cytological examination of exudate, punctate or biopsy is confirmed by the diagnosis of the tumor.
What do need to examine?
What tests are needed?
Bartholin gland abscess treatment
Conservative treatment is permissible and is successful only in the initial stages of the disease (infiltrative stage) with at least partial outflow from the gland. In such cases, prescribed therapy for acute suppurative inflammation.
When abscessing is adequate, only the surgical method of treatment is the opening of the abscess. Late surgical intervention leads to complications - lymphangitis, lymphadenitis, spontaneous opening of the abscess in the vagina or rectum and the transition of an acute disease into a chronic purulent-infiltrative process.
It should be noted that attempts to expand the outlet of the main duct of the gland to improve the outflow of purulent secretions are always unsuccessful. Puncture abscess, aspiration of its contents and washing with antiseptic solutions, as a rule, gives a short-term effect associated with the evacuation of pus; the puncture hole then closes immediately and does not provide a constant outflow from the purulent cavity.
Adequate benefit is a wide opening of the abscess at the lower pole in the area of fluctuation from the mucous membrane of the labia. After complete emptying (as a rule, there is one purulent cavity), the cavity is reorganized with antiseptic solutions (they are administered using a syringe through a tube until a “clean” solution is obtained). The patient's condition immediately improves, pain decreases, symptoms of purulent intoxication disappear. To ensure the natural outflow after the opening of the abscess, patients need to walk. It is advisable to rinse the abscess cavity 2-3 times on the first day, in the future it is enough to perform the manipulation once a day.
It is not recommended to leave tubes (except ADF) in the abscess cavity, to introduce turunds, especially gauze, as this does not provide drainage, but only prevents outflow, besides, these objects, being foreign bodies, absorb the purulent secret on themselves.
Local (turunds, gaskets, tampons) application of ointment agents, especially those containing components that enhance regeneration, is also illogical, since the rapid epithelialization of the wound that occurs during this process causes a disturbance of the outflow, and the risk of recurrence increases.
In parallel with the surgical component, of course, is carried out and drug treatment of acute suppurative inflammation, including the fight against microbes, edema, etc.
Further, resorptional treatment, physiotherapy, and restorative treatment are carried out.
If a false Bartholin gland abscess has occurred and after the treatment, the Bartholin gland cyst is determined, in the “cold” period (after 2-3 months) a planned surgical procedure is performed, in which the entire cyst capsule is necessarily removed to prevent recurrence.
The operation of marsupilization of the gland (opening the cyst cavity and stitching its walls to the vaginal mucosa), as a palliative and ineffective, is not currently used.
In cases of chronic purulent Bartholinitis, only surgical treatment is effective — extirpation of the gland, removal of scar and purulent-necrotic tissues, excision of the fistulous passages. The operation is carried out in the period of remission after preliminary preparation (as with other forms of chronic suppurative inflammation, the prescription of antibiotics during remission is meaningless, local rehabilitation, the use of immunomodulators, eubiotics, tissue metabolites are necessary).

