Medical expert of the article
New publications
White spots on the tip, side of the tongue: what mean, causes, what to treat
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
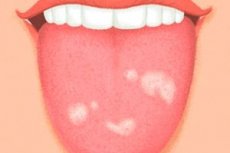
White spots on the tongue are a fairly common occurrence among children and adults. Many do not pay attention to this symptom, as they are sure that the cause is the lack of a balanced diet. This is somewhat true, however, plaque or spots may indicate the course of more severe pathological processes. Diseases of the gastrointestinal tract are not the entire list of problems that can be recognized by looking at the tongue. Acute and chronic injuries to the mucous membrane, bacterial, viral and autoimmune diseases, pathologies of the immune and cardiovascular systems - all this can manifest itself in a change in the color and structure of the tongue. Having assessed its appearance, you can suspect many difficult to diagnose diseases. Some of them appear on the tongue, being in the early stages. This allows you to diagnose the disease in time and start treatment as early as possible. It is not for nothing that they say that the tongue is a mirror of the body, which reflects the state of all its organs and systems. There can be many reasons for plaque and white spots on the tongue. In order to avoid analyzing rare syndromes, one should abandon attachment to accepted classifications.
Causes of white spots on the tongue
Let's look at all the main diseases that cause white plaque and spots.
The appearance of white plaque in the morning
White plaque on the tongue in the morning is a completely physiological process. Its formation is explained by the fact that some taste buds of the tongue are covered with keratinized epithelium. Due to this, the upper layers of tissue are exfoliated. This is a kind of protective mechanism of the body, which allows self-cleaning of the tongue surface. Naturally, plaque in the morning can also appear with various diseases. To distinguish normal plaque from pathological, it is necessary to know the main features of physiological plaque. In a healthy person, the tongue is covered with a thin layer of epithelium in the morning. Taste buds of the tongue should be visible through it. The color of the plaque should be white or slightly grayish. But if it is yellow, brown, black or dark gray, then you should consult a general practitioner who will help identify the cause of this condition. Also, plaque can be considered physiological if it has a uniform structure: it is not collected in lumps, does not form circles, rings, stripes and other figures, covers only the back of the tongue. In addition, you should know that in the morning there should be no burning, tingling, pain in the tongue or other unpleasant symptoms. And finally, normal plaque disappears immediately after morning oral hygiene or eating. Pathological plaque does not disappear on its own during the day, but is most often removed only partially.
Geographic tongue
This is an individual structural feature of the tongue, in which there are ring-shaped whitish spots on its back. The origin and pathogenesis of this condition remain unknown. Many researchers claim that the cause is a genetically determined anomaly in the development of the tongue. Geographic tongue in children can appear from birth and proceed without any sensations for the child. When parents notice white spots on the tongue of a child, they think that these elements appeared quite recently. However, most likely, the white formations simply remained unnoticed or were expressed to an insignificant degree.
Differential diagnostics of geographic tongue is carried out with desquamative glossitis, candidiasis, leukoplakia. In this case, diagnostics is more important than the treatment itself. After all, if the presence of geographic tongue is confirmed, then treatment is not required. This anomaly does not require correction, since it does not pose a danger to the child's health. But drug treatment of the "imaginary" disease can significantly affect the health of the child's body. Therefore, a thorough examination should be carried out before planning any therapy.
Flat leukoplakia of the tongue
The tongue is an organ that is constantly exposed to traumatic damage. Teeth, food, orthopedic and orthodontic structures - all this can have a negative effect on the tissues of the tongue. Since the structure of this organ involves functioning in aggressive conditions, it quickly regenerates with minor one-time injuries. However, serious injuries, chronic damage can cause infection or a risk factor for the appearance of benign and malignant tumors. If we talk about white spots on the tongue, they can appear as a result of chronic mechanical trauma. As a rule, this type of damage is provoked by incorrectly positioned teeth, poor-quality restorations and dentures. As a result of constant damage, the epithelium covering the mucous membrane grows and thickens. This condition is called leukoplakia - hyperkeratosis of the mucous membrane. Visually, the defect looks like a grayish-white spot located on the unchanged mucous membrane. It can be located on the tip of the tongue, back, side surface or under the tongue, depending on the location of the traumatic agent. Flat leukoplakia does not rise above the level of surrounding tissues and does not manifest itself clinically. This condition should be differentiated from fungal and viral diseases, benign and malignant neoplasms.
Diagnosis of white spots on the tongue involves scraping followed by cytological examination. When analyzing the data, many epithelial cells are identified that are prone to increased keratinization.
Treatment of white spots on the tongue with leukoplakia consists of eliminating the damaging factor and using medications. Most often, doctors prescribe drugs that contain vitamins A and E. They are regulators of metabolism and cell keratinization processes. If the hyperkeratosis focus is quite extensive, cryodestruction (minimally invasive surgical treatment using liquid nitrogen) is performed.
Chemical trauma to the tongue
Chemical trauma to the tongue may manifest itself as white spots if it is caused by acidic substances. In this case, the burn site will look like a spot covered with a white film. The surrounding tissues in case of a chemical burn are usually hyperemic and edematous. Clinically, a chemical burn manifests itself quite clearly, a person is bothered by severe, constant pain in the tongue. When touching the affected area, the symptoms intensify. It is quite easy to differentiate spots caused by a burn, because the diagnosis is confirmed by a traumatic anamnesis.
Treatment of chemical trauma involves removing the irritant from the mucosal surface, using antiseptics and a neutralizing agent (for acids - alkalis: soapy water, 0.1% ammonia solution; for alkalis - acids: 5% citric acid, acetic acid; for silver nitrate - 2-3% sodium chloride solution, for phenol - 50% ethyl alcohol). After this, herbal treatment is recommended (rinsing with infusions of chamomile, sage, oak bark, etc.), which stimulate healing processes, epithelialization, and reduce inflammation.
Galvanose
Galvanosis is a disease associated with the occurrence of biocurrents between different metal alloys. For example, if one crown is made of cobalt-chromium alloy and the other is made of steel, then a galvanic current may occur between these structures. The clinical picture of galvanosis can be quite vague. The fact is that the degree of expression of this pathological process may be different for each person. Some people complain of an unpleasant taste in the mouth, viscosity of saliva, burning of the oral mucosa, etc. White spots with galvanosis occur if it provoked the occurrence of hyperkeratosis (leukoplakia) or lichen planus, which will be discussed below.
If galvanosis has a pronounced clinical picture, then it is easy to diagnose. However, if it is accompanied only by, for example, leukoplakia, then it will be difficult to detect the galvanism process. A comprehensive instrumental and laboratory diagnosis will be required, during which all pathologies that occur with hyperkeratosis phenomena will be gradually excluded.
Treatment of galvanosis involves removing the metal fillings, crowns and dentures that caused the disease. This will leave only one group of alloys in the oral cavity. Hyperkeratosis caused by galvanic currents is treated in the same way as flat leukoplakia, which was discussed earlier.
Desquamative glossitis, spots and plaque in gastritis, gastric ulcer, enterocolitis
Since the tongue is one of the organs of the digestive system, gastrointestinal diseases almost always manifest themselves on the mucous membrane of the tongue. In acute and chronic gastritis, the acid balance in the stomach is disturbed. If the acidity is reduced, the tongue has a bright pink color, a smooth surface with cracks. In case of increased acidity, acute gastritis is accompanied by a gray dense coating on the back of the tongue. Clinically, a person is concerned about dryness and an unpleasant taste in the mouth, increased viscosity of saliva. Naturally, with an acute inflammatory disease of the stomach, there will be complaints of pain in the supra-gastric (epigastric) region of a stabbing nature. Chronic gastritis is often accompanied by desquamative glossitis. The essence of this pathology is the sloughing (desquamation) of the epithelium, which leads to the formation of spots with a white border. The rest of the back of the tongue is often covered with a white coating. A characteristic feature of desquamative glossitis is its dynamism and inconstancy. Desquamation foci may change shape, merge, disappear and reappear within a few hours. In this case, there may be no complaints from the gastrointestinal tract. It is worth saying that enterocolitis and gastric ulcer are also accompanied by desquamative glossitis. However, gastric ulcer is accompanied by pronounced symptoms from the gastrointestinal tract, which makes it possible to easily identify the cause of the white coating on the tongue. Enterocolitis is accompanied by the appearance of a grayish-yellow coating. With this disease, fungal and bacterial infections are often observed.
Diagnosis of all gastrointestinal diseases begins with collecting anamnesis. If chronic pathology is present, then the version of exacerbation of the disease is considered. Instrumental diagnostics involves gastroduodenoscopy, which allows assessing the structure of the mucous membrane of the digestive organs. Laboratory tests are carried out to identify the Helicobacter Pilory bacterium, which is the cause of gastric ulcer and duodenal ulcer. It is advisable to determine the acidity in the stomach in case of gastritis. The method of treating hypoacid and hyperacid gastritis has its own characteristics. It is important to conduct differential diagnostics with candidal glossitis. To do this, a scraping is taken from the surface of the tongue, and the number of Candida fungi is determined.
Treatment of inflammatory diseases of the stomach is planned by a gastroenterologist. The therapy is complex and multidirectional. It includes antibacterial therapy (De-nol), proton pump inhibitors (Omeprazole), a therapeutic diet (exclude fatty, fried, spicy, processed foods), folk treatment (a decoction of calendula, chamomile, St. John's wort, yarrow, combined in equal proportions). Homeopathy offers the drug Gastritol, Hepar sulfur, Antimonium crudum for the treatment of gastroduodenitis. Before using any medications, you should consult a specialist. After all, the use of many medications weakens the body and provokes the occurrence of various complications.
White plaque and spots in kidney diseases
Kidney diseases are also accompanied by characteristic manifestations on the mucous membrane of the tongue. Due to the dysfunction of the excretory function, many substances remain in the body, causing its poisoning. The toxic effect of nitrogen compounds leads to disruption of the digestive, cardiovascular and nervous systems, metabolism and nutrition of cells are disrupted. As a result, the mucous membrane of the tongue becomes bright red. Changes in the properties of saliva lead to dry mouth, which in turn provokes mechanical trauma to the tongue. Violation of regeneration processes is a prerequisite for the appearance of ulcers and foci of hyperkeratosis (white spots). In addition, the process of physiological desquamation of the epithelium is disrupted, which is manifested by a grayish-white coating of the tongue. Diagnosis of kidney diseases does not cause problems for specialists. This is due to the fact that clinical manifestations in other organs occur only some time after the onset of the disease. Therefore, the root cause of the pathology is quite easy to identify. It is also worth saying that even a simple urine test can identify abnormalities in kidney function.
Treatment of plaque and spots on the tongue is carried out only in parallel with the main therapy, which is aimed at eliminating the disease of a urological nature.
White plaque and spots due to allergies
Allergic reactions are a global problem in the modern world. Every third person on the planet is allergic to some substance. This is due to the fact that the human body weakens with each generation. Poor quality food, stress, a passive lifestyle are only a small part of the reasons that increase the level of allergization of the population.
Contact drug allergy occurs when taking medications (mainly penicillins). In this condition, foci of hyperemia and papillary atrophy appear on the back of the tongue. This area may be surrounded by a white rim. An allergic reaction to tetracycline drugs is accompanied by the appearance of a grayish-brown coating on the back of the tongue. In addition to visual manifestations, there are complaints of burning of the mucous membrane, dry mouth, and impaired taste perception. A person feels that the white spot on the tongue hurts. If such symptoms are detected, it is necessary to immediately stop taking the drug and undergo a course of disensitizing therapy.
Candidal glossitis
Candidiasis is a disease caused by fungi of the genus Candida. Being representatives of saprophytic flora, these microorganisms constantly live in the oral cavity. However, when immunity decreases, fungi switch to a parasitic type of existence. This allows them to increase the number of colonies and become more resistant to the body's defenses.
Candidiasis is often observed in infants. Immaturity of the body's defense structures provokes the occurrence of fungal diseases. The first signs of a fungal infection are the child's crying, refusal to eat, and poor sleep. Upon examination, you may notice redness of the mucous membrane and a white coating on the tongue. The coating is easily removed, leaving an intact mucous membrane underneath. In adolescents and adults, candidiasis occurs in the same way as in infants. The only difference is that with age, the likelihood of the disease becoming chronic increases. It is also worth noting that the severity of the clinical picture in adults is lower than in children. There are several types of candidiasis: pseudomembranous, atrophic, and hyperplastic. All variants of the course have a common origin, but each of them has some features in the clinical picture. Pseudomembranous candidiasis is characterized by the appearance of a coating in the form of white films that are easily removed by scraping. Atrophic candidiasis is characterized by bright redness of the mucous membrane, dry mouth and a relatively small amount of white plaque. Hyperplastic candidiasis is unique in that the plaque forms in the form of papules that can merge into separate foci. This is how spots appear on the tongue. With chronic hyperplastic candidiasis, the plaque may not be completely removed, which distinguishes it from other forms of fungal infections. This disease is considered a precancerous condition, so it should be given special attention. Diagnosis of candidiasis rarely causes difficulties. It is much more difficult to determine what caused its development. In order to find out what caused the plaque or spots on the tongue, you should take a scraping and conduct a laboratory study. The material must be collected in the morning. Before this manipulation, it is contraindicated to carry out oral hygiene, drink, eat food. All this can reduce the number of colonies, which will provoke a false negative result.
Treatment of candidiasis depends on the severity of the disease. If the disease is mild, then local therapy can be enough. For this, antifungal ointments are used: Nystatin, Levorin, Natamycin. Rinsing solutions are also used: Lugol's solution diluted 2-3 times, Clotrimazole, Afmotericin. If the form of candidiasis is severe, then general antifungal therapy will be required: Fluconazole, Ketoconazole, etc. In cases of severe candidiasis, additional diagnostic manipulations should be carried out. It is necessary to identify the risk factors that provoked the development of the disease. First of all, a thorough anamnesis is carried out. This allows you to reduce the range of possible pathologies. When about 5 most likely factors remain, studies are performed to confirm or exclude them. Such tests can be an immunogram, a test for intestinal microflora, fibrogastroduodenoscopy, an analysis for TORCH infections, etc.
Lichen planus
This is a chronic disease in which the lesion is a papule.
The cause of this disease is currently unknown. However, the occurrence of this disease is associated with carbohydrate metabolism disorders, permanent stress, accumulation of metabolic products in the body and systemic diseases of various organs and systems.
Depending on the clinical picture, lichen planus (LP) is divided into 5 forms: papular, linear, reticular, annular and pigmented. In the papular form, small spots (papules) appear on the surface of the tongue. The size of the formation varies within 1-2 mm. The elements of the lesion have a whitish tint, can be located singly or in groups. Spontaneous disappearance of spots and repeated recurrence of the disease is possible. Most often, no other symptoms are observed. If they are present, then most likely they are caused by a concomitant disease. The linear form is observed on the lateral surfaces of the tongue. The name of the subspecies already indicates that the formations have a linear (strip-shaped) structure and slightly rise above the level of surrounding tissues. Most often, this form of lichen planus occurs in diseases of the gastrointestinal tract. The reticular form occurs due to the fusion of papules into a pattern that resembles a mesh. This clinical picture is called "Wickham's mesh" and is characteristic only of lichen planus. The annular form is characterized by the appearance of ring-shaped formations that are white. This pathology is very similar to geographic tongue and desquamative glossitis. However, the distinctive feature of LPL is the stable location and shape of the lesion elements. The pigmented form of lichen planus occurs in people who work with various chemicals. Most often, it is caused by metal intoxication. In this case, white spots appear on the root of the tongue, in its middle or under the tongue. The lesion elements are grayish-whitish, sometimes with a blue tint. Other symptoms, except for the appearance of spots, may not be observed. The exudative-hyperemic form differs from others only in the presence of a pronounced inflammatory reaction. The mucous membrane becomes edematous, acquires a bright red color, Wickham's mesh appears on it. Sharp pain is noted on palpation. A person is bothered by burning, itching, pain in the mucous membrane and increased viscosity of saliva. If the inflammatory process is not stopped in time, it will develop into an ulcerative-necrotic form.
Diagnosis of lichen planus can be quite difficult. This is explained by the presence of many types of this disease, which have different manifestations. As a result, lichen planus can easily be confused with leukoplakia, candidiasis, and various glossitis. Therefore, differential diagnosis of this disease can be difficult. To confirm the diagnosis, it is necessary to perform a histological examination, which will reveal hyperkeratosis of cells, dystrophy, and Sevatt's bodies.
The principles of treating lichen planus are constantly being improved. New research, experiments and clinical experience allow us to introduce effective methods that bring positive therapeutic results. The list of drug groups used to treat lichen planus includes: sedatives, antihistamines, corticosteroids, adaptogens, herbal preparations. Diet therapy and stabilization of sleep patterns are also of great importance for achieving the desired result.
Prevention
Prevention of white spots on the tongue is possible only in cases where we are talking about pathological processes. After all, physiological plaque is removed without special procedures and does not need prevention. If we talk about spots and plaque that occur with glossitis, leukoplakia, candidiasis, geographic tongue and other diseases, then you should follow several main rules. First, you need to monitor your immunity level. If you know that it is reduced, then consult an immunologist who, if necessary, will prescribe a course of immunocorrection. It is also worth mentioning the gastrointestinal tract, with diseases of which white spots on the tongue often appear. You should eat only healthy food and follow a diet. The general rule of prevention for all diseases is to work on your emotional state. After all, stress is a risk factor for most diseases. As for geographic tongue and geographic tongue, the situation is somewhat different here. There is no specific prevention against these diseases. Therefore, all that remains is to lead a healthy lifestyle, and the likelihood of developing these pathologies will decrease. As statistics show, the prognosis for white spots on the tongue is usually favorable. However, this primarily concerns those diseases that were discussed in the article.
Forecast
A favorable prognosis does not mean that the condition of the tongue mucosa does not require specialist intervention. As mentioned earlier, leukoplakia is a barely noticeable but precancerous condition. Under certain conditions, this formation can become malignant. It is also worth noting that the article only considered the most common conditions with white spots on the tongue. Rare syndromes and specific pathologies also occur. Therefore, you should be attentive to your body and consult with specialists. Be healthy!


 [
[