Medical expert of the article
New publications
Tolosa-Hunt syndrome
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Superior orbital fissure syndrome, pathological ophthalmoplegia - all this is nothing more than Tolosa Hunt syndrome, which is a lesion of the structures in the superior orbital fissure. The process usually involves the orbital vessels (arterial and venous), nerve fibers (oculomotor, trochlear, abducens nerves, as well as the first branch of the trigeminal nerve) and the nearby cavernous sinus. The disease can be classified as a relatively rare and quite difficult to diagnose pathology. [ 1 ]
Epidemiology
Tolos Hunt syndrome was described not so long ago: about 70 years ago. It was studied by the Spanish doctor of neurology E. Tolos. A few years later, the work was supplemented by the Englishman, doctor of ophthalmology W. Hunt. The names of the doctors-researchers became the basis for the name of the syndrome.
Tolosa Hunt syndrome is found equally in men and women. The pathology is usually unilateral and is observed equally often on the left or right side. Bilateral syndrome is possible, but occurs only in isolated cases.
The average age of those affected is 50 years. In general, Tolosa Hunt syndrome can be recorded at the age of 15-85 years. Most patients belong to the elderly age category: the development of the disease is facilitated by multiple cardiovascular disorders, as well as age-related changes in tissues.
The most common symptom of the disease is the manifestation of a classic migraine attack: a person experiences a sudden pulsating headache on one side, “shooting” or “twisting”, with irradiation to the eye socket. Since Tolosa Hunt syndrome lacks typical specific symptoms, the pathology is often called a “neurological chameleon”: diagnostics are complex, requiring differentiation from many other diseases.
Patients with Tolosa Hunt syndrome are periodically found in different countries of the world, without any territorial or seasonal features. The incidence rate is 0.3-1.5 cases per 1 million population. [ 2 ]
Causes Tolosa-Hunt syndrome
In the course of investigating the causes of the development of Tolosa Hunt syndrome, scientists discovered the following facts:
- in most cases, the disease was provoked by immune inflammation of the outer wall of the cavernous sinus;
- in some cases the causes were vascular malformations, tumor processes in the brain (primary and secondary forms), localized cranial pachymeningitis, orbital myositis, periarteritis nodosa, and thrombus formation in the cavernous sinus;
- In approximately 30% of patients, the cause of the disorder cannot be determined, so the diagnosis of idiopathic Tolosa Hunt syndrome was established.
Let us consider these supposed reasons in more detail.
- Autoimmune development of the syndrome is associated with both hypothermia and recent infectious pathologies, as well as with deep stress. The autoimmune form of the disease is characterized by: acute onset, recurrent course, high efficiency of glucocorticosteroid therapy. This form of the disease most often affects men.
- Vascular malformations often occur in decompensated arterial hypertension. Women are more often affected. The disease begins acutely, pain is moderate, with virtually no exophthalmos or chemosis.
- Among the tumor processes capable of leading to the development of Tolosa Hunt syndrome, the most common were primary brain tumors, metastatic tumors with primary foci in the lungs, bronchi, prostate, or metastases of cutaneous melanoma.
- Localized cranial pachymeningitis causes an acute onset of the syndrome in the absence of general cerebral and meningeal signs, without exophthalmos. The diagnosis is confirmed morphologically during biopsy.
- Orbital myositis causes a subacute onset, with intense pain and exophthalmos, pronounced chemosis and double vision.
- Cavernous sinus thrombosis causes total ophthalmoplegia. The diagnosis is confirmed by magnetic resonance imaging.
- Nodular periarteritis can cause the development of Tolosa Hunt syndrome several months after the onset of the disease.
The autoimmune mechanism in most cases underlies the formation of pathology, which has been proven by many specialists. The autoimmune nature is indicated, in particular, by the following factors:
- recurrent course;
- dysmunic disorders;
- protein-cell dissociation in the cerebrospinal fluid and increased levels of proinflammatory cytokines in the cerebrospinal fluid and blood serum. [ 3 ]
Risk factors
Scientists have not yet determined the exact cause of Tolosa Hunt syndrome. But they have managed to identify certain factors that influence the development of such a disorder:
- Genetic predisposition to autoimmune diseases in general. If one of the family members suffered or suffers from an autoimmune disorder, then other relatives may also have similar or other pathologies with a similar development mechanism. This factor is still an assumption that requires additional research and evidence.
- Environmental factors, including dietary habits, environmental conditions, water quality, industrial hazards, etc.
- Severe stressful situations, frequent stress and psycho-emotional shocks, powerful hormonal changes (including pregnancy, menopause, etc.).
- Long-term chronic infectious diseases, including hepatitis, herpesvirus infection, cytomegalovirus, etc.
- Hypothermia, radiation, other strong irritants and damaging factors.
Pathogenesis
The etiological mechanism of the development of Tolosa Hunt syndrome has not been fully elucidated. The determining role is given to autoimmune reactions. Many scientists assume that viral and microbial infections, stressful situations, and radiation act only as a provoking factor. There is no strong evidence of the relationship between the entry of pathogenic microorganisms into the body and the development of Tolosa Hunt syndrome. However, there are suspicions about the involvement of cytomegalovirus in the autoimmune process, which contributes to the formation of granulomas. [ 4 ]
The pathogenetic scheme is caused by the appearance of a local granulomatous inflammatory process in the area of the outer wall of the cavernous sinus, infraclinoid or supraclinoid section of the internal carotid artery, which leads to its narrowing. An important role is also played by the disorder of humoral and cellular immune protection. The humoral side of the syndrome is associated with increased formation of antineutrophil cytoplasmic antibodies acting against the enzymes proteinase-3, myeloperoxidase and a specific membrane protein capable of binding endotoxins. Presumably, cytoplasmic antibodies stimulate existing neutrophils, as a result of which they attack the "target" organs; in particular, the inflammatory process develops in the outer wall of the cavernous sinus.
Cellular changes also play a role in the development of Tolosa Hunt syndrome. This is demonstrated by the predominance of T-lymphocytes, macrophages and plasma cells in granulomas.
There is information about highly active endothelial structures and anti-inflammatory cytokines, which indicates a tendency of the disease process to become chronic.
In isolated cases, focal necrotic changes were noted in the area of the outer wall of the cavernous sinus.
Symptoms Tolosa-Hunt syndrome
Symptoms characteristic of Tolosa Hunt syndrome appear suddenly and unexpectedly for the patient. The main symptoms are considered to be the following:
- Severe pain in the eye socket area, extremely unpleasant, drilling, spreading from the frontal region to the brow ridges, to the eyes and further throughout the head.
- Double vision, which is detected after the onset of pain. It becomes extremely difficult for a person to visually concentrate and examine any object.
- Disorder of the motor function of the eyeball, or so-called ophthalmoplegia, is predominantly unilateral. It can manifest itself to varying degrees, depending on the severity of the pathological process and the extent of the lesion.
- Conjunctival edema.
- Anterior displacement of the eyeball (exophthalmos, “bulging” eyes).
- Deviation of the visual axis of one eyeball to the side, strabismus, which is typical with unilateral nerve damage.
- General deterioration of health, slight increase in temperature, weakness, irritability.
The clinical picture gradually progresses, the symptoms change and worsen, but can disappear as suddenly as they appeared. However, in the absence of the necessary therapy, Tolosa Hunt syndrome again reminds of itself with a relapse.
Neurological symptoms are caused by the local localization of the painful process. Pain occurs as a result of irritation of the first branch of the trigeminal nerve, which passes near the trunk of the oculomotor nerve, and is noted in the area of the orbit, forehead, temple, base of the nose. The intensity of pain varies: from moderate to severe.
Atypical symptoms are possible, which are characterized by the absence of pain. This can be observed when the lesion is localized before the fifth pair enters the cavernous sinus.
Oculomotor disorders usually manifest themselves as double vision during direct gaze.
If the painful process is localized in the orbital apex area, neurological manifestations are often found in combination with visual analyzer disorders. As a result, edema or atrophy of the optic nerve disc occurs, and central scotoma is often observed. Exophthalmos (bulging eyes) and chemosis (conjunctival edema) are possible, the occurrence of which is caused by infiltrative changes in the retrobulbar tissue and difficulties with venous outflow from the orbit.
First signs
Since Tolosa Hunt syndrome has not been studied enough to date, scientists continue to clarify the possible mechanisms of development of this pathology. Taking into account the criteria outlined by the International Neurological Society, the diagnosis of Tolosa Hunt syndrome is justified in the presence of a granuloma of the outer wall of the cavernous sinus, detected during MRI of the brain or biopsy.
The list of signs that are accepted as diagnostic criteria for the syndrome is as follows:
- "picking" or "twisting" pain in one eye socket with subsequent development of muscle paralysis (ophthalmoplegia);
- combined lesions of the oculomotor nerves, the first branch of the trigeminal nerve and the periarterial nerve plexus;
- an increase in the clinical picture over several days (or within 1-2 weeks);
- the possibility of spontaneous remission (in some cases – with residual preservation of defects);
- the likelihood of a relapse of the syndrome, months or years later;
- unchanged systemic picture, no lesions outside the carotid sinus;
- the presence of a positive effect from corticosteroid therapy.
There is another similar diagnostic list of features proposed in 2003. According to this list, Tolosa Hunt syndrome is considered to be the result of the proliferation of granulomatous tissue in the cavernous sinus, superior orbital fissure and orbital cavity:
- one or more episodes of unilateral pain in the orbital area that resolve without treatment for a couple of weeks;
- damage to the cranial nerve (III, IV or VI) in the form of paresis, the presence of a granuloma confirmed by magnetic resonance imaging or biopsy;
- the appearance of paresis simultaneously with pain syndrome, or within 14 days after it;
- disappearance of paresis and pain syndrome within 3 days from the start of corticosteroid therapy.
Forms
In Tolosa Hunt syndrome, the left and right sides are affected with approximately equal frequency, so the pathology is divided into left-sided or right-sided.
The disease is usually unilateral. Bilateral lesions have been observed only in extremely rare cases.
The clinical picture of the disease can develop through the following stages:
- acute or subacute, which occurs after a recent viral infectious disease, hypothermia, a strong increase in blood pressure, sometimes without an obvious reason;
- chronic relapsing, with a gradual increase in symptoms and periodic exacerbations.
In addition, Tolosa Hunt syndrome may be:
- total, with damage to all nerves that pass through the superior orbital fissure;
- incomplete, with involvement in the pathological process of nerves VI, IV, III pairs and I branch of the V pair in various combinations.
With respect to the sinus, anterior, middle and posterior forms of Tolosa Hunt syndrome can be distinguished.
Complications and consequences
Tolosa Hunt syndrome is accompanied by severe pain, which entails loss of sleep, disturbances in the emotional and mental sphere. Sick people become irritable, emotionally unstable. If the necessary treatment is not carried out, then neurotic disorders may appear against this background: depressive states, neurasthenia, hypochondria develop. Work capacity is significantly reduced, the patient becomes withdrawn.
A characteristic feature of Tolosa Hunt syndrome is a relapsing course, which often occurs in autoimmune diseases. The duration of the remission period can be very different: the maximum recorded indicator of asymptomatic duration was 11 years. After treatment, the risk of relapses is significantly reduced. If exacerbations do occur, they are less severe.
Diagnostics Tolosa-Hunt syndrome
Often it becomes difficult for doctors to immediately diagnose Tolosa Hunt syndrome, since the symptoms are very similar to the manifestations of other more common diseases. In most cases, additional consultation with a number of narrow specialists is required: a neurologist, ophthalmologist, endocrinologist, oncologist, neurosurgeon, etc.
At the first stage, it is necessary to exclude malignant diseases, aneurysms, meningitis, etc.
Most often, Tolosa Hunt syndrome is diagnosed by exclusion: the patient undergoes a series of tests to rule out other most likely diseases. The following tests are required:
- detailed blood picture;
- study of the hormonal function of the thyroid gland;
- study of the level of total protein in the blood (to assess the quality of protein metabolism);
- cerebrospinal fluid analysis.
- Instrumental diagnostics involves performing the following diagnostic procedures:
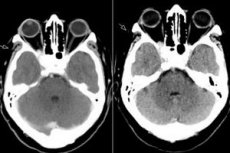
- magnetic resonance imaging of the brain and orbital region, with and without contrast;
- magnetic resonance angiography;
- digital subtraction angiography (intravenous subtraction angiography);
- Computerized brain and orbital tomography with and without contrast.
Gadolinium-enhanced MRI is the modality of choice for the evaluation of THS and can demonstrate abnormal enlargement and enhancement of the CS extending through the superior orbital fissure into the orbital apex. Reported MRI findings on T1-weighted and T2-weighted images are extremely variable and non-specific. MRI plays a key role in diagnosis and helps to exclude other common lesions associated with CS, avoiding the need for invasive high-risk procedures such as SC biopsy, the only way to obtain histopathological confirmation of this disease.[ 5 ]
These studies help to identify traces of inflammatory processes in the cavernous sinus, superior orbital fissure, or orbital apex. Traces of inflammation in the orbital region on cross-sectional images in the absence of cranial nerve palsy are considered more benign in terms of prognosis.
Some patients who are suspected of having Tolosa Hunt syndrome are advised to undergo a biopsy to rule out cancer.
Differential diagnosis
Clinical practice indicates that similar symptoms may be present in many somatic and neurological pathologies:
- in microbial, viral and fungal inflammatory processes affecting the meninges or the outer wall of the cavernous sinus;
- in tumor processes in the brain and orbit - for example, in pituitary adenoma, craniopharyngioma, neurinoma, meningioma of the sphenoid bone wing, in cerebral or orbital metastases;
- in vascular malformations - in particular, in venous-arterial aneurysms, carotid-cavernous fistulas, etc., as well as in dissections of branches of the internal carotid artery;
- for thrombosis, cystic formations of the cavernous sinus, lymphoma;
- for sarcoidosis, orbital myositis (eye muscles), Wegener's granulomatosis (granulomatosis with polyangiitis), ophthalmomigraine, and some blood pathologies.
Differential diagnostics involves working out the possibility of developing all of the above diseases, based on the results of a survey, examination, laboratory and instrumental studies.
Most often, Tolosa Hunt syndrome must be distinguished from the following pathologies:
- blockage of the cavernous sinus by a thrombus;
- Rochon-Duvignod syndrome;
- retrosphenoidal space syndrome (Jacot syndrome);
- paratrigeminal Raeder syndrome;
- cranial polyneuropathy.
Who to contact?
Treatment Tolosa-Hunt syndrome
Tolosa Hunt syndrome responds well to treatment with an immunosuppressive course of corticosteroid hormonal agents. Such drugs are able to suppress the aggressive response of the immune system and its damaging effect on the body's tissues.
The most commonly prescribed drugs are Prednisolone, Methylprednisolone, Cortisone, or alternative drugs that have shown positive effects in the treatment of known autoimmune pathologies. The benefits of steroids are probably related to the antioxidant mechanism and/or the ability of such high doses to reduce edema and subsequent ischemia in the affected areas. [ 6 ]
In addition to corticosteroids, it is appropriate to use painkillers and anticonvulsants. Complex multivitamin preparations are mandatory.
If you strictly follow all the instructions and recommendations of your doctor, the painful symptoms of Tolosa Hunt syndrome are quickly relieved: patients note a marked improvement in their well-being on about the second or third day. In the vast majority of cases, working capacity is maintained. [ 7 ]
Optimal dosages and frequency of taking hormonal drugs are determined on an individual basis. There is no generally accepted treatment regimen, since it is very difficult to organize placebo-controlled studies, which is associated with the low prevalence of the syndrome. Most often, high doses of corticosteroids are recommended, although there have been cases of effectiveness and fairly small doses of drugs (for example, the use of Prednisolone in an amount of less than 0.5 mg / kg per day). Today, the average amount of Prednisolone used in Tolosa Hunt syndrome is 1-2 mg / kg per day.
Approximate treatment plan:
- Methylprednisolone (Solu-Medron 1000 as an intravenous drip infusion with 250 ml of isotonic sodium chloride solution and Panangin (10.0) daily for five days;
- Mildronate for normalization of cellular metabolism, 500 mg by intravenous jet injection daily for 10 days;
- Neuromidin to improve impulse transmission along neuromuscular fibers, 20 mg orally three times a day;
- Clonazepam to enhance the inhibitory effect on the transmission of nerve impulses and stimulation of benzodiazepine receptors, 2 mg orally, and/or Trileptal 150 mg orally before bedtime.
It is possible to prescribe a prolonged course of glucocorticosteroid therapy using high doses of Prednisolone. [ 8 ]
Prevention
It is not possible to prevent the occurrence of Tolosa Hunt syndrome in advance. This is due, at least, to the fact that the causes of the disorder have not yet been clearly determined. If any painful symptoms are detected - in particular, frequent pain in the frontal region and eye sockets, double vision and weakening of the eye muscles, then you should contact the appropriate specialist as soon as possible and conduct a full diagnosis.
Secondary prevention is aimed at preventing relapses in patients with already diagnosed Tolosa Hunt syndrome. Important points of preventive actions are:
- regular medical consultations, diagnostic procedures, and specialist outpatient monitoring;
- periodic courses of corticosteroid therapy;
- strengthening and maintaining an adequate state of the immune system.
All those who are sick should try to avoid stressful situations and promptly treat any inflammatory processes in the body.
Forecast
The prognosis for Tolosa Hunt syndrome is considered favorable. There is a good response to corticosteroid therapy, cases of spontaneous remission are common, although some patients experience residual effects in the form of impaired function of the damaged eye muscles. If left untreated, the disease subsequently becomes recurrent. In patients who have received treatment, relapses are observed in approximately 35% of cases. [ 9 ]
After completion of the therapeutic course, working capacity is usually restored. However, this applies to a correctly diagnosed disease, and not to other pathologies that develop under the “mask” of the syndrome. [ 10 ]
Disability is observed only in rare cases. Only with documented frequent exacerbations is it possible to assign the third group of disability. In difficult cases, the patient is transferred to light work, which is not accompanied by visual loads. If Tolosa Hunt syndrome is of a persistent recurrent nature, then the person is not recommended to drive vehicles, which is due to impaired motor function of the eyeballs and diplopia.

