Medical expert of the article
New publications
Tendinopathy
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
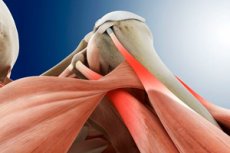
Tendinopathy is a general medical term that refers to damage or abnormal changes in the tendons (tendons). Tendons are the tissues that connect muscles to bones and allow force to be transferred from muscles to bones, allowing joint movement. Tendinopathy can occur as a result of various types of trauma, overuse, inflammation, or natural aging.
There are different types of tendinopathies, and they can affect the tendons of different parts of the body.
Treatment depends on its type, severity, and location. It usually involves rest, physical therapy, ice application, anti-inflammatory medications, injections, and in some cases, surgery. It is important to see a doctor for proper diagnosis and treatment of tendinopathy to prevent further damage and return to normal activity.
Causes of the tendinopathies
Tendinopathy can occur due to a variety of causes, and these can vary depending on the specific area where the tendon is injured. Some of the common causes include:
- Overloading and overloading: One of the most common causes of tendinopathy is excessive physical activity or improper movements that can overload the tendons. This often occurs in athletes or people who perform repetitive movements for long periods of time.
- Trauma: Injuries such as bumps, falls, or sprains can cause tendon damage and contribute to tendinopathy.
- Improper movement technique: Proper exercise and movement technique is important to prevent tendinopathy. Improper execution of movements can put additional stress on the tendons.
- Age: As we age, the tissues of the body, including the tendons, become less elastic and more susceptible to damage. This makes older people more susceptible to tendinopathy.
- Specific sports: Certain sports, such as tennis, golf, basketball, or running, can put increased stress on certain tendons, which contributes to tendinopathy.
- Other Risk Factors: Certain medical conditions such as obesity, diabetes, arthritis, and hormonal disorders may increase the risk of tendinopathy.
Symptoms of the tendinopathies
Symptoms of tendinopathy can vary depending on the location of the lesion and severity, but include the following common signs and symptoms:
- Pain: This is one of the main symptoms of tendinopathy. The pain may be sharp, aching, localized in the area of the affected tendon and may be intensified by movement or application of load to the involved muscle.
- Order of pain: Pain often occurs with specific movements or activities associated with the affected tendon. For example, in patients with Achilles tendinopathy (lesion of the tendon of the plantar muscle), pain may increase with walking or running.
- Swelling: Swelling can develop in the area of the affected tendon, which can worsen pain and limit the mobility of the joint.
- Compression and stiffness: In some cases, tendinopathy can cause a feeling of stiffness or compression in the area of the affected tendon. This can lead to a decreased range of motion in the joint.
- Feelingof weakness: A tendon injury can cause a feeling of weakness in the muscle involved. This can affect the ability to perform certain movements or activities.
- Worsening with exertion: Symptoms of tendinopathy mayworsen with vigorous movement or exercise.
- Duration of symptoms: Sym ptoms of tendinopathy may develop gradually and get worse over time. They may be more pronounced after physical activity and improve at rest.
- Location: Symptoms depend on which tendon is affected. For example, shoulder tendinopathy can cause pain and restriction of motion in the shoulder, while elbow tendinopathy can cause pain and restriction of motion in the elbow area.
Forms
- Tendinopathy of the supraspinous tendon: This condition involves damage to the tendon that is associated with the muscles of the upper arm and shoulder, including the deltoid muscle. It can cause pain and discomfort in the shoulder and upper arm, especially with shoulder movements.
- Tendinopathy of the plantar muscle: This is an injury to the tendon of the plantar muscle, which connects to the top of the shoulder blade and the top of the upper arm. Tendinopathy of this area can cause pain and restriction of movement in the shoulder joint.
- Shoulder tendinopathy: This condition is associated with damage to the tendons that run through the shoulder joint. It can lead to pain in the shoulder and upper arm, especially when lifting the arm up.
- Gluteal muscle tendinopathy: This condition is associated with damage to the tendons of the muscles located in the buttock area. It can cause pain and discomfort in the buttock area, especially when walking or moving the legs.
- Knee tendinopathy: This is a condition in which the tendons associated with the knee joint become damaged or inflamed. One common type of knee tendinopathy is patellar tendinopathy, in which the tendon that connects the patella and the femur is affected.
- Tendinopathy of the hand: May involve affecting the tendons in the wrist or fingers. This can cause pain, limitation of movement, and even joint deformity.
- Tendinopathy of the foot: The foot contains many tendons, and tendinopathy of the foot may involve damage to the tendons connecting to the heel bone or metatarsal bones. This can cause walking pain and discomfort.
- Degenerative tendinopathy: This is a type of tendinopathy that is associated with the aging process and degeneration of the tendons. It can develop slowly and lead to gradual deterioration of the tendons.
- Calcifying tendinopathy: In this case, calcium deposits form in the tendon, which can cause pain and restriction of movement. This most commonly occurs in the shoulder joint, but can occur elsewhere as well.
- Insertional tendinopathy: This type of tendinopathy involves affecting the area where the tendon attaches to the bone (insertion). It can occur in various parts of the body and can cause pain and limitation of movement.
- Hip muscle tendinopathy: May involve damage to the tendons associated with the thigh muscle or other muscles in the hip area. This condition can cause pain and restriction of movement in the hip and may be associated with overuse or other factors.
- Rotator Cuff Tendinopathy: Usually refers to damage to the tendons that form the cuff of the shoulder joint. This condition can cause pain and restriction of motion in the shoulder and may be associated with injury or excessive stress on the shoulder joint.
- Biceps tendinopathy: Associated with damage to the biceps tendon, which runs through the shoulder joint. This can cause pain and restriction of movement in the upper arm and shoulder.
- Quadriceps tendinopathy: This tendinopathy is associated with damage to the tendons of the quadriceps (quadriceps) muscle. It can cause knee pain and limitation of movement.
- Hip tendinopathy: May involve damage to the tendons associated with the hip joint. This can cause pain and discomfort in the pelvis and hip area.
- Tendinopathy of the hamstring muscle: May involve damage to the tendons associated with the muscles of the back of the thigh. This can cause pain and restriction of movement in the hamstring area.
-
Tendinopathy of the patellar collateral ligament:
- This condition is characterized by damage or inflammation of the patella's own ligament, which connects the thigh and lower leg.
- Usually occurs due to overuse, injury or overloading of the tendon.
- Symptoms may include pain, swelling, and restricted movement in the patella area.
-
Cruciate ligament tendinopathy:
- The cruciate ligaments (anterior and posterior cruciate ligaments) are located in the knee joint and serve to stabilize it.
- It can result from torn or damaged ligaments, which often occurs in sports injuries or accidents.
- Symptoms may include pain, swelling, knee instability and restricted movement.
-
Achilles tendinopathy:
- The Achilles tendon is located in the heel area and is used to elevate the heel when walking and running.
- May develop due to overloading, unsuitable footwear, changes in foot architecture, or other factors.
- Symptoms may include pain, swelling and restricted movement in the heel and calf muscles.
-
Tendinopathy of the subscapular muscle:
- The subscapularis muscle (tendon of the subscapularis muscle) is located in the shoulder area and plays an important role in the movement of the shoulder joint.
- Can develop due to improper movement, overload or injury.
- Symptoms may include pain, restricted movement in the shoulder, weakness and discomfort when lifting the arm.
Diagnostics of the tendinopathies
Diagnosing tendinopathy, that is, tendon disorders, involves a number of methods and clinical signs that help the physician determine the presence and nature of the injury. Here are some of them:
- Medical history: The physician begins the diagnosis by asking the patient questions about symptoms, chronic or repetitive injuries, physical activity, occupational characteristics, and other factors that could contribute to the development of tendinopathy.
- Physical Exam: The physician performs a physical examination, assessing the condition of the tendon and surrounding tissues. The doctor may look for signs of inflammation, swelling, painful points, restriction of movement, etc.
- Clinical Symptoms: Patients with tendinopathy may experience pain, soreness, stiffness, swelling, or other symptoms in the area of the affected tendon.
- Movement patterns: Certain movements or loads can cause or increase the symptoms of tendinopathy. This can be used for diagnosis.
- Instrumental Investigations:
- Ultrasound (USG): Ultrasound can visualize tendon structures and determine the presence of changes such as thickness, inflammation, and degenerative changes.
- Magnetic resonance imaging (MRI): An MRI can provide more detailed information about the condition of the tendons and surrounding tissues.
- Radiography: X-rays can be helpful in identifying bony changes associated with tendinopathy.
- Lab tests: Lab tests, such as general blood work and biochemistry tests, can help rule out other possible causes of pain and inflammation.
Differential diagnosis
The differential diagnosis of tendinopathy involves identifying and distinguishing this condition from other medical problems that can cause pain and discomfort in the tendon and joint area. It is important to properly diagnose tendinopathy in order to begin appropriate treatment. Below are some of the conditions and problems that may resemble tendinopathy and require differential diagnosis:
- Joint inflammation: Inflammation of a joint, such as arthritis, can cause pain and discomfort in the vicinity of the tendons. Differential diagnosis may include joint examination and joint fluid analysis.
- Synovitis: Synovitis is an inflammation of the joint lining that may be accompanied by tendon pain. Examination of the joint and clinical signs may be required for differential diagnosis.
- Neuropathy: Some neuropathies, such as carpal tunnel syndrome or cubital tunnel syndrome, can cause symptoms resembling tendinopathy in the hand and wrist. A neurologic examination may be helpful for differential diagnosis.
- Vascular disease: Some vascular diseases can cause pain and changes in the blood supply to the tissues, which can mimic the symptoms of tendinopathy. Instrumental techniques such as ultrasound or angiography may help in diagnosis.
- Cancer: In rare cases, malignant tumors may affect the tendons or tissue adjacent to them and cause pain and discomfort. Differential diagnosis may include examination and biopsy of the tumor.
- Other Medical Conditions: Other conditions such as infections, systemic diseases, or metabolic disorders can cause joint and tissue pain that may be similar to the symptoms of tendinopathy.
For differential diagnosis and to determine the exact cause of tendon pain and discomfort, it is important to perform an extensive examination and, if necessary, consultations with various specialists such as a rheumatologist, neurologist, orthopedist, or surgeon.
Who to contact?
Treatment of the tendinopathies
Treatment of tendinopathy depends on the location and severity of the lesion, but may include the following:
- Rest and activity restriction: The first step in treating tendinopathy may be to limit the activity that is causing or exacerbating symptoms. Rest allows the tendons to recover and avoid further damage.
- PhysicalTherapy: Physical therapy plays an important role in the treatment of tendinopathy. Physical therapy specialists may prescribe exercises to strengthen muscles and tendons, as well as techniques such as ultrasound therapy, laser therapy, and massage to speed recovery.
- Non-steroidal anti-inflammatory drugs (NSAIDs): Your doctor may prescribe medications such as ibuprofen to reduce pain and inflammation. However, they should be used with caution and as recommended by your doctor.
- Injections: In some cases, injections such as steroid injections or protein injections into the painful area may be given to reduce inflammation and pain.
- Muscle Strengthening and Stretching: A physical therapist can help develop an individualized exercise program to strengthen the muscles surrounding the affected tendon and stretch to improve mobility.
- Use of orthotic aids: Orth otics or bandages are sometimes used to reduce stress on the affected tendon and provide support.
- Laser and ultrasound treatment: Some physical therapy modalities, such as laser and ultrasound therapy, can help improve blood flow and speed recovery.
- Surgery: In some cases, if conservative methods are ineffective and tendinopathy becomes chronic or severely limits the patient's life, surgery may be required.

