Medical expert of the article
New publications
Cervical surgeries
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Cervical hysterectomy is indicated for women when there is laboratory confirmation of non-invasive cancer. In this disease, only the cervix is affected, and regional lymph nodes and adjacent organs are not damaged. There is only one way out - it is necessary to completely remove the altered cells of the mucous membrane to prevent progressive development of the tumor.
During surgical intervention, a cone-shaped fragment of the cervix surface is removed, as well as part of the cervical canal. The removed area is subjected to careful examination (laboratory research) in order to identify atypical (degenerating into cancer) cells. Surgical removal of affected tissues is also necessary if a woman is diagnosed with cervical erosion, which, if treated incorrectly, can "degenerate" into cancer. In modern medicine, a gentle radio wave method (radioknife) is used, which allows for quick and painless removal of the affected area of the mucous membrane.
Before the surgery, the woman is examined, a biopsy is prescribed, as well as a CT and MRI. According to statistics, cervical ablation is one of the most common surgeries today. For example, in America, it ranks second after cesarean section. Naturally, gynecological surgery is performed strictly according to medical indications.
Indications for cervical ablation surgery
Cervical ablation surgeries are indicated in cases where pathological areas covering part of the cervical canal are detected on the mucous membrane. Such changes may relate to many conditions that require intensive care and the following diagnostic actions.
Indications for cervical ablation surgery include both minor cell pathologies (erosions) and an obvious tumor (cancer). A PAP test is often used to diagnose the disease, i.e. a cytological smear to detect atypical cells, which helps to detect both precancerous and cancerous changes in cervical tissues in a timely manner. Such a study is recommended to be done annually for all women, especially those who are at risk. For example, when stage II-IV cervical dysplasia is detected, there is reason to talk about a precancerous condition, when the cells become atypical, i.e. acquire other functions that are not characteristic of them. Dysplasia is dangerous because it most often occurs without pronounced symptoms, which is a threat to health. If the disease is not diagnosed in a timely manner, cervical cancer may develop.
Let us consider the indications for the use of specific methods aimed at excision of the cervix when dangerous pathologies are detected.
- Knife amputation is indicated in case of detection of the first stage of cancer. The operation is performed using a scalpel and involves excision of the cervix with subsequent removal of its part, as well as parametrium tissue and the upper part of the vagina. The advantage of this method is the complete preservation of the woman's reproductive function.
- Radio wave conization is used in case of diagnosing serious diseases such as dysplasia or cancer. Special instruments are used to remove the damaged organ: a diathermoelectrosurgical device and an electrode (Game-Rogovenko), with which you can easily adjust the length of the radio wave in accordance with the anatomical features of the cervix. It should be noted that this method has contraindications: pathologies of the organ structure, acute inflammatory process, leukocytosis, etc.
- Laser amputation (used for dysplasia or benign tumors). The surgeon cauterizes the area where the tumor is located. Over time, scar tissue forms in this area.
- Cryodestruction (the affected tissue area is exposed to liquid nitrogen, under the influence of low temperature the cell membranes are destroyed and the tissues die). This method is contraindicated in inflammatory processes and endometriosis.
- Ultrasonic amputation (almost the same as laser amputation, the only difference is that ultrasound is used to remove tissue).
- The radiosurgical method (radio waves have a destructive effect on cells) using the American device "Surgiton" is considered the safest and most effective method.
During the postoperative period, the patient is under the supervision of medical personnel. She is prescribed painkillers and antibiotics. After discharge, physical activity should be minimized, hot baths should be avoided, as well as sexual intercourse.
Preparation
Cervical ablation surgeries are performed according to the indications of a gynecologist when a woman has serious pathologies such as erosion, non-invasive cancer, chronic endocervicitis. Before surgery, it is necessary to undergo a full medical examination, i.e. take blood tests (general, biochemical) and urine tests, as well as a biopsy and colposcopy. If necessary, the patient is prescribed an ECG, ultrasound of the pelvic organs, smear testing for the presence of atypical cells and other additional studies.
Preparation for the operation begins several days before the scheduled date, and if the patient has chronic endocervicitis, then conservative treatment is carried out: vaginal baths, douches and tampons with the use of medicinal solutions.
Immediately before the procedure, mucus is removed from the cervical canal using a probe wrapped in sterile gauze or cotton wool, previously moistened with a 10% soda solution. Then the cervical canal is lubricated with iodine tincture. Preparatory manipulations should also include sanitary treatment: hair removal from the pubic area, a hygienic shower and bowel cleansing (the patient takes a laxative for 2 days).
Today, doctors resort to several methods of performing cervical amputation operations:
- cold knife conization;
- cone electroexcision;
- ultrasonic amputation;
- cryodestruction;
- radiosurgical method;
- laser amputation.
During the preoperative period, the woman undergoes psychoprophylactic preparation and also takes medications (sleeping pills and sedatives). More intensive planned preparation takes place in a hospital setting (for 1-3 days). An anesthesiologist consultation is held, a number of studies that were conducted on an outpatient basis (coagulogram, blood test) are repeated, and the optimal method of pain relief is selected. In each specific case, preoperative preparation is determined by the scope of the operation and the patient's condition.
Technique of implementation
Cervical ablation operations take an average of 15-30 minutes, depending on the severity of the pathology and the amount of work to be done. The following operations can be performed on the cervix: cryodestruction and conization, removal of polyps, diathermoexcision, diathermocoagulation, as well as amputation and plastic surgery.
The technique of the operation depends on the chosen method. For example, radio wave conization uses a colposcope, diathermoelectrosurgical apparatus and an electrode. First, the surface of the cervix is anesthetized (local anesthesia is administered). Then, at a distance of 3-5 mm from the affected area, an electrode loop is fixed and high-frequency alternating current is directed, resulting in the removal of the pathological area of tissue. In order to prevent postoperative infectious exacerbation, the patient is prescribed antibacterial and general strengthening complexes.
Laser vaporization involves vaginal sanitation, which involves the complete removal of mucus from the cervical canal. Pain is blocked using intracervical anesthesia. For this purpose, a solution of lidocaine and epinephrine can be used. In some cases, the operation can be performed without anesthesia. The doctor uses Lugol's solution to mark the surgical field. A colposcope is used to visualize and control the laser. The power value is 20-25 W, the beam diameter can reach up to 2.5 mm. The laser's effect on tissues begins from the posterior lip of the cervix, the depth of penetration of the laser beam depends on the tissues to be treated. Thus, when irradiating the cervical canal, this figure can be 7 mm.
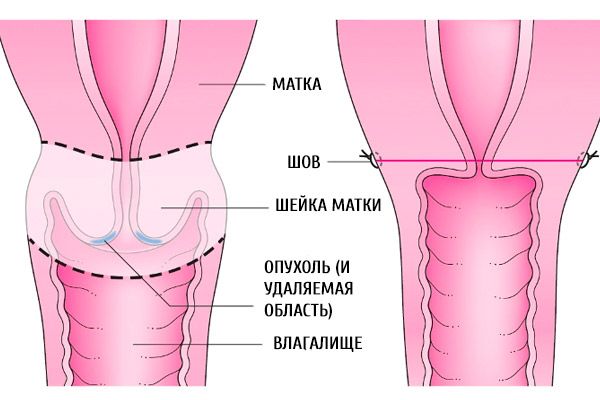
Cone-shaped amputation is performed in the presence of hypertrophy or anatomical deformations of the cervix. The technique for performing the operation is as follows. Using gynecological mirrors, the vagina is opened, after which part of the cervix is grasped with forceps and released downwards. Then a circular opening of the mucous membrane is performed, approximately 1 cm above the pathological tissue. Using a scalpel, the tissue is conically excised and removed. After this, V-shaped sutures are applied, and the cervical canal is formed.
Wedge excision of the cervix is indicated when ectropion (eversion of the mucous membrane) is detected. At the beginning of the operation, the vaginal part of the cervix is opened from different sides of the canal, the depth of which will depend on the expected volume of amputation. Wedge excision of the anterior lip of the cervix is performed, after which its edges are sutured with separate sutures. Similar manipulations are performed with the posterior lip of the cervix, including its suturing with special catgut sutures. Then lateral sutures are applied, and the patency of the cervical canal is checked with a probe.
It should be noted that in the postoperative period, unpleasant consequences such as nagging pain and bloody discharge may be observed, which on average last up to 20 days and do not signal danger. After vaporization of the cervix, a woman must abstain from sexual intercourse for at least one month. Reliable test results (colposcopy, cytology scraping and HPV detection test) will be ready approximately two months after the surgical intervention.
Cavity surgery to remove the cervix
Cervical ablation operations can be abdominal, i.e. performed during the removal of the uterus itself if the woman has been diagnosed with uterine cancer. The word "abdominal" means that the operation will be performed directly on the organs located in the abdominal cavity. The danger is that such operations violate protective barriers, which requires special measures to comply with the rules of antisepsis and asepsis.
Abdominal surgery to remove the cervix most often occurs when there is a need to remove the uterus with a large tumor that cannot be removed by another method. Accordingly, the entire organ is removed, along with the affected areas, including the cervix. Unfortunately, this type of surgery involves severe blood loss, which increases the risk of infection in the postoperative period. Rehabilitation after abdominal surgery is long and averages 6 weeks.
As for the algorithm for performing abdominal surgery, it includes general anesthesia, which ensures complete immobility and pain relief during the procedure. In the absence of contraindications, the patient is given general anesthesia. Then, the stages of surgical access to the organ, manipulations with the damaged organ and tissues, and suturing the wound (layer-by-layer closure) are carried out sequentially. A suture (vertical or horizontal) approximately 20 cm long will remain at the incision site. For better tissue healing, the woman is recommended to wear a postoperative bandage.
How long does cervical ablation surgery take?
Cervical ablation operations are performed when a pathological process is detected that requires immediate surgical intervention. This may be follicular hypertrophy, chronic endocervicitis, ectropion, tumor (cancer) and other pathological processes.
How long does a cervical ablation surgery last? Many women who are preparing for the surgery are interested in this question. The answer will be different in each individual case. The duration of the procedure depends on the anesthetic used, the age and individual characteristics of the female body, the diagnosis of the disease, as well as its severity, the qualifications of the surgeon and a number of other factors.
On average, the time of such an operation is 10-15 minutes, but with diathermoexcision of the cervix - a little longer, which is explained by the careful preparation of special equipment and the patient herself. The operation to remove cervical polyps lasts only a few minutes and does not require a long rehabilitation period. Amputation of the cervix through vaginal access lasts about 1 hour, hysterectomy - a little longer, removal of the uterus with appendages can take from 1 to 2 hours, which is explained by the significant volume of the operation.
If we talk about cases related to a malignant tumor, the operation can last several hours. Everything depends on the expected scope of surgical intervention, the need to collect material for histology and other tests, possible complications during the operation, etc.
Consequences
Cervical ablation surgeries may have negative consequences that arise as a result of various complications. First of all, it is necessary to note the risk of repeated surgical intervention due to bleeding caused by mechanical damage to the mucosa when using surgical instruments or insufficient hemostasis. In such a case, there is a need to duplicate the operation.
The consequences may concern infectious complications: the development of sepsis, peritonitis and suppuration of hematomas. In the postoperative period, a woman may experience vaginal bleeding and necrosis of the vaginal dome. It is also possible to develop a disease called "endometriosis", in which cells of the uterine mucosa may be found in other reproductive organs.
The consequence of radio wave conization of the cervix is bloody discharge before menstruation. In rare situations, such a procedure becomes an obstacle to conception and further bearing of a child due to adhesions and sutures that arise after the operation. If conization is performed using a laser, the risks of negative consequences are minimized. Successful operation to amputate the cervix will not affect the woman's reproductive function in the future.
With multiple conizations, problems of early miscarriage, premature pregnancy, or inability to conceive a child may arise. However, this is rare.
Complications after cervical ablation surgery
Cervical amputation surgeries are often accompanied by various complications associated with bleeding, purulent infections, and sepsis. In rare cases, when the surgery is performed by an unqualified doctor, such a complication as vaginal dome necrosis may develop. To exclude unpleasant consequences, the gynecologist prescribes a routine examination for the woman. Thus, after two weeks from the surgery, you should be completely sure that the rehabilitation is going smoothly. It is very important that every woman who has undergone cervical amputation surgery visits a gynecologist at least once every 3 months for examination and regular vaginal smear testing for cytological examination.
Complications after cervical ablation surgery can be of different nature. The most common of them are listed below.
- Bleeding from the vagina (surgical wound). Usually observed in the first hours and days after the operation, most often due to poorly performed hemostasis.
- Bladder injury. Occurs with high amputation of the cervix due to incorrectly performed technical techniques at individual stages of the operation (incision, suturing, etc.).
- Narrowing or closure of the cervical canal. This complication may occur during suturing, so the patency of the cervical canal must be checked with a probe.
- Damage to the peritoneum of the rectal pocket during excision of the cone due to the surgeon's carelessness.
In addition, when suturing the rigid tissues of the cervix, the surgical needle may break and its fragment will remain in the tissue. This leads to unnecessary tissue trauma, so it is important to use strong needles that are long enough.
Rehabilitation period
Cervical ablation operations are performed in hospital conditions and require the use of special medical equipment and instruments. In the first hours after the operation, the patient will be under the supervision of medical staff. Then she will be transferred to a regular ward and prescribed painkillers to relieve pain. Antibacterial agents are used to prevent possible infections. On average, a woman can stay in the hospital for 6-7 days - everything depends on the success of the rehabilitation, the presence or absence of complications, and the general well-being of the patient.
The rehabilitation period may be accompanied by such unpleasant sensations as fatigue, dizziness, weakness, general malaise, pain, etc. Therefore, a woman needs to limit physical activity as much as possible and return to normal life gradually.
For 6 weeks, you should abstain from sexual intercourse and taking contraceptives, and avoid water procedures (swimming, taking baths, etc.). It is not recommended to use hygienic tampons to avoid infection of the wound. Usually, in the first week after the operation, a woman experiences bloody discharge of a dark brown color. If they acquire a different shade and become more abundant, you should immediately contact a gynecologist. On average, the rehabilitation period lasts for 4-6 weeks, after which you can return to work and your normal lifestyle.
Cervical ablation operations are serious procedures that require a special approach and selection of optimal methods aimed at eliminating pathology and the woman's full recovery. Two weeks after surgery, it is necessary to visit a gynecologist for an examination. The next time, the doctor will take a smear for cytological examination, as well as perform a colposcopy and magnetic resonance imaging. For 5 years, a woman should undergo a gynecological examination every 3 months.


 [
[