Medical expert of the article
New publications
Serozocele
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
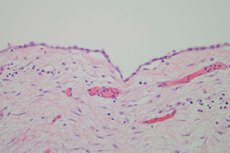
When doctors detect accumulation of serous fluid in any of the body cavities or under the skin, they talk about serozocele. This neoplasm can be localized in any area of the small pelvis and is most often caused by surgery, acute inflammatory process, endometriosis, peritonitis, etc. Another possible name for serozocele is inclusion cyst.
Epidemiology
Serosocele is a fairly common pathology that can occur at almost any age. However, the problem is most often diagnosed in women aged 30-45.
The moisture that accumulates in the tissues is transparent and light yellow. In case of complications, pus or blood may be found in the fluid.
Serosocele rarely poses a threat to the patient's life: this disease is not prone to malignant degeneration, and timely treatment helps to completely get rid of the pathology without any negative consequences.
Causes serocele
Serosocele is often diagnosed in female patients, shortly before menopause. However, there are other reasons for the development of the pathology:
- Inflammatory processes affecting organs located in the pelvis (salpingo-oophoritis, endometritis, peritonitis, parametritis, prolonged presence of an IUD, repeated abortions and curettage, sexually transmitted infections - all these factors cause fibrinous "sticking" of tissues, the formation of adhesions and the accumulation of fluid in the inter-adhesive space).
- Surgical interventions on the pelvic organs and abdominal cavity (hysterectomy, appendectomy, etc.).
- Trauma to abdominal organs, intra-abdominal bleeding.
- Endometriosis.
Even a simple surgical intervention can trigger fluid accumulation. But most often the problem develops after removal or structural changes of organs.
Serocele is often detected after the following surgeries:
- contour plastic surgery (facelifts, liposuction, etc.);
- breast augmentation surgery, mastectomy;
- hernia repair;
- Abdominal plastic surgery.
Risk factors
There are many known factors that can help predict the risk of developing serozocele.
- Heredity plays a significant role. The risk of the disease increases if close relatives have been diagnosed with genital or extragenital tumor processes.
- Patients with serozocele often have a history of chronic tonsillitis and childhood infectious pathologies (scarlet fever, measles). It has been proven that toxic infections have a negative effect on the genitourinary system, reducing the body's resistance to various pathologies and creating favorable conditions for the occurrence of metabolic disorders.
- Patients with serozocele are often diagnosed with extragenital pathologies, such as diseases of the cardiovascular system (more than 17%), endocrine system (about 16%), digestive tract (about 14%), and hepatobiliary system (more than 14%). [ 1 ]
- Patients with serocele often have a history of prolonged infertility, spontaneous abortions, and medical abortions.
Surgical interventions that can trigger the formation of serozocele include appendectomy, cesarean section, hysterectomy, and operations on the intestines or ovaries.
Pathogenesis
Serosocele is a benign neoplasm located in the pelvic area. In such a formation, moisture accumulates without signs of an inflammatory process.
A cyst can have different sizes, depending on the amount of fluid in it – from several millimeters to several centimeters.
Serosocele is called an inclusion cyst. The neoplasm has a spherical, oval or irregular configuration and can have one or more chambers. The walls, membranes or partitions are adhesions formed as a result of inflammatory processes or surgical operations.
The cavity is filled with a light yellow liquid: its volume usually ranges from ten milliliters to a liter.
Serosocele can form in any cavity space affected by adhesive changes. However, the problem is most often found in the area of the uterus and appendages.
Symptoms serocele
Serosocele is detected mostly by chance, since the symptoms of the disease are non-specific. Even after listening carefully to the patient's complaints, it is almost impossible to immediately diagnose "serosocele". The pathology in the vast majority of cases is asymptomatic, and sometimes manifests itself as chronic pelvic pain syndrome - chronic pelvic pain. The patient may complain of lumbar and spinal pain, a pulling sensation in the lower abdomen. The pain tends to increase as a result of hypothermia, physical exertion, stress. Women often experience irregularities in the menstrual cycle, painful PMS, etc. Unpleasant and even painful sensations during sexual intercourse are not uncommon. The pain can be quite severe: some women are forced to give up sexual activity because of this.
Regular pain gradually "exhausts" the nervous system, negatively affects performance and the state of the immune system. In some cases, reproductive capacity also suffers: often women with serozocele seek medical help due to the inability to get pregnant.
The first signs of serozocele often go unnoticed, so the pathology is classified as difficult to diagnose. Only during a routine ultrasound can the presence of a pathological formation be seen. Palpation can detect the problem only when it reaches significant sizes, exceeding 15-20 centimeters.
Stages
Symptoms of serozocele often depend on the size and location of the neoplasm, as well as on the stage of the pathological process.
- The acute stage is rare: patients complain of dyspepsia, elevated body temperature, tachycardia. The abdomen is painful on palpation.
- The intermittent stage is characterized by periodic pain and/or intestinal and menstrual cycle disorders.
- The chronic stage occurs most often. It is characterized by hidden symptoms, rare nagging pains, and infertility.
Forms
Neoplasms are classified depending on the cause, localization of the process, and its size.
The main factor in the formation of serozocele is the adhesion process, which occurs for various reasons. It is between the adhesions that a cystic formation with liquid contents develops, which disrupts the functioning of internal organs, intestines, etc.
Serocele in the pelvis after surgery often appears in cases where prevention of adhesions was not carried out during the rehabilitation period. The pathology can form after an ectopic pregnancy, cesarean section, appendectomy, etc. [ 2 ]
Serocele of the ovary is often a consequence of inflammatory processes - adnexitis, salpingo-oophoritis. At the site of a prolonged inflammatory process, adhesions are formed, which become a kind of framework on which a cystic formation is subsequently built. In some cases, the problem develops after the removal of ovarian cysts.
Serosocele of the uterus may be the result of parametritis, endometritis, pelivioperitonitis, or caused by the use of an intrauterine device for a long time, curettage, multiple artificial terminations of pregnancy, infection of the reproductive organs. During the inflammatory process, fibrin accumulates on the peritoneal surface, and closely located tissues stick together. As a result, an adhesive process develops, and serous contents accumulate in the formed interadhesive space - this is a pathological neoplasm. [ 3 ]
For the correct treatment, it does not matter whether the serozocele is found on the left or right. What is important is the degree and intensity of the cyst growth, the presence of symptoms, and how much the tumor interferes with the function of other pelvic organs.
Since the right ovary is located in close proximity to the appendix (aka the vermiform appendix), then with appendicitis, the inflammation can easily spread to the ovary, which will subsequently cause the appearance of a serocele on the right. In some cases, doctors have to differentiate the symptoms of appendicitis from the signs of a cystic formation in the right ovary. [ 4 ]
If a serocele with a parietal element is detected, then to exclude a malignant process, a study on the CA-125 tumor marker is mandatory. [ 5 ]
Often, along with serozocele, a fluid accumulation of more than 50 ml is found in the retrouterine space. In such a situation, the woman should be examined thoroughly. In particular, the fluid may be the result of a cyst leak, or the so-called opening of the cyst. A small volume of fluid (up to 50 ml) without additional inclusions (for example, blood) is considered a normal variant.
Complications and consequences
Despite the apparent harmlessness of serozocele, this disease can lead to serious complications, including a bend in the cervix, menstrual irregularities, ectopic pregnancy, etc. This occurs because the neoplasm can contribute to the displacement of the pelvic organs and impair their functionality. [ 6 ]
Serosocele is a kind of abdominal cyst - it is a serous fluid that accumulates between adhesions. After a puncture or even after removal of the cyst by surgery, the same neoplasm can form at the site of the adhesion process.
Can a serozocele disappear? This scenario is also possible. For example, when adhesions soften, the contents of the cyst can flow out. In this case, its walls collapse and it actually disappears from the field of view of ultrasound monitors. However, according to statistics, a “disappeared” cyst has a high chance of appearing again - this happens in about half of the cases.
Can a serocele burst? A rupture of the neoplasm is unlikely, but it is impossible to completely exclude such an outcome. Usually, the cyst is regularly monitored and, in case of its critical growth, the patient is sent for surgery. Small seroceles, as a rule, cannot burst. But medical monitoring of tumor growth should be mandatory.
Diagnostics serocele
The following diagnostic measures are considered mandatory:
- laboratory tests (complete blood count with determination of total protein, creatinine and urea, bilirubin, liver enzymes, blood sugar; serological blood test with Wasserman reaction, determination of Rh factor, HbSAg; complete urine analysis, CA-125 assessment);
- instrumental diagnostics (vaginal and rectovaginal examination, diagnostic uterine curettage with histological examination, ultrasound of the pelvic organs and abdominal cavity, chest X-ray, fibrogastroduodenoscopy, colonoscopy to exclude metastatic lesions of the appendages, CT and/or MRI of the abdominal organs).
In patients under 30 years of age, β-chorionic gonadotropin and α-fetoprotein are determined.
The basic diagnostic method for serozocele is ultrasound examination. The disease is characterized by proliferation of peritoneal mesothelium, which is clearly visible during transabdominal ultrasound and MRI of the pelvis.
Differential diagnosis
Differential diagnosis of serocele is usually carried out with the following painful processes:
- paraovarian cystic formation;
- hydrosalpinx (fluid accumulation in the fallopian tube);
- pyosalpinx (purulent accumulation in the fallopian tube);
- appendix cyst (mucocele).
If partitions are found in the neoplasm, then serocele should be distinguished from chamber peritoneal mesothelioma and malignant processes in the ovaries.
If there is the slightest suspicion of oncopathology, it is imperative to perform a biopsy of the formation.
Who to contact?
Treatment serocele
In the absence of symptoms and complaints from the patient, there is no need to rush to treat serozocele: the doctor prescribes regular examinations and ultrasound monitoring of the dynamics of the neoplasm every 6 months. If serozocele is diagnosed in a pregnant woman, there are considerable risks of circulatory disorders in the fetus, so ultrasound is performed 1-2 times a month.
If the patient indicates severe pain, then the only radical solution to the problem is surgery. [ 7 ] Physiotherapy may be prescribed as an addition.
Drug treatment usually includes taking anti-inflammatory, anti-adhesive (resolving) and hormonal drugs.
Serosocele and IVF
Pregnancy and serozocele are not a very desirable combination from a medical point of view, requiring a particularly careful approach from a gynecologist. A large neoplasm can provoke compression of nearby organs, disruption of the blood supply to the reproductive system. A large cyst can cause severe pain, and compression of the enlarged uterus can lead to complications during pregnancy. It is optimal to remove serozocele before pregnancy occurs, so no specialist will dare to prepare a patient for IVF against the background of this pathology.
Only small serozoceles are not considered a contraindication to IVF. However, the decision in any case remains with the attending physician.
How to stop the growth of serocele?
In order to stop the growth of serozocele, it is possible to use enzyme agents based on hyaluronidase. This enzyme substance affects the "framework" of connective tissue fibers, which form the adhesions that form the neoplasm. It is pointless to introduce natural hyaluronidase into the body: it is quickly neutralized by blood plasma components and does not have time to perform its therapeutic task. Therefore, Longidaza is used for treatment - we are talking about a modern enzyme agent based on the action of the same hyaluronidase. However, unlike the absorbable drugs of previous generations, the composition of Longidaza is balanced by a high-molecular representative. This allows hyaluronidase to exhibit resistance to external enzyme influence and demonstrate its therapeutic effect. Longidaza optimizes the redistribution of moisture in the intercellular space, which, in turn, helps to eliminate edema, resolve hemorrhages, and also improves the percentage of antibiotics delivered directly to the infectious focus. In addition, the decrease in the density of the connective tissue base under the influence of Longidaza increases the elasticity of adhesions, which helps reduce pain.
The development of serozocele often goes unnoticed by the patient. At first, adhesions are formed, which act as a holding "skeleton" for the neoplasm. In this situation, it is important to both eliminate the existing adhesion process and prevent the appearance of new pathological elements. Longidaza will also help with this, which will reduce the swelling of inflamed tissues, make the formed adhesions more elastic and prevent the formation of new ones.
Longidaza is available in the form of suppositories and lyophilisate for the preparation of an injection solution. The doctor will be able to select the correct treatment regimen and will describe in detail the main points of treatment with the enzyme preparation.
Medicines that a doctor may prescribe
Treatment of serozocele currently involves the administration of anti-inflammatory and antibacterial drugs. However, even prolonged use of antibiotic therapy does not always provide sufficient concentration and delivery of medications to the site of chronic inflammation. Doctors have been using proteolytic enzymes for many years now - their ability to enhance the therapeutic effect of antibiotics, improve the degree of their penetration into tissues and increase the effectiveness of treatment has been proven by a number of tests and clinical trials.
One of the main factors in the formation of disorders of connective tissue is the inflammatory process. Of course, to get rid of serozocele, it is necessary to comprehensively influence both the formed fibrous process and the inflammatory reaction that activates its formation.
For serocele, the doctor may prescribe the following medications:
Aloe extract liquid |
A biogenic stimulant that is injected subcutaneously at 2 ml daily for ten days. Side effects are rare: allergic reactions, a feeling of blood flow to the pelvic area, increased menstrual bleeding are possible. |
Folic acid |
A drug that takes part in many important biochemical processes. It is taken 1 capsule (2 mg) three times a day for a month. The drug is usually well tolerated, only in rare cases nausea, itching, and insomnia may bother. |
Vitamin E |
A fat-soluble vitamin with a pronounced antioxidant and radioprotective property. Take 0.4 g twice a day. The duration of administration is determined by the doctor. Possible side effects: allergic reactions, dizziness, nausea, general weakness. |
Longidaza |
It is the "gold standard" of treatment of serozocele. Suppositories are prescribed rectally or vaginally, 1 pc. once a day at night, for 10-20 days. If necessary, the treatment is repeated after 3 months. When first used, it is necessary to take into account the possibility of individual hypersensitivity to the drug. The treatment regimen using the injection method of Longidaza is determined by the doctor individually. |
Trypsin |
A proteolytic agent that can be administered as intramuscular injections or electrophoresis. 0.01 g of the drug is administered intramuscularly 1-2 times a day, with sodium chloride or procaine. The treatment course usually includes 10-15 injections. Possible side effects: allergy, tachycardia, pain at the injection site. |
Vitamins
If the serozocele is already detected at a fairly large size, and there is an active adhesive process, then in addition to the main treatment, biogenic stimulants and resorption drugs are prescribed, such as aloe, FiBS, vitreous body, Lidase, Longidaza, Humizol.
In addition to all of the above, injections of vitamin B 12, or cyanocobalamin, are prescribed at 400-600 mcg per day for two weeks. In addition, thiamine chloride, or vitamin B 1, is indicated at 0.5-1 ml of a 2.5% solution for a month.
Cyanocobalamin helps eliminate pain syndrome and restore tissue metabolism. And thiamine chloride regulates metabolism and participates in the processes of conducting nervous excitation. These vitamins help to restore damaged tissues, accelerate recovery, and prevent the development of relapses of serozocele.
Physiotherapy treatment
Physiotherapeutic methods often become auxiliary in a complex of therapeutic measures consisting of drug and surgical treatment. Physiotherapy helps:
- reduce the duration of therapy;
- prevent the development of complications and relapses;
- prevent the development of side effects from drug therapy;
- reduce the drug load on the body.
For serocele, the following procedures are most often prescribed:
- Electro and magnetic therapy are often used in the early postoperative period and have anti-inflammatory and anti-edematous effects.
- Ultrasound therapy – provides an analgesic effect, helps soften adhesions, optimizes blood circulation.
- Phototherapy – causes a powerful bactericidal effect, helps stop the inflammatory process.
- Manual therapy, massage – affects skin receptors, the vascular network of internal organs, significantly improves blood and lymph circulation in the pelvic area and the entire abdominal cavity.
Treatment for serozocele requires a thorough and individual approach. Physiotherapy can become that very necessary link in the chain of treatment measures that contribute to improving the general health and, in particular, the reproductive function of patients.
Folk remedies
Sometimes patients try to use folk methods for treatment. However, medical specialists are skeptical about this type of therapy and consider it ineffective, allowing only a combination of alternative treatment and the doctor's prescriptions. For example, in case of serozocele, the use of a decoction of the rhizome of bergenia is popular. To prepare it, take 15 g of crushed raw materials, pour 200 ml of boiling water, keep for about half an hour in a water bath, filter and squeeze, add water to 200 ml. Drink the remedy on an empty stomach, 2 tbsp. three times a day, or use for douching.
Another common recipe is to use an infusion of peony root three times a day before meals, ¼ cup (about 50 ml) for a month. To prepare the infusion, pour 1 teaspoon of raw material with 400 ml of boiling water, leave overnight under the lid. In the morning, filter and take. Store in the refrigerator.
Another recipe involves the use of the herb Morinda citrifolia. The juice or powder (crushed raw material) of the plant is usually used for treatment.
To get rid of serocele, some patients resort to hirudotherapy: procedures with the use of medical leeches are repeated in courses 2-3 times a year.
Herbal treatment
Treatment with medicinal herbs is usually available and sometimes effective. However, such an unconventional approach to solving the problem should be discussed with your doctor in advance. You can use various medicinal plants for serozocele, following these recipes:
- Squeeze the juice from fresh burdock leaves. Take 2 tbsp. three times a day, about half an hour before the main meal. Duration of treatment is 1 month.
- Take 4 tbsp. dried acacia flowers, pour 0.5 l of vodka, place in a dark place for 7 days. After a week, filter the tincture, take 1 tbsp. three times a day before meals.
- Pour 1 tbsp. of clover with 1500 ml of boiling water, leave for 7-8 hours. Filter and drink the entire volume during the day. Repeat the procedure daily for 8 weeks.
- Take 5 tbsp. of fresh spruce needles, pour 1 liter of boiling water, leave in a thermos for 24 hours. Take 3 tbsp. of this remedy in the morning before breakfast, 100 ml before lunch, and 50 ml before dinner. The regimen is as follows: take for 3 days, then take a break for 2 days. The total duration of treatment is 5 weeks.
Homeopathy
Alternative treatments, such as homeopathy, cannot replace surgical intervention. However, in mild cases, doctors allow the use of homeopathic drugs, which act gently and do not have negative side effects.
The selection of a suitable remedy is made only with the use of an individual approach, detailed collection of anamnesis. Each case for a homeopath is not only a special course of the disease, but also individual characteristics of the patient. Only taking into account all the nuances can one hope for the healing of a person with serozocele.
In case of serozocele, the following preparations are recommended: Angustura vera, Bellis perennis, Calcarea fluorica, Cuprum metallicum, Nux vomica, Ignatia amara. Arnica montana, Hypericum perforatum, Aconitum napellus, Calcarea carbonica, Phosphorus have a good effect.
The main purposes may be:
- Silicea 6 – for 3 weeks, C12 or C30;
- Apis mellifika 6;
- Silicea 30 in combination with Apis mellifica 6.
Surgical treatment
Quite often, getting rid of serocele becomes impossible without radical surgical treatment. Usually, adhesions are dissected using a laparoscopic or laparotomic method. Unlike puncture, the risk of recurrence of serocele after surgery is only about 30%. In the postoperative period, the patient is prescribed rehabilitation treatment, using absorbable drugs, physiotherapy, and exercise therapy.
The adhesions holding the serozocele are dissected with a scalpel, laser beam, "electric knife" or by means of aquadissection. After the procedure, it is possible to apply absorbable polymeric materials to the tissues to prevent recurrence of the adhesion process.
Laparoscopy has a number of advantages over laparotomy:
- less postoperative discomfort;
- fast rehabilitation period, early patient discharge;
- the best cosmetic result (almost complete absence of postoperative scars).
- However, laparoscopy also has some disadvantages, such as:
- some technical difficulties, need for special equipment;
- the need for appropriate training of specialists.
In normal cases, doctors prefer to choose laparoscopy. If the serozocele has significant dimensions and is accompanied by extensive adhesions, then the choice may end in favor of laparotomy.
Recovery after surgery can last from 2 months to six months, depending on the scale of the operation. Throughout the rehabilitation period, the patient undergoes regular ultrasound checks. During rehabilitation, it is recommended to refrain from physical activity and thermal procedures, eat a full and high-quality diet, monitor normal bowel movements, and control your own weight. [ 8 ]
The operation to remove a serocele usually ends positively: the cyst disappears along with all the previously disturbing symptoms. Possible complications of surgical treatment may include:
- infectious processes;
- postoperative hernias;
- damage to the intestines, bladder;
- intestinal obstruction.
Complications after laparoscopy occur quite rarely, but with laparotomy they occur more often – approximately 4 times more often.
Serosocele puncture
The minimal surgical operation for serozocele is considered to be a puncture biopsy. The procedure is performed as follows. Under ultrasound observation (monitoring), the surgeon inserts a special needle into the cystic cavity and sucks out the fluid present in it. Directly during this procedure, the pressure exerted by the neoplasm on the surrounding tissues and organs decreases, and the pain disappears. If the fluid accumulates again, the puncture is repeated.
The extracted fluid undergoes laboratory analysis. Using enzyme immunoassay and bacterial cultures, the microbial flora is identified and its sensitivity to antibiotic therapy is determined. During the study, it is possible to determine the affiliation of bacteria, viruses, fungal infections, identify chronic genitourinary infections and antibodies to the tuberculosis pathogen. The diagnostic results directly affect the doctor's prescription scheme. [ 9 ]
Prevention
To date, there have been no cases of transformation of serozocele into a malignant process. However, this disease can cause a number of complications. Therefore, it is important to follow the doctors' preventive instructions to prevent both the occurrence and recurrence of serozocele. Experts recommend:
- undergo a preventive examination by a gynecologist every year;
- prevent and promptly treat endometriosis and inflammatory processes in the pelvis;
- to prevent unwanted pregnancy, use effective contraceptives;
- During pregnancy, strive for natural vaginal birth.
Serosocele is classified as a peritoneal cyst with complex diagnosis. This is due, in particular, to the difficult clinical differentiation of the disease. And this is another argument why it is necessary to pay sufficient attention to the prevention of pathology.
Forecast
The prognosis for detecting a serozocele depends on several factors at once - for example, the size of the pathology, its location, the age and general health of the patient. An unfavorable development of events can be discussed in the absence of therapy and observation by a doctor.
In order to improve the prognosis, it is recommended to lead a moderately active lifestyle, avoid overloading and carrying heavy objects, and refuse strength training. However, a complete lack of physical activity is also not welcomed.
It is equally important to monitor your diet and avoid gaining excess weight.
Any infectious and inflammatory diseases should be treated as soon as possible. It is necessary to prevent infection with STIs, refrain from unprotected sexual intercourse. In case of serozocele, it is necessary to regularly visit a doctor for control diagnostics.

