Medical expert of the article
New publications
Schizophrenia
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Schizophrenia is a serious and chronic mental disorder that affects a person's thinking, feelings, and behavior. People with schizophrenia may experience a variety of symptoms, including auditory hallucinations ( auditory hallucinations ), delirium (disjointed or meaningless thinking), confusion about time and place, and cognitive impairment. The disorder usually begins in early adulthood, often in adolescence or young adulthood.
The main characteristics of schizophrenia include:
- Positive symptoms: These symptoms include auditory and visual hallucinations, delirium (confused thoughts and speech), delusions (beliefs that are not based on reality), and thought disturbances.
- Negative symptoms: Negative symptoms include apathy, social withdrawal, anedonia (inability to experience pleasure), apraxia (impaired ability to perform daily tasks), and poverty of speech.
- Disorganization: Disorganization involves impairments in the ability to maintain a logical sequence of thoughts and normal social and occupational function.
- Cognitive symptoms: These are disturbances in cognitive functions such as memory, attention and planning.
The causes of schizophrenia are not yet fully understood or researched, but it is believed that they may include genetic factors, neurochemical imbalances in the brain, and environmental factors such as stress, drugs, and early childhood exposure.
Treatment of schizophrenia involves a combination of medication (psychopharmacotherapy) and psychosocial interventions (psychotherapy, rehabilitation and support). The goal of treatment is to reduce symptoms, improve quality of life and manage the disease. Early detection and treatment can help reduce the effects of schizophrenia and improve the prognosis.
Epidemiology
The global age-standardized prevalence of schizophrenia in 2016 was estimated to be 0.28% (95% UI: 0.24–0.31), showing the onset of schizophrenia in adolescence and young adulthood, with prevalence peaking at around 40 years of age and declining in older age groups. No sex differences in prevalence were observed.[ 4 ]
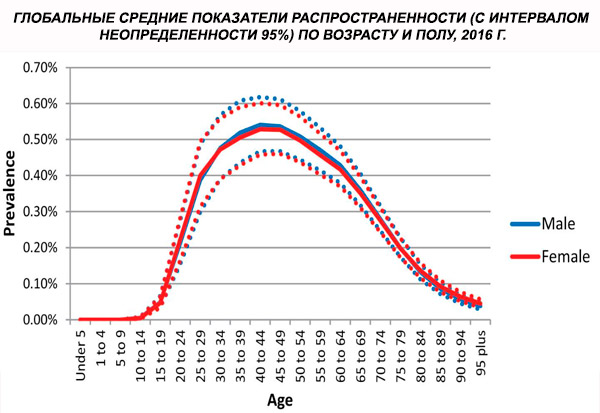
Worldwide, the prevalence of cases increased from 13.1 (95% CI: 11.6–14.8) million in 1990 to 20.9 (95% CI: 18.5–23.4) million cases in 2016. Age group 25–54 years.

Worldwide, the prevalence of schizophrenia is about 1%. Rates are similar among men and women and are relatively constant across cultures. Prevalence is higher among lower socioeconomic classes in cities, possibly because of the disabling effects of unemployment and poverty. Similarly, the higher prevalence among lonely people may reflect the effect of the illness or precursors of the illness on social functioning. The average age of onset is about 18 years in men and 25 years in women. Schizophrenia rarely begins in childhood, but may occur in early adolescence and late adulthood (sometimes called paraphrenia).
 [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ]
[ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ]
Risk factors
The advent of psychotropic drugs and modern highly sensitive neurochemical methods made it possible to establish a connection between the function of the central nervous system and mental disorders. Research into the mechanisms of action of psychotropic drugs has allowed a number of hypotheses to be put forward about the role of certain neurotransmitters in the pathogenesis of psychosis and schizophrenia. The hypotheses suggested the involvement of dopamine, norepinephrine, serotonin, acetylcholine, glutamate, several peptide neuromodulators and/or their receptors in the pathogenesis of these disorders. The dopamine hypothesis of schizophrenia has remained dominant for more than a quarter of a century.
 [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ]
[ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ]
Dopamine
Psychostimulants, including cocaine, amphetamine, and methylphenidate, activate the dopaminergic system of the brain. Their abuse can cause paranoid psychosis, reminiscent of the positive symptoms of schizophrenia. In patients with schizophrenia, psychostimulants can provoke an exacerbation of psychosis. Conversely, there is strong evidence that the action of typical neuroleptics is associated with the blockade of dopamine receptors. First, most typical neuroleptics can cause extrapyramidal side effects, which can develop with the death of dopaminergic neurons (as, for example, in Parkinson's disease). Second, receptor binding studies have revealed a relationship between the clinical efficacy of typical neuroleptics and their affinity for dopamine D2 receptors. Moreover, it turned out that the antipsychotic activity of neuroleptics does not depend on their interaction with other receptors: muscarinic, alpha-adrenergic, histamine or serotonin. All this gives grounds to assume that the symptoms of schizophrenia are caused by excessive stimulation of dopamine receptors, presumably in the cortico-limbic areas of the brain. [ 21 ]
However, the weak point of the dopamine hypothesis of schizophrenia is that the effect on dopamine receptors affects mainly positive symptoms and has little effect on negative symptoms and cognitive disorders. In addition, it was not possible to establish a primary defect in dopaminergic transmission in schizophrenia, since researchers obtained different results when functionally assessing the dopaminergic system. The results of determining the level of dopamine and its metabolites in the blood, urine and cerebrospinal fluid were inconclusive due to the large volume of these biological environments, which leveled out possible changes associated with limited dysfunction of the dopaminergic system in schizophrenia.
The increase in the number of dopamine receptors in the caudate nucleus in schizophrenia can also be considered as a confirmation of the dopamine hypothesis, but the interpretation of these changes is difficult, and they may be not so much a cause as a consequence of the disease. [ 22 ] A more informative approach to assessing the state of the dopaminergic system is based on the use of ligands that selectively interact with D2 receptors and allow us to determine their binding capacity. By comparing the number of occupied receptors before and after drug administration, it is possible to estimate the ratio of dopamine release and reuptake. Two recent studies using positron emission tomography (PET), based on this technique, provided the first direct evidence for the truth of the hyperdopaminergic theory of schizophrenia. [ 23 ], [ 24 ]
Measuring dopamine and its metabolites in brain tissue at postmortem examination may also be important. However, because cells disintegrate after death, true tissue dopamine concentrations are often difficult to determine. Furthermore, administration of antipsychotic drugs may also affect the results of postmortem biochemical studies. Despite these methodological limitations, postmortem studies have revealed neurochemical differences in the brains of patients with schizophrenia and controls. For example, postmortem examination of the brains of patients with schizophrenia has revealed elevated dopamine concentrations in the left amygdala (part of the limbic system). This finding has been confirmed in several studies and is unlikely to be an artifact (since the changes are lateralized). Increased postsynaptic dopamine receptors have also been reported in the brains of patients with schizophrenia who have not received antipsychotic therapy. These data confirm that the increased receptor numbers are not a consequence of drug therapy. In addition, there is evidence of an increase in the number of dopamine D4 receptors in certain areas of the brain, regardless of whether the patient was taking neuroleptics or not.
However, the dopamine hypothesis is unable to explain the development of abulic and anhedonic manifestations of schizophrenia. As already mentioned, the complex of negative symptoms seems to be relatively independent of positive symptoms. It is interesting that dopamine receptor agonists can positively influence negative symptoms, while receptor antagonists promote their development in humans and model them in laboratory animals. Thus, although elevated dopamine levels in the anterior cingulate cortex and other limbic structures may partly cause positive psychotic symptoms, negative symptoms may be a consequence of decreased activity of the dopaminergic system in the prefrontal cortex. Perhaps this is why it is difficult to create an antipsychotic drug that would simultaneously correct dopaminergic hyperfunction in some areas of the brain and their hypofunction in others.
 [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ]
[ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ]
Glutamatergic hypothesis of schizophrenia development
Glutamate is the major excitatory neurotransmitter in the brain. Interest in its possible role in the pathogenesis of schizophrenia has arisen from data on the N-MemuA-D-acuapmame (NMDA) receptor complex, the major subtype of glutamate receptors. Recent studies of the interactions between the glutamatergic, dopaminergic, and GABAergic systems of the brain have shown that phencyclidine, when administered acutely and chronically, is a psychotomimetic that noncompetitively blocks the NMDA receptor ion channel. Acute administration of phencyclidine produces effects similar to the positive, negative, and cognitive symptoms of schizophrenia. In addition, reports of long-term exacerbation of psychosis in patients with schizophrenia confirm the psychotomimetic properties of phencyclidine. Long-term administration of phencyclidine induces a state of dopaminergic deficit in the prefrontal cortex, which may be responsible for the development of negative symptoms. In addition, both phencyclidine and its analogue ketamine weaken glutamatergic transmission. Observations of schizophrenia-like symptoms in phencyclidine abusers are confirmed by studies on healthy volunteers, in whom ketamine induced transient, mild positive, negative and cognitive symptoms characteristic of schizophrenia. Like phencyclidine, ketamine induced distortion of perception. Thus, glutamatergic deficiency causes the same symptoms as in the hyperdopaminergic state, which resemble the manifestations of schizophrenia. Glutamatergic neurons are able to suppress the activity of dopaminergic neurons via NMDA receptors (directly or via GABAergic neurons), which may explain the connection between the glutamatergic system and the dopamine theory of schizophrenia. These data support the hypothesis linking schizophrenia with insufficiency of glutamatergic systems. Accordingly, compounds that activate the NMDA receptor complex may be effective in schizophrenia. [ 32 ], [ 33 ]
The difficulty in developing drugs that stimulate the glutamatergic system is that excessive glutamatergic activity has a neurotoxic effect. However, activation of the NMDA receptor complex via its glycine site by glycine itself or D-cycloserine has been reported to alleviate negative symptoms in patients with schizophrenia, which is an excellent example of a possible practical application of the glutamatergic hypothesis.
The glutamatergic hypothesis represents a major breakthrough in the study of biochemical disturbances in schizophrenia. Until recently, neurochemical studies of schizophrenia were limited to studying the mechanisms of action of neuroleptics, which were developed empirically. With the growth of knowledge about the neuronal organization of the brain and the properties of neurotransmitters, it became possible to first develop a pathophysiological theory and then create new drugs on its basis. The various hypotheses of the origin of schizophrenia that exist today allow us to hope that in the future the development of new drugs will proceed more rapidly.
Other neurotransmitter and neuromodulatory hypotheses for the development of schizophrenia
The rich serotonergic innervation of the frontal cortex and limbic system, the ability of the serotonergic systems of the brain to modulate the activity of dopaminergic neurons and participate in the regulation of a wide range of complex functions have led a number of researchers to conclude that serotonin plays an important role in the pathogenesis of schizophrenia. Of particular interest is the hypothesis that excess serotonin can cause both positive and negative symptoms. [ 34 ] This theory is consistent with the ability of clozapine and other new-generation neuroleptics that block serotonin receptors to suppress positive symptoms in chronically ill patients resistant to typical neuroleptics. However, a number of studies have questioned the ability of serotonin receptor antagonists to reduce negative symptoms associated with psychosis, depression, or side effects of pharmacotherapy. These drugs have not been officially approved as a treatment for the primary negative symptoms that form the underlying defect in schizophrenia. However, the idea that serotonin receptor antagonists (especially 5-HT2a) may be effective has played a major role in the development of new-generation neuroleptics. The advantage of combined D2/5-HT2 receptor antagonists is more likely to be a lower incidence of extrapyramidal side effects than a higher antipsychotic activity. However, since this improves compliance (patients' willingness to cooperate), the treatment is more effective.
There are also hypotheses about the importance of dysfunction of the noradrenergic systems in schizophrenia. It is assumed that anhedonia is one of the most characteristic manifestations of schizophrenia, which consists of the inability to receive satisfaction and experience pleasure, and other deficit symptoms may be associated with dysfunction of the noradrenergic reinforcement system. However, the results of biochemical and pharmacological studies testing this hypothesis have proven contradictory. As in the case of the dopamine and serotonin hypotheses, it is assumed that in schizophrenia, both a decrease and an increase in the activity of the noradrenergic systems may occur.
General hypotheses of the development of schizophrenia
Future research into schizophrenia will likely be guided by complex models based on a synthesis of neuroanatomical and neurochemical hypotheses. An example of such an approach is a theory that takes into account the role of neurotransmitter systems in disrupting connections between the cortex, basal ganglia, and thalamus, which form the subcortical-thalamocortical neural circuits. The cerebral cortex, through glutamatergic projections to the basal ganglia, facilitates the implementation of selected actions while suppressing others. [ 35 ] Glutamatergic neurons stimulate intercalated GABAergic and cholinergic neurons, which in turn suppress the activity of dopaminergic and other neurons. The study of the neuroanatomical and neurochemical mechanisms of the cortical-subcortical circuits considered in this model served as a starting point for the creation of new hypotheses on the pathogenesis of schizophrenia. These models facilitate the search for neurotransmitter targets for new drugs and also explain some of the features of the action of existing drugs, such as phencyclidine, in schizophrenia.
A modern neuroanatomical model was proposed by Kinan and Lieberman (1996) to explain the distinctive action of atypical antipsychotics (such as clozapine ) compared with conventional agents (eg, haloperidol ). According to this model, the distinctive action of clozapine is explained by the fact that it has a very specific action on the limbic system without affecting the activity of striatal neurons, whereas typical antipsychotics have a significant effect on striatal function. Other antipsychotics with similar properties (eg, olanzapine ) may also have an advantage over conventional agents. Newer antipsychotics (eg, risperidone and sertindole ) are not as limbic-limited as clozapine, but they compare favorably with typical antipsychotics in that they are less likely to cause neurological impairment at therapeutic doses. Research into the validity of this and other hypotheses will continue as new agents with pharmacological and clinically similar actions become available.
Pathogenesis
Patients with schizophrenia are prescribed certain groups of drugs, but the choice of drug is often determined not so much by the diagnosis as by the patient's symptoms and the nature of their combination.
Although perceptual distortion and behavioral disorganization are different symptoms, they respond to the same drugs, dopamine D2 receptor antagonists. [ 36 ], [ 37 ] This justifies considering these two symptom complexes together when discussing antipsychotic therapy.
The mechanisms of development of negative symptoms in schizophrenia are associated with decreased activity of the dopaminergic system in the prefrontal cortex, and not with its hyperfunction in the limbic structures, which is supposed to underlie psychosis. In this regard, concerns arise that drugs that suppress psychosis may aggravate negative symptoms. [ 38 ], [ 39 ], [ 40 ] At the same time, dopamine receptor agonists can weaken negative symptoms, but provoke positive symptoms. Negative symptoms are among the key manifestations of schizophrenia and are characterized by persistent disorders of the emotional-volitional sphere. Until now, there are no drugs that would demonstrably reduce these most important manifestations of the disease. However, clinical trials of atypical antipsychotics have shown that they are able to reduce the severity of negative symptoms, assessed using rating scales. The SANS, BPRS, and PANSS scales contain items assessing activity at school or work, limitation of social contacts, and emotional detachment. These symptoms can be considered as general manifestations of the disease, decreasing with the weakening of psychosis, but can also be associated with the side effects of neuroleptics (for example, bradykinesia and sedative effect) or depression (for example, anhedonia). Thus, a patient with pronounced paranoid delusions against the background of neuroleptic therapy can become more sociable and less wary, and his emotional reactions can become more lively as the paranoid symptoms regress. But all this should be considered as a weakening of secondary negative symptoms, and not as a result of a decrease in primary affective-volitional disorders.
Many neuropsychological tests that assess attention and information processing and involve neuroanatomical interpretation reveal changes in patients with schizophrenia. Cognitive impairments in patients with schizophrenia are not directly related to the main symptoms of the disease and usually remain stable even with significant regression of psychotic symptoms. [ 41 ], [ 42 ] Cognitive impairments, along with primary negative symptoms, are apparently one of the important causes of persistent maladjustment and decreased quality of life. The lack of effect of typical neuroleptics on these central manifestations of the disease may explain such a high level of disability in patients, despite the ability of neuroleptics to effectively suppress psychotic symptoms and prevent their relapses.
 [ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ], [ 48 ], [ 49 ], [ 50 ], [ 51 ], [ 52 ]
[ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ], [ 48 ], [ 49 ], [ 50 ], [ 51 ], [ 52 ]
Symptoms schizophrenias
The concept of schizophrenia as a single disease emerged in the early 20th century, when Emil Kraepelin suggested that paranoia, hebephrenia, and catatonia were not separate diseases but manifestations of dementia praecox. He also made a clear distinction between this form of mental illness and manic-depressive psychosis. This became possible after a significant number of cases of mental illness were linked to syphilis, which made it possible to distinguish them from the rest of the group of patients with mental disorders. The discovery of the etiology, treatment, and prevention of neurosyphilis was one of the major victories of medical science and gave hope that the causes of the main mental disorders would be found.
Eugen Bleuler (1950) proposed the new term "schizophrenia" instead of the previously used "dementia praecox", arguing that the fundamental psychopathological phenomenon characteristic of this disease was dissociation ("splitting") - both "within" the thought process and between thoughts and emotions. The term "schizophrenia" was an expression of this concept and, in turn, had a significant impact on its further development. Classical forms of schizophrenia (e.g., hebephrenic, paranoid, catatonic, simple), to which schizoaffective and latent were later added, are still commonly diagnosed in clinical practice for descriptive purposes, although recently there has been a tendency to transform psychiatric terminology under the influence of the official American nomenclature DSM-III and DSM-IV. However, the identification of individual forms of schizophrenia has proven to be unproductive in terms of developing differentiated therapy or studying etiology and pathogenesis.
ICD-10 lists the following symptoms of schizophrenia: delusions (bizarre, grandiose, or persecutory), disordered thinking (intermittent or illogical flow of thoughts or incomprehensible speech), perceptual disturbances (hallucinations, feelings of passivity, ideas of reference), mood disturbances, movement disturbances (catatonia, agitation, stupor), personality decline, and decreased functioning.
During life, schizophrenia develops in 0.28% (95% UI: 0.24–0.31). In childhood, symptoms of schizophrenia are manifested by a weakening of motivation and emotional reactions. Subsequently, the sense of reality is impaired, and perception and thinking deviate significantly from the norms existing in a given culture, which is usually manifested by delusions and auditory hallucinations. Visual and somatic hallucinations, disorganization of thinking and behavior are also common.
Psychosis associated with a disturbance of the sense of reality usually manifests itself in men aged 17-30 years, and in women - 20-40 years. The course and outcome of psychotic disorders are highly variable. In some patients (about 15-25%), the first psychotic episode ends in complete remission, and in the following 5 years there are no psychotic disorders (however, during subsequent observation, the proportion of these patients decreases). In other patients (approximately 5-10%), pronounced psychotic disorders persist without remission for many years. In the majority of patients, after the first psychotic episode, partial remission occurs, and subsequently exacerbations of psychotic symptoms are periodically observed.
In general, while the severity of psychotic disorders reaches a plateau 5-10 years after the first episode, emotional-volitional impoverishment continues for a longer period. [ 53 ] The progression of schizophrenia symptoms is often a consequence of the increase in primary disorders associated with schizophrenia. These include autism, loss of working capacity, learning disabilities, and low self-esteem and that of others. As a result, patients are left alone, unable to find work, and subject to stress, which can provoke an exacerbation of symptoms and an increase in their functional impairment. In addition, the diagnosis of schizophrenia itself continues to generate a negative reaction among others, which further limits the patient's capabilities. Although with age there is a tendency for schizophrenia symptoms to weaken and functional status to often improve, it cannot compensate for the years of life lost to the patient and the opportunities missed.
The relationship between criminal activity and schizophrenia
Wessely et al., in their study of the Camberwell Register, sought to answer the question: "Is schizophrenia associated with an increased risk and frequency of offending?" They concluded that people with schizophrenia, although not generally considered to be at increased risk of criminal behaviour, do have a higher risk than other mental disorders of conviction for violent offences. There was an increased risk of violence and therefore conviction for violence among people with psychosis, but this association was less clear in the absence of co-morbid substance misuse. In an Office for National Statistics review of psychiatric morbidity in prisoners, the prevalence of functional psychosis in the year studied was 7% among convicted men, 10% among unconvicted remand men and 14% among female prisoners, compared with a comparable figure of 0.4% in the general population. The results of this review may require a reconsideration of the above results, as it is highly unlikely that the differences in rates of mental disorder between prison and general populations of this size could be explained by the courts' bias towards sentencing mentally ill people. Of course, these results in no way indicate a causal relationship between crime and psychosis, only an association.
The association of schizophrenia with violent crime has generally received more attention than the association of schizophrenia with other crimes. [ 54 ], [ 55 ] Taylor's review of the research on the topic concludes that in people with schizophrenia and convictions for violent crimes, the violent acts overwhelmingly occur after the onset of the illness. A study of first-episode schizophrenia shows that among first-episode patients, more than a third had engaged in violent behaviour in the month before admission, including potentially life-threatening behaviour and bizarre sexual behaviour. Many of these patients had had police contact prior to their first admissions, but few were charged after admission. Taylor investigated the possibility of schizophrenia in a consecutive sample of remand prisoners in Brixton Prison. The prevalence of convictions for violent crimes among individuals with schizophrenia was approximately 12% to 13%. Approximately 5% to 8% of controls were convicted of violent crimes. According to a report from the National Confidential Inquiry into Homicide by People with Mental Illness, 5% of those convicted of homicide had symptoms of psychosis. Contrary to popular beliefs about people with psychosis, the victim is most often a family member rather than a stranger (a more general finding for violent behavior in a community sample in the Steadman et al. study).
Some specific symptoms of schizophrenia are associated with violence. Thus, Virkkunen, studying a group of schizophrenic patients in Finland who were guilty of severe episodes of violence and a group of arsonists, found that 1/3 of them committed crimes directly as a result of hallucinations or delusions; the remaining 2/3 committed crimes due to problems caused by stress in the family. Symptoms of threat/loss of control over the situation are directly associated with violence. With symptoms that destroy the feeling of personal autonomy and the ability to influence the situation, patients may consider their actions to counteract threats related to them to be justified ("rationality within irrationality").
Delusional psychotic patients who commit violent acts as a result of their ideas differ from non-violent patients in their preoccupation with evidence to support their ideas, their conviction that such evidence has been found, and their affective changes, particularly depression, anger, or fear, associated with their delusional preoccupation. In the Brixton studies by Taylor et al., delusions of passivity, religious delusions, and delusions of influence were significantly more associated with violent acts.
The risk associated with active symptoms of schizophrenia, including threat/loss of control symptoms, is greatly increased by substance abuse. The role of the latter factor is highlighted by the study by Steadman et al.: when this factor was controlled for, the rate of violence among recently discharged psychiatric patients was no higher than the rate of violence in the general population. Hallucinations as part of the illness are most often associated with violence if they are command hallucinations, or if falsely perceived tastes and smells are interpreted as “evidence” for delusions of control. Less well understood is the role of abnormal personality development in the commission of crimes by individuals with schizophrenia (whether it is a comorbid condition or a consequence of the illness).
 [ 56 ], [ 57 ], [ 58 ], [ 59 ]
[ 56 ], [ 57 ], [ 58 ], [ 59 ]
Theories of Schizophrenia Symptoms
The original concept of schizophrenia as an early-onset and steadily progressing neurodegenerative disease (dementia praecox) is currently rejected. Modern hypotheses consider schizophrenia as a neurodevelopmental disease associated with impaired development of the nervous system and progressing only in the first years, but not throughout life, which is more consistent with clinical observations. [ 60 ], [ 61 ] The dysontogenetic theory of schizophrenia allows us to understand the role of established etiological factors. Risk factors for schizophrenia, such as birth in winter, positive family history, complicated pregnancy and childbirth, can disrupt brain development, early forming a predisposition to the disease. Observations of children with a hereditary predisposition, for example, those born to mothers suffering from schizophrenia, have revealed a link between the presence of motor, cognitive and affective disorders and the subsequent development of psychosis. There is debate as to whether psychosis is the result of the disease progressing in childhood and adolescence or whether it occurs when a predisposition that arose in early years but remained stable manifests itself during adolescence, under conditions of increased psychological stress. These theories are not mutually exclusive, as both suggest the early appearance of mild symptoms and the subsequent development of full-blown psychosis. It should be noted that after the disease has reached the psychotic level, neither neuroimaging methods, nor neuropsychological research, nor clinical observation, nor, finally, pathomorphological data indicate further progression of the disease.
Most patients with schizophrenia continue to have negative symptoms throughout their lives, and increasing social maladjustment may be a consequence of the relationship between the patient and society. [ 62 ] This can be explained at a very basic level, for example, by considering the problem of employment. After a psychotic episode, it is difficult for the patient to return to his previous life and previous occupation. Even in the absence of any symptoms, employers, co-workers, friends and relatives do not consider him to be a capable person. The unemployment rate among patients with schizophrenia reaches 80%, although a significant proportion of them retain their ability to work. The significance of this factor is well demonstrated in studies of sociocentric cultures in developing countries, where patients with schizophrenia can maintain their social and professional status in a significantly less stressful environment. In these countries, the disease has a more benign course. A detailed discussion of the etiology and neurobiological foundations of schizophrenia is provided by Carpenter and Вuchanan, Waddington.
It has long been noted that patients with schizophrenia are very heterogeneous in relation to the nature of the onset of the disease, the leading symptoms, the course, the effectiveness of treatment, and the outcome. In 1974, an alternative hypothesis was proposed (Strauss et al., 1974), based on data from cross-sectional and prolonged clinical observations, which indicate a relative independence between positive psychotic symptoms, negative symptoms, and a violation of interpersonal relationships. The essence of the hypothesis is that these groups of symptoms have an independent psychopathological basis, and do not represent manifestations of a single pathophysiological process. [ 63 ] During the observation period, a high correlation was noted between the severity of psychopathological symptoms related to one group, and, conversely, no correlation was observed between the severity of symptoms related to different groups. These data were confirmed in numerous studies, but with one addition. It turned out that hallucinations and delusions are closely related to each other, but do not correlate with other positive symptoms (for example, disorganization of thinking and behavior). Currently, it is generally accepted that the key manifestations of schizophrenia include a distortion of the sense of reality, disorganization of thinking and behavior, negative symptoms and cognitive impairment. Negative symptoms of schizophrenia include weakening of emotional reactions and their external manifestations, poverty of speech, and decreased social motivation. Earlier, Kraepelin described these manifestations as "drying up of the source of will." Differences between groups of symptoms are extremely important when prescribing pharmacotherapy. Other clinical manifestations that are important from a therapeutic point of view include depression, anxiety, aggression and hostility, suicidal behavior.
For many years, the effect of drugs in schizophrenia was assessed mainly by their effect on psychotic symptoms or related parameters, such as the duration of hospitalization or remission. With the recognition of the relative independence of different symptom groups, a comprehensive assessment of the effect of therapy on each of these groups has become standard. It turned out that standard antipsychotic therapy has virtually no effect on cognitive impairment and negative symptoms of schizophrenia. [ 64 ] Meanwhile, these two symptom groups can have a decisive influence on the severity of the patient's condition and his or her quality of life. Awareness of the limitations of traditional pharmacotherapy has become an impetus for the development of new agents for the treatment of these manifestations of schizophrenia.
Schizophrenia is a chronic illness that may progress over several exacerbations, although the duration and characteristics of exacerbations may vary. Patients with schizophrenia tend to develop psychotic symptoms 12 to 24 months before seeking treatment. The premorbid period may include normal or impaired social competence, mild cognitive disorganization or perceptual distortions, decreased ability to experience pleasure (anhedonia), and other generalized difficulties in coping. Such symptoms of schizophrenia may be subtle and recognized only in retrospect, or may be more prominent with impairment of social, academic, and occupational functioning. Subclinical symptoms may be present in the prodromal period, including withdrawal or isolation, irritability, suspiciousness, unusual thoughts, perceptual distortions, and disorganization. The onset of the disease (delusions and hallucinations) may be sudden (over days or weeks) or slow and gradual (over years). The course of schizophrenia may be episodic (with obvious exacerbations and remissions) or continuous; there is a tendency for the functional deficit to worsen. In the late phase of the disease, the patterns of the disease may be stable, the degree of disability may stabilize and even decrease.
In general, the symptoms of schizophrenia as such can be divided into positive, negative, cognitive, and disorganizational symptoms. Positive symptoms are characterized by excess or distortion of normal functions; negative symptoms are characterized by a decrease or loss of normal functions. Disorganizational symptoms include disturbances in thinking and inappropriate behavior. Cognitive symptoms are disturbances in information processing and difficulty in problem solving. The clinical picture may include symptoms from one or all of these categories.
The positive symptoms of schizophrenia can be divided into delusions and hallucinations, or disturbances of thought and inappropriate behavior. Delusions are false beliefs. In delusions of persecution, the patient believes that he is being pestered, followed, or deceived. In delusions of reference, the patient believes that passages from books, newspapers, song lyrics, or other external cues are relevant to him. In delusions of thought insertion or thought withdrawal, the patient believes that other people can read his mind, that his thoughts are transmitted by others, or that thoughts and impulses are implanted in him by external forces. Hallucinations may be auditory, visual, olfactory, gustatory, or tactile, but auditory hallucinations are by far the most common. The patient may hear voices commenting on his behavior, talking to each other, or making critical and insulting remarks. Delusions and hallucinations can be extremely distressing to the patient. [ 65 ]
Thought disorders include disorganized thinking with incoherent, purposeless speech, with constant shifts from one topic to another. Speech disturbances may range from mild disorganization to incoherence and meaninglessness. Inappropriate behavior may include childlike stupidity, agitation, and inappropriate appearance and mannerisms. Catatonia is an extreme form of behavioral disturbances that may include maintaining a rigid posture and persistent resistance to movement or purposeless spontaneous motor activity.
Negative (deficit) manifestations of the disease are expressed in the form and include flattened affect, poverty of speech, anhedonia, and unsociability. With flattened affect, the patient's face appears hypomimetic, with poor eye contact and insufficient expressiveness. Poverty of speech is manifested by a decrease in speech production, monosyllabic answers to questions, creating the impression of internal emptiness. Anhedonia may reflect insufficient interest in activity and an increase in aimless activity. Unsociability is manifested by insufficient interest in relationships with people. Negative symptoms often lead to poor motivation and a decrease in the purposefulness of behavior.
Cognitive deficits include problems with attention, language processing, working memory, abstract thinking, problem solving, and understanding social interactions. The patient's thinking may become rigid, and the ability to solve problems, understand other people's points of view, and learn from experience is reduced. Symptoms of schizophrenia typically impair the ability to function and significantly interfere with work, social relationships, and self-care. Unemployment, isolation, disrupted relationships, and decreased quality of life are common. The severity of cognitive impairment largely determines the degree of overall disability.
Suicides
Research suggests that at least 5–13% of patients with schizophrenia die by suicide. [ 66 ] Suicide is the leading cause of premature death among people with schizophrenia, which may partly explain why life expectancy is reduced by an average of 10 years among people with schizophrenia. Patients with paranoid schizophrenia, late onset, and adequate pre-illness functioning, who have the best prognosis for recovery, are also more likely to commit suicide. Because these patients retain the capacity for grief and distress, they may be more likely to act in despair based on a realistic understanding of the consequences of their illness.
Violence
Schizophrenia is a relatively minor risk factor for violent behavior. Threats of violence and minor aggressive outbursts are much more common than truly dangerous behavior. Patients who are more likely to commit violent acts include those who abuse drugs and alcohol, have persecutory delusions or command hallucinations, and those who do not take prescribed treatment. Very rarely, severely depressed paranoid patients who feel isolated will attack or kill those they perceive as the sole source of their problems (e.g., an authority figure, a celebrity, a spouse). Most patients with schizophrenia will never be violent. For every person with schizophrenia who commits homicide, 100 commit suicide. [ 67 ] Patients with schizophrenia may present to emergency departments with threats of violence or to obtain food, shelter, and needed care.
Stages
Types of disease progression:
- Continuously progressive, that is, chronic schizophrenia;
- Paroxysmal schizophrenia, which in turn has subtypes
- Fur-like (paroxysmal - progressive);
- Recurrent (periodic).
Stages of schizophrenia:
- Initial. It usually begins with asthenia, apathy and manifests itself with deep depression, psychosis, delirium, hypomania.
- Manifestation. Symptoms intensify, the clinical picture freezes and becomes fixed.
- The final, last stage. Symptoms are usually deficit, the clinical picture freezes.
The degree of speed (progressiveness) of disease development:
- Malignant schizophrenia (rapidly progressive);
- Paranoid schizophrenia (moderately progressive);
- Slow-moving form (low-progressive).
Forms
Five forms of schizophrenia have been described: paranoid, disorganized, catatonic, residual, and undifferentiated. Paranoid schizophrenia is characterized by delusions and auditory hallucinations with intact cognitive functioning and affect. Disorganized schizophrenia is characterized by disorganization of speech and behavior, and flattened or inappropriate affect. In catatonic schizophrenia, physical symptoms predominate, including either immobility or excessive motor activity and the adoption of bizarre postures. In undifferentiated schizophrenia, symptoms are mixed. In residual schizophrenia, there is a clear anamnestic evidence of schizophrenia with more pronounced symptoms, followed by a long period of moderately expressed negative symptoms.
Some experts, on the contrary, classify schizophrenia into deficit and non-deficit subtypes based on the presence and severity of negative symptoms, such as flattened affect, insufficient motivation, and decreased goal-directedness. Patients with the deficit subtype are dominated by negative symptoms without taking into account other factors (i.e., depression, anxiety, insufficient environmental stimulation, side effects of medications). Patients with the non-deficit subtype may have delusions, hallucinations, and thought disorders, but they have virtually no negative symptoms.
Diagnostics schizophrenias
There are no specific tests to diagnose schizophrenia. Diagnosis is based on a comprehensive assessment of the patient's history, symptoms, and signs. [ 76 ] Information from additional sources such as family, friends, teachers, and co-workers is often helpful. According to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), diagnosis requires two or more characteristic symptoms (delusions, hallucinations, disorganized speech, disorganized behavior, negative symptoms) present for a significant portion of the time during a month, prodromal symptoms of illness or microsymptoms with social, occupational, and self-care impairments must be evident for a 6-month period, including 1 month of overt symptoms.
Psychosis due to other medical conditions or substance abuse must be excluded by review of the patient's history and testing, including laboratory tests and neuroimaging. Although structural brain abnormalities are found in some patients with schizophrenia, they are not specific enough to be diagnostic.
Other mental disorders with similar symptoms include some schizophrenia-related disorders: transient psychotic disorder, schizophreniform disorder, schizoaffective disorder, and delusional disorder. In addition, mood disorders can cause psychosis in some people. Some personality disorders (especially schizoid) present with symptoms similar to schizophrenia, although they are usually milder and not psychotic.
When psychosis develops, the first step is to try to establish its cause. If the cause is known, then treatment and prevention can be more specific. The fact that an accurate diagnosis is the key to effective therapy can be seen in the example of delusional symptoms, which can be a manifestation of not only schizophrenia, but also temporal epilepsy, amphetamine addiction, and the manic phase of affective disorder. Each of these cases requires special treatment.
Differential diagnosis
The algorithm for differential diagnosis of schizophrenia can be found in the 4th revision of the Diagnostic and Statistical Manual of Mental Disorders of the American Psychiatric Association (DSM-IV). According to this algorithm, in a patient with psychosis, somatic diseases and substance abuse should be ruled out first. Then it should be established whether the symptoms are caused by an affective disorder. If not, then, depending on the clinical picture, a diagnosis of schizophrenia or schizotypal disorder is made. Although the treatment of psychotic disorders of various origins has its own characteristics, in all cases, as a rule, neuroleptics are used.
 [ 81 ], [ 82 ], [ 83 ], [ 84 ], [ 85 ], [ 86 ], [ 87 ], [ 88 ], [ 89 ], [ 90 ]
[ 81 ], [ 82 ], [ 83 ], [ 84 ], [ 85 ], [ 86 ], [ 87 ], [ 88 ], [ 89 ], [ 90 ]
Who to contact?
Treatment schizophrenias
Schizophrenia is definitely a condition that requires referral for psychiatric treatment. And here it is not at all necessary that there is a direct connection between psychotic experiences and the crime committed. It is quite enough that the subject is ill. In general, as practice confirms, if the crime is not associated with positive psychotic symptoms, then it is associated with a decrease in the patient's personality as a result of the disease. At the same time, of course, one can meet people whose crime is part of their life criminal pattern and who - it so happened - fell ill with schizophrenia, but in general, people who currently need psychiatric treatment should be offered such treatment. This does not always happen, especially in the absence of satisfactory inpatient services. If, on the one hand, the subject commits a crime while in complete remission, and this is part of his criminal "career", then he is responsible for his actions. Schizophrenia can be so severe that the subject can be recognized as incompetent to participate in the trial. This disease is the basis for reduced liability in cases of murder and can be the basis for the application of the MacNaughten Rules.
The time from the onset of psychotic symptoms to the start of treatment correlates with the rapidity of the initial therapeutic response, the quality of the therapeutic response, and the severity of negative symptoms. Early treatment usually results in a more rapid and complete response. If untreated during the first episode, 70–80% of patients will develop a subsequent episode within 12 months. Long-term use of antipsychotics can reduce the relapse rate by approximately 30% over 1 year.
The main goals of treatment are to reduce the severity of psychotic symptoms, prevent exacerbations of symptoms and related impairments in functioning, and help the patient function at the highest possible level. Antipsychotics, community-based rehabilitation, and psychotherapy are the main components of treatment. Given that schizophrenia is a long-term and recurrent illness, teaching patients self-help skills is an important goal of therapy.
Based on affinity for specific neurotransmitter receptors and activity, drugs are divided into typical antipsychotics (neuroleptics) and second-generation antipsychotics (SGAs). SGAs may have certain advantages, consisting of slightly greater efficacy (although for some SGAs these advantages are controversial) and a reduced likelihood of hyperkinetic disorders and other side effects.
Treatment of schizophrenia with traditional antipsychotics
The mechanism of action of these drugs is primarily related to the blockade of dopamine D 2 receptors (dopamine-2 blockers). Traditional antipsychotics can be divided into high-, intermediate-, and low-potency. High-potency antipsychotics have a higher affinity for dopamine receptors and a lower affinity for adrenergic and muscarinic receptors. Low-potency antipsychotics, which are rarely used, have a lower affinity for dopamine receptors and a relatively higher affinity for adrenergic, muscarinic, and histamine receptors. The various drugs are available as tablets, liquids, short-acting, and long-acting intramuscular injections. The choice of drug is based primarily on the side effect profile, the desired route of administration, and the patient's previous response to the drug.[ 91 ]
Traditional antipsychotics
Class |
Preparation (boundaries) |
Daily dose |
Average dose |
Comments |
Aliphatic phenothiazines |
Chlorpromazine |
30-800 |
400 mg orally at bedtime |
Prototype of low potency drugs. Also in rectal suppositories |
Piperidine |
Thioridazine |
150-800 |
400 mg orally at bedtime |
The only drug with an absolute maximum dose (800 mg/day) - in high doses it causes pigment retinopathy and has a pronounced anticholinergic effect. Additional warnings are included in the instructions due to prolongation of QTk |
Dibenzoxazepines |
Loxapine |
20-250 |
60 mg orally at bedtime |
Has affinity for dopamine D- and serotonin 5HT-receptors |
Dihydroindolones |
Molindon |
15-225 |
60 mg orally at bedtime |
May cause weight loss |
Thioxanthenes |
Thiothixene |
8-60 |
10 mg orally at bedtime |
High incidence of akathisia |
Butyrophenones |
Haloperidol |
1-15 |
4 mg orally at bedtime |
Prototype of high potency drugs; haloperidol decanoate (i/m depot) is available. Akathisia is common |
Diphenyl butylpyridines |
Pimozide |
1-10 |
3 mg orally at bedtime |
Approved only for Tourette syndrome |
Piperazine |
Trifluoperazine Fluphenazine Perphenazine 2 ' 3 |
2-40 0.5-40 12-64 |
10 mg orally at bedtime 7.5 mg orally at bedtime 16 mg orally at bedtime |
There are also fluphenazine decanoate and fluphenazine enanthate, which are depot forms (there are no dose equivalents) |
QTk - 07" interval corrected for heart rate.
1 Current recommendations for starting typical antipsychotics are to start with the lowest dose and titrate up to the required dose; bedtime is recommended. There is no evidence that rapid dose escalation is more effective. IM formulations are available for acute treatment.
Conventional antipsychotics have some serious side effects, including sedation, confusion, dystonia or muscle rigidity, tremor, elevated prolactin levels, and weight gain (to treat the side effects). Akathisia (motor restlessness) is particularly troublesome and may lead to poor compliance. These drugs may also cause tardive dyskinesia, an involuntary movement disorder most often characterized by wrinkling of the lips and tongue and/or a "twisting" sensation in the arms or legs. The incidence of tardive dyskinesia is about 5% per year of medication use among patients taking conventional antipsychotics. In about 2% of cases, tardive dyskinesia is severely disfiguring. In some patients, tardive dyskinesia persists indefinitely, even after the medication is stopped.
Two traditional antipsychotics and one antipsychotic are available as long-acting depot preparations. These preparations are used to avoid drug incompatibilities. They can also help patients who, due to disorganization, indifference, or aversion to the disease, are unable to take their medications orally on a daily basis.
Depot antipsychotics
Preparation 1 |
Dosage |
Time to peak 2 |
Fluphenazine decanoate |
12.5-50 mg every 2-4 weeks |
1 day |
Fluphenazine enanthate |
12.5-50 mg every 1-2 weeks |
2 days |
Haloperidol decanoate |
25-150 mg every 28 days (possibly every 3-5 weeks) |
7 days |
Risperidone Microspheres S |
25-50 mg every 2 weeks |
35 days |
1 Administered intramuscularly using the Z-track technique.
2 Time to peak level after a single dose.
Since there is a 3-week delay between the first injection and achieving adequate blood levels, the patient should continue oral antipsychotic therapy for 3 weeks after the first injection. It is recommended to assess tolerability before initiating therapy with oral risperidone.
Clozapine is the only SGA that has been shown to be effective in approximately 50% of patients resistant to traditional antipsychotics. Clozapine reduces negative symptoms, causes virtually no motor side effects, has a minimal risk of developing tardive dyskinesia, but causes other undesirable effects such as sedation, hypotension, tachycardia, weight gain, type 2 diabetes mellitus, and increased salivation. Clozapine can also cause seizures, this effect is dose-dependent. The most severe side effect is agranulocytosis, which can develop in approximately 1% of patients. Therefore, frequent monitoring of the white blood cell count is necessary, and clozapine is usually used as a reserve drug in patients who do not respond adequately to other drugs. [ 92 ], [ 93 ]
The newer SGAs have many of the advantages of clozapine without the risk of agranulocytosis and are generally preferred over traditional antipsychotics for the treatment of acute episodes and prevention of exacerbations. The newer SGAs are very similar in efficacy but have different side effects, so the choice of drug is based on individual susceptibility and other drug characteristics. For example, olanzapine, which has a relatively high risk in patients receiving long-term maintenance therapy, should be assessed at least every 6 months. Rating tools such as the Abnormal Involuntary Movement Scale may be used. Neuroleptic malignant syndrome is a rare but potentially fatal adverse event characterized by muscle rigidity, fever, autonomic instability, and elevated creatinine phosphokinase.
Approximately 30% of patients with schizophrenia do not respond to traditional antipsychotics. In these cases, clozapine, a second-generation antipsychotic, may be effective.
Treatment of schizophrenia with second-generation antipsychotics
Second-generation antipsychotics act by blocking both dopamine and serotonin receptors (serotonin-dopamine receptor antagonists). SGAs generally reduce positive symptoms; may reduce negative symptoms to a greater extent than traditional antipsychotics (although such differences are controversial); may cause less cognitive impairment; are less likely to cause extrapyramidal (motor) side effects; have a lower risk of developing tardive dyskinesia; some SGAs do not cause or cause only a slight increase in prolactin levels.
Pathological Involuntary Movement Scale
- Observe the patient's gait on the way to the office.
- Ask the patient to remove chewing gum or dentures if they are causing problems.
- Determine if the patient is aware of some movements.
- Have the patient sit on a firm chair without armrests, with hands on the lap, legs slightly apart, and feet flat on the floor. Now and throughout the examination, observe the patient's entire body to assess movement.
- Instruct the patient to sit with their arms hanging unsupported over their knees.
- Ask the patient to open his mouth twice. Watch the tongue movements.
- Ask the patient to stick out his tongue twice.
- Ask the patient to tap the thumb on the other fingers of the hand for 15 seconds on each hand. Observe the face and legs.
- Ask the patient to stand with his arms extended forward.
Rate each item on a scale from 0 to 4 according to the degree of increase in severity. 0 - none; 1 - minimal, may be the extreme limit of the norm; 2 - mild; 3 - moderate; 4 - severe. If movements are observed only after activation, they should be rated 1 point less than those that appear spontaneously.
Facial and oral movements |
Facial expressions Lips and perioral area Jaws Language |
Limb movements |
Hands Legs |
Torso movements |
Neck, shoulders, hips |
General conclusion |
Severity of pathological movements Failure due to pathological movements Patient's awareness of abnormal movements (0 - not aware; 4 - severe distress) |
Adapted from: ECDEU Assessment Manual for Psychopharmacology by W. Guy. Copyright 1976 by US Department of Health, Education and Welfare.
Weight gain, hyperlipidemia, and increased risk of type 2 diabetes are the major adverse effects of ACE inhibitors. Therefore, before initiating treatment with ACE inhibitors, all patients should be screened for risk factors, including personal/family history of diabetes, weight, waist circumference, blood pressure, fasting blood glucose, and lipid profile. Patients and families should be educated about the signs and symptoms of diabetes (polyuria, polydipsia, weight loss), including diabetic ketoacidosis (nausea, vomiting, dehydration, rapid breathing, blurred vision). In addition, all patients starting ACE inhibitors should be counseled about nutrition and physical activity. All patients treated with antipsychotics require periodic monitoring of body weight, body mass index (BMI), fasting glucose levels and should be referred for special evaluation if hyperlipidemia or type 2 diabetes mellitus develops. Neuroleptic malignant syndrome has been associated with virtually all antipsychotic drugs, including the newly marketed neuroleptics.[ 94 ]
Second generation antipsychotics 1
LASS |
Preparation |
Dose limits |
Average adult dose |
Comments |
Dibenzodiazepines |
Clozapine |
150-450 mg orally 2 times a day |
400 mg orally at bedtime |
First ASA to show efficacy in treatment-resistant patients. Requires frequent monitoring of white blood cell counts due to risk of agranulocytosis; increases risk of seizures, weight gain |
Benzoxazoles |
Risperidone |
4-10 mg orally before bedtime |
4 mg orally at bedtime |
May cause extrapyramidal symptoms at doses >6 mg; dose-dependent increase in prolactin levels; the only ASAID with a long-acting injectable form |
Thienobenzodiazepines |
Olanzapine |
10-20 mg orally before |
15 mg orally at bedtime |
Somnolence, weight gain and dizziness are the most common side effects. |
Dibenzothiazepines |
Quetiapine |
150-375 mg orally 2 times a day |
200 mg orally 2 times daily |
Low potency allows for wide dosing; no anticholinergic effect. Dose titration is necessary due to a-receptor blockade; twice daily administration is necessary |
Benzisothiazolylpiperazines |
Ziprasidone |
40-80 mg orally 2 times a day |
80 mg orally 2 times daily |
Inhibits the reuptake of serotonin and norepinephrine, may have antidepressant properties. Shortest half-life of new drugs; requires twice daily administration with food. For acute conditions, an intramuscular form is available. Low tendency to increase body weight |
Dihydrocarostyril |
Aripiprazole |
10-30 mg orally before |
15 mg orally at bedtime |
Partial dopamine-2 receptor agonist, low tendency to weight gain |
APVPs are second-generation antipsychotics.
1 Monitoring for weight gain and development of type 2 diabetes is recommended for this class of antipsychotics.
All second-generation antipsychotics are associated with increased mortality in elderly patients with dementia.
Treatment of schizophrenia with atypical neuroleptics began almost simultaneously with the beginning of the prescription of typical neuroleptics to patients with schizophrenia.
Rehabilitation and social support services
Psychosocial skills training and vocational rehabilitation programs help many patients work, shop and care for themselves, manage their household, get along with others, and collaborate with mental health professionals. Employment maintenance can be especially valuable when the patient is placed in a competitive work environment and provided with a workplace mentor to facilitate adjustment to work. Over time, the workplace mentor acts only as a backup for decision making or communication with employers.
Community-based support services enable many people with schizophrenia to live in the community. Although most patients can live independently, some require supervised housing, where staff are present to ensure medication compliance. Programs provide graded levels of supervision in a variety of settings, ranging from 24-hour support to periodic home visits. These programs help ensure patient autonomy, while providing appropriate medical care reduces the likelihood of relapses and the need for hospitalization. Community-based treatment programs operate in the patient's home or other setting and have high staff-to-patient ratios; treatment teams directly provide most or all of the necessary treatment.
During severe exacerbations, hospitalization or crisis intervention in a hospital may be required, as well as involuntary hospitalization if the patient poses a danger to themselves or others. Despite better rehabilitation and social services, a small number of patients, especially those with severe cognitive deficits and those resistant to treatment, require long-term hospital stays or other supportive care.
Psychotherapy
Current models of psychotherapy for schizophrenia, tempered to a large extent by disappointing past efforts, are more modest and pragmatic in their aims and are seen as part of a comprehensive treatment with pharmacological interventions at the core. [ 95 ] The goal of psychotherapy is to develop an integrated relationship between the patient, family, and physician so that the patient can learn to understand and manage his or her illness, take medications as prescribed, and cope with stress more effectively. Although a common approach is to combine individual psychotherapy with medication, there are few practical guidelines for this. The most effective psychotherapy is one that begins by addressing the patient's basic social needs, provides support and education about the nature of the illness, promotes adaptive functioning, and is based on empathy and a proper dynamic understanding of schizophrenia. Many patients require empathic psychological support in adapting to the fact that the illness is often a lifelong disorder that can significantly limit functioning.
For patients living with their families, psychoeducational family interventions may reduce relapse rates. Supportive and advocacy groups such as the National Alliance on the Mentally Ill are often helpful to families.
More information of the treatment
Forecast
During the first 5 years after onset of the disease, functioning may be impaired, social and professional skills may decline, and self-care neglect may progressively increase. Negative symptoms may increase in severity, and cognitive functioning may decline. Thereafter, impairments reach a plateau. There is some evidence that the severity of the disease may decrease with age, especially in women. Hyperkinetic disorders may develop in patients with severe negative symptoms and cognitive dysfunction, even if antipsychotics are not used.
The prognosis varies depending on the form of schizophrenia. Patients with paranoid schizophrenia have less disability and respond better to treatment. Patients with the deficit subtype are usually more disabled, have a worse prognosis, and are more resistant to therapy.
Schizophrenia may be associated with other mental disorders. [ 96 ] If it is associated with obsessive-compulsive symptoms, the prognosis is particularly poor; if with borderline personality disorder symptoms, the prognosis is better. About 80% of people with schizophrenia experience one or more episodes of major depression at some point in their lives.
During the first year after diagnosis, the prognosis is closely related to strict adherence to the prescribed psychotropic medication. Overall, 1/3 of patients achieve significant and lasting improvement; 1/3 show some improvement but have periodic exacerbations and residual impairment; 1/3 have severe and persistent symptoms. Only 15% of all patients fully return to the pre-illness level of functioning. Factors associated with a good prognosis include good pre-illness functioning (eg, good academic performance, successful work), late and/or sudden onset of illness, family history of mood disorders other than schizophrenia, minimal cognitive impairment, mild negative symptoms, and paranoid or non-deficit form. Factors associated with a poor prognosis include early age of onset, poor pre-illness functioning, family history of schizophrenia, and disorganized or deficit subtype with multiple negative symptoms. Men have worse outcomes than women; women respond better to antipsychotic therapy.
Alcohol and drug abuse are significant problems in approximately 50% of people with schizophrenia. Anecdotal evidence suggests that marijuana and other hallucinogens can be extremely destructive in people with schizophrenia and should be discouraged. Co-occurring substance abuse is a strong predictor of poor outcome and can lead to non-adherence to medication, relapses, frequent hospitalizations, decreased functioning, and loss of social support, including homelessness.

