Medical expert of the article
New publications
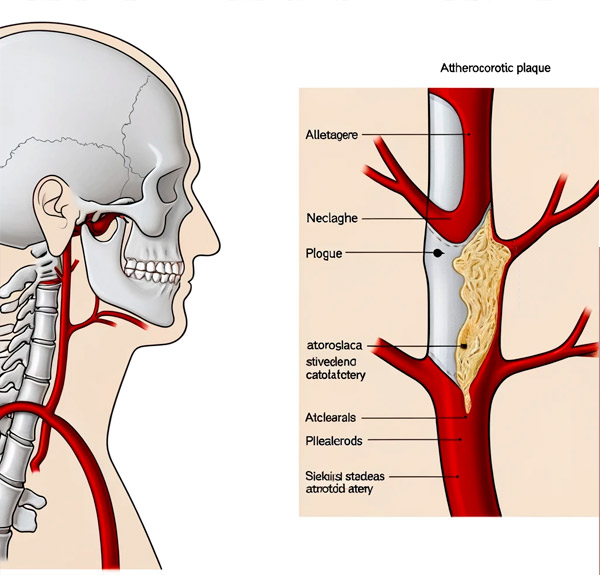
Plaque in the carotid artery in the cervical region.
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Although the common carotid artery (a. Carotis communis), which is part of the brachiocephalic (brachial) trunk, divides into two arteries (external and internal), the carotid plaque in the cervical carotid artery usually forms in the internal carotid artery (a. Carotis interna), which runs up the neck through the connective tissue formation of its fascial layers. [1]
Causes of the carotid plaque
Plaques are cholesterol deposits on the vascular wall of arteries - in its inner lining (tunica intima), consisting of endothelium - a thin layer of single endothelial cells (endotheliocytes), which is supported by an inner elastic lamina that forms the boundary between the inner and middle lining (tunica media) of the vessel wall.
The reasons for the formation of atheromatous or atherosclerotic plaques lie in a disorder of lipid (fat) metabolism and hypercholesterolemia - an increase in blood cholesterol and circulating low-density lipoprotein (LDL) levels, which leads to the development of carotid atherosclerosis.
As experts note, the typical place of atherosclerotic plaque development is the cervical part (pars cervicalis) of the internal carotid artery near the bifurcation (separation) of the common carotid or carotid artery - at the level of the fourth cervical vertebra (or at the level of the hyoid bone within the trigonum caroticum - the carotid triangle of the neck).
Depending on the state of the internal lumen of the affected artery and its ability to participate in the systemic blood flow differentiate: non-stenosing atherosclerosis (with hemodynamically insignificant narrowing of the vascular lumen) and stenosing atherosclerosis (when the plaque prevents normal blood flow).
Pathogenesis
It is generally believed that atherogenesis begins with damage to the endothelium of the inner lining of vessels, which leads to the accumulation and adhesion of low-density lipoproteins in the subendothelial space - with the formation of fatty deposits (oxidized LDL), which then undergo fibrosis and calcification. [2] As a result, the vascular wall thickens and loses elasticity, and the plaque protrudes into the vessel lumen and narrows it, which reduces the normal blood flow to the brain.
The pathogenesis of the atherosclerotic process with plaque formation is discussed in detail in publications:
Symptoms of the carotid plaque
Nonstenotic atherosclerosis is asymptomatic in most patients.
In arterial insufficiency of the carotid arteries due to significant narrowing of their lumen by atherosclerotic plaques, symptoms may occur: [3]
- Weakness;
- Frequent dizziness and noise in the head;
- Sudden onset intense headaches;
- A momentary loss of balance;
- Intermittent fainting spells;
- Paresthesia (numbness) in part of the face or arm;
- With temporary visual impairments.
Complications and consequences
A plaque in the carotid artery in the neck can slowly squeeze the artery, reducing blood flow. Or when the plaque ruptures, a blood clot (thrombus) may suddenly form, blocking some or all of the blood flow to the brain. [4] There can be serious complications and consequences, including:
- Carotid stenosis;
- Development of dyscirculatory encephalopathy due to impaired trophicity of brain tissue - with cognitive impairment;
- Occurrence of transient ischemic attacks (mini-strokes);
- Ischemic stroke.
Clinical statistics show the presence of atherosclerotic lesions of the carotid arteries in 20-25% of patients with ischemic stroke and transient ischemic attacks.
Diagnostics of the carotid plaque
In addition to medical examination and collection of anamnesis, the diagnosis of atherosclerotic lesions of arterial vessels involves mandatory laboratory tests: general and biochemical blood tests; coagulogram; for the level of total cholesterol, LDL (low-density lipoprotein), HDL (high-density lipoprotein) and triglycerides in serum; for antibodies to endothelial cells.
Visualizes vessels instrumental diagnostics: ultrasound vascular Dopplerography, duplex scanning of the vessels of the head and neck, CT angiography, MR angiography.
The differential diagnosis includes carotid artery dissection, atherosclerosis of vertebral arteries of the neck, atherosclerosis of cerebral vessels, cerebral amyloid angiopathy, and a rare vascular pathology of the internal carotid artery - fibrous muscular dysplasia of its inner sheath.
Who to contact?
Treatment of the carotid plaque
Details in the articles:
Surgical treatment may include removal of the atherosclerotic plaque (carotid endarterectomy), carotid angioplasty or stenting.
Prevention
Measures of prevention of atherosclerotic plaque formation in vessels of any localization are:
- Adherence to the principles of a healthy lifestyle;
- Treatment for high cholesterol;
- Diet for high cholesterol.
Literature
- Kirienko, Saveliev, Azaryan: Vascular Surgery. National manual. Brief edition. Publisher: GEOTAR-Media, 2020.
- Shlyakhto, E. V. Cardiology: national guide / ed. By E. V. Shlyakhto. - 2nd ed., revision and supplement. - Moscow: GEOTAR-Media, 2021

