Medical expert of the article
New publications
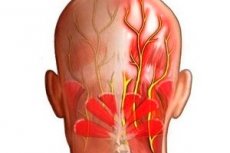
Occipital nerve entrapment
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Epidemiology
Separate clinical statistics of these disorders of the occipital nerves are not kept: the number of patients with long-term primary or secondary headaches is taken into account.
According to experts from the American Osteopathic Association, the prevalence of neurological headaches in the general population is 4%, and among patients suffering from severe cephalgia, it reaches 16-17.5%.
According to the American Migraine Foundation (AMF), occipital neuralgia is diagnosed in no more than three to four people per 100,000 population each year.
As noted, the majority of patients are over 40 years old, and the ratio of men to women with neuralgic pain in the back of the head is 1:4.
Causes occipital nerve entrapment
The pathological condition called occipital neuralgia was first described almost two centuries ago. Etiologically, spontaneously developing intense pain in the occipital part of the head may be associated with compression of the occipital nerve.
The greater occipital nerve (nervus occipitalis major), which innervates the occipital and parietal regions of the head, is formed by the dorsal branch of the second spinal cervical nerve, which runs between the facet-shaped cervical vertebrae C1 (atlas) and C2 (axis) and, bending around the inferior oblique muscle of the head (obliquus capitis inferior musculus) and passing through the ligament of the musculus trapezius (ligament of the trapezius muscle), forms several branches at once. The longest of them - first appearing subcutaneously, and then moving to the back of the head - is the greater afferent (sensory) occipital nerve.
The fibers of the anterior branches of the cervical nerves form the minor occipital nerve (nervus occipitalis minor), which supplies cutaneous sensitivity to the lateral surfaces of the head, including behind the ears, and also innervates the posterior cervical muscles. In addition, the branch of the third cervical nerve, which passes medially to the greater occipital and ends in the skin of the lower part of the back of the head, is considered the third occipital nerve (nervus occipitalis tertius), which innervates the joint of the second cervical vertebra and the intervertebral disc between it and the third cervical vertebra.
Noting the most probable causes of occipital nerve entrapment, neurologists name:
- compression of nerve fibers due to traumatic changes in normal anatomical structures (for example, between a muscle and the occipital bone or between the layers of muscles of the upper and back of the neck);
- atlantoaxial osteoarthritis (osteoarthritis of the cervical vertebrae C1-C2) or cervical osteochondrosis;
- spondylolisthesis or displacement of the cervical vertebrae;
- fibrous thickening of muscle tissue in the neck area or myogelosis of the cervical spine;
- intramuscular formations (cyst, lipoma), for example, in the area of the deep splenius muscle (musculus splenius capitis) at the back of the neck;
- spinal cavernous (vascular) anomalies in the form of arteriovenous malformations;
- intramedullary or epidural tumors of the spine in the cervical region.
Risk factors
Key risk factors for occipital nerve entrapment include any spinal injuries in the neck area. Particularly notable are atlantoaxial rotatory subluxation and so-called whiplash injuries: when, as a result of car accidents, sudden blows to the head or falls, the head is strongly tilted forward, backward or to the side (with a sharp change in the position of the cervical vertebrae).
In addition to extreme factors, a real threat of pinching these nerves is posed by pathological changes in the biomechanics of the anatomical structures that support the stability of the cervical spine. This refers to regional muscle deformation due to constant posture disorders in the so-called crossed proximal muscle imbalance syndrome: tension in some muscles of the neck (with worsening kyphosis of the cervical spine), shoulder girdle and anterior chest, and simultaneous weakening of diagonally located muscles.
Pathogenesis
When the occipital nerve is pinched, the pathogenesis directly depends on the localization and specificity of the injury. Thus, with osteoarthrosis of the cervical vertebrae, compression of the nerve fiber by a bone growth - osteophyte - can occur, and in cases of their displacement, the stability of the cervical spine is disrupted, and the nerve can be pinched between the vertebral bodies.
In most cases, with arthrosis of the first two cervical vertebrae, as well as with pathological changes in the zygapophyseal (zygapophysial) joint C2-C3, there is peripheral pinching of the greater occipital nerve in the craniovertebral junction zone - the place where the spinal column “joins” the skull.
Specialists also know other points of potential compression along the course of the greater occipital nerve: near the spinous process of the first vertebra; at the entrance of the nerve to the semispinalis or trapezius muscle; at the exit from the fascia of the trapezius muscle to the line of the occipital crest - in the area of the occipital protuberance.
If at least one of these points the muscle fibers are in a state of hypertonicity for a long time, a compression effect on the axons of the occipital nerve passing through them occurs with increased excitation of pain receptors.
Symptoms occipital nerve entrapment
The result of pinched occipital nerve, and, in fact, its consequences and complications, is occipital neuralgia, the symptoms of which are manifested by one-sided shooting or stabbing headaches in the neck (at the base of the skull) and the back of the head.
Moreover, unlike migraine, the first signs of neuralgic pain of this etiology do not include a prodromal period and are not accompanied by an aura.
Patients may also experience:
- burning and throbbing pain that spreads from the neck area to the scalp (back and sides);
- retro and supraorbital pain (localized around and behind the eyeball);
- increased sensitivity to light and sound;
- cutaneous hyperpathy (increased superficial sensitivity along the course of the pinched nerve);
- dizziness and ringing in the ears;
- nausea;
- pain in the neck and back of the head when turning or tilting the head.
Between attacks of shooting pain, less acute pain of a constant nature is also possible.
Diagnostics occipital nerve entrapment
The diagnosis of occipital nerve entrapment is made by neurologists based on a combination of anamnesis, clinical signs, palpation of the neck and the results of a diagnostic block (administration of a local anesthetic).
Diagnostic injections (which, in the case of compression, lead to pain relief) are given into the atlantoaxial joint, the zygapophyseal joints C2-3 and C3-4, the nervus occipitalis major and nervus occipitalis minor, and the third occipital nerve.
To visualize the cervical spine and surrounding occipital soft tissues and assess their condition, instrumental diagnostics are performed using magnetic resonance imaging - positional and kinetic. Conventional radiography and CT are useful for identifying arthritis, spondylosis, vertebral displacement and pathological bone formations in this localization.
Differential diagnosis
Since neuralgia due to a pinched nerve can be confused with migraine (hemicrania) or headaches of other etiologies, differential diagnosis is of particular importance. Differential diagnosis includes tumors, infections (brain inflammation, arachnoiditis), myofascial syndrome, congenital anomalies, etc.
Who to contact?
Treatment occipital nerve entrapment
Before visiting a doctor and undergoing an examination, the patient does not know that his excruciating occipital pain is a consequence of a pinched nerve, so only after determining the exact diagnosis will the doctor explain what to do if the occipital nerve is pinched and prescribe appropriate symptomatic treatment.
There is a wide range of conservative (medicinal) means for pain relief. In particular, various medications are used, including non-steroidal anti-inflammatory drugs (NSAIDs), such as Ibuprofen (Ibuprom, Ibufen, Imet, Nurofen) and other analgesics. For details, see - Tablets for neuralgia.
In cases of neuropathic pain, the effectiveness of oral antiepileptic drugs such as Pregabalin, Gabapentin (Gabalept, Meditan, Tebantin) or Carbamazepine, which reduce the activity of nerve cells similar to the inhibitory neurotransmitter gamma-aminobutyric acid (GABA), has been recognized.
For example, Pregabalin can be prescribed to adults at 0.05-0.2 g three times a day. However, these drugs can cause side effects in the form of dizziness, dry mouth, vomiting, drowsiness, tremors, as well as disturbances in appetite, urination, coordination of movements, attention, vision, consciousness and sexual functions.
In difficult cases, the muscle relaxant Tolperisone (Mydocalm) is used to relax the neck muscles - 50 mg three times a day. Among its side effects are nausea, vomiting, arterial hypotension, headache.
It is recommended to use capsaicin ointments (Kapsikam and Nikoflex) locally, the analgesic effect of which is due to the neutralization of the tachykinin neuropeptide of nerve endings. Analgesic cream with lidocaine Emla and 5% lidocaine ointment, as well as ointment with procaine Menovasan also relieve pain well without side effects.
On the recommendation of a doctor, homeopathy can be used to relieve pain, in particular, such remedies as: Aconite, Arsenicum, Belladonna, Bryonia, Colocynthis, Pulsatilla, Spigelia, Gelsemium, Glonoinum, Nux Vom. The dosage of the drugs is determined by a homeopathic doctor.
Interventional treatment of pain syndrome is performed by injections of anesthetic (Lidocaine) and steroid (Hydrocortisone) into the occipital nerve area. The duration of the analgesic blockade is about two weeks (in some cases longer).
Longer-term pain relief (for several months) is possible by introducing botulinum toxin A (BoNT-A) into the trigger zone, which reduces neuronal activity. In order to stop the flow of pain signals to the brain, pulsed radiofrequency stimulation of the occipital nerves is performed.
Yoga and acupuncture sessions are advisable, as well as physiotherapy treatment aimed at strengthening muscles and improving posture; for more details, read - Physiotherapy for neuritis and neuralgia of peripheral nerves. Myofascial therapy helps relieve pain using therapeutic massage, which causes blood flow to the tissues and has a positive effect on muscles, tendons and ligaments.
Among the remedies offered by folk medicine, a hot shower, alternating cold and hot compresses on the occipital region (relieving headaches) can be useful. Also, some advise applying a composition made from chloroform and acetylsalicylic acid (Aspirin) tablets dissolved in it to the painful area.
It should be borne in mind that herbal treatment - taken internally as decoctions of feverfew or skullcap - does not provide a quick pain-relieving effect. And tea with peppermint leaves simply calms the nerves.
Also read – Treatment of Neuropathic Pain.
Surgical treatment
If all conservative pain relief therapy is ineffective, surgical treatment is possible using:
- selective radiofrequency rhizotomy (destruction) of nerve fibers;
- radiofrequency neurotomy (ablation), which involves thermal denervation of the pinched nerve;
- cryoneuroablation;
- radiofrequency neurolysis (excision of tissue causing compression of the occipital nerve);
- microvascular decompression (when a nerve fiber is pinched by blood vessels), in which, during a microsurgical operation, the vessels are moved away from the site of compression.
According to experts, even after surgical treatment, almost a third of patients continue to suffer from headaches, so the benefits of surgery should always be carefully weighed against its risks: the possibility of developing causalgia or a painful nerve tumor (neuroma).
 [ 5 ]
[ 5 ]
Prevention
What can prevent occipital nerve impingement consist of? Preventing injuries to the cervical vertebrae and the entire spine; correct posture; sufficient physical activity; a healthy diet containing all the necessary vitamins and micro and macroelements. In general, a conscious attitude to your health.
 [ 6 ]
[ 6 ]
Forecast
According to neurologists, the long-term prognosis in case of pinching of the greater or lesser occipital nerve depends not only on timely access to a doctor and adequate treatment, but also on the causal factors of this injury.
If the etiology of the compression of the nerve fiber is due to irreversible changes in the corresponding anatomical structures, the treatment of chronic occipital neuralgia becomes lifelong.

