Medical expert of the article
New publications
Piloid astrocytoma
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
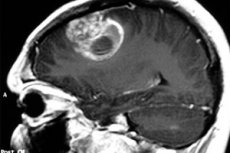
The medical term pilocytic astrocytoma is used to refer to neoplasms formerly called cystic cerebral astrocytomas, either hypothalamic-parietal gliomas or juvenile pilocytic astrocytomas. The tumor process originates from neuroglia and most commonly affects pediatric and adolescent patients, although it can occur in the elderly. The tumor can be either benign or malignant. Treatment is predominantly surgical. [1]
Epidemiology
The name "piloid" has been known since the 1930s. It was used to describe astrocytomas with hair-like, bipolar branches in their cellular structure. Currently, piloid astrocytoma is a tumor that previously had many names, including "polar spongioblastoma," "juvenile astrocytoma," and others. Piloid astrocytoma belongs to the category of neoplasms of low malignancy: according to the WHO classification of tumor processes - GRADE I.
Piloid astrocytoma is the most common brain neoplasm in pediatrics. It accounts for more than 30% of all gliomas that develop between the ages of newborn to 14 years, and more than 17% of all primary brain neoplasms in childhood. In addition to children, the disease is frequently reported in young adults 20-24 years of age. In patients over 50 years of age, the pathology is noted less frequently.
Piloid astrocytoma can develop in any part of the central nervous system. Often the disease affects the optic nerve, hypothalamus/chiasma, cerebral hemispheres, basal ganglia/thalamus, and brain stem. But the vast majority of such neoplasms are either piloid astrocytomas of the cerebellum or brainstem tumors.
Causes of the piloid astrocytoma
The underlying causes of piloid astrocytoma development are currently poorly understood. Presumably, some types of tumors are formed at the stage of embryonic development. But scientists have not yet been able to trace the mechanism of origin of this pathology. Nor has it been found out how to prevent or block the development of the disease.
In some cases, it is caused by radiation exposure to the head or neck region for therapy of another pathology. The risks of piloid astrocytoma are slightly higher in patients with neurofibromatosis type 2 and mammary gland tumors. There may be an influence of hormonal background - namely, levels of progesterone, estrogens, and androgens.
Neurosurgical oncologists now have somewhat more information about piloid astrocytoma than they did 20-30 years ago. However, there are still many unresolved issues in the development of this disease. Certainly, among the possible causes of the tumor are radiocausal effects, the influence of oncoviruses, genetic predisposition, adverse effects of bad habits, ecology and occupational hazards. [2]
Risk factors
At the moment, experts cannot name a single guaranteed risk factor for the development of piloid astrocytoma. Nevertheless, information about suspected factors is available:
- Age. The highest number of piloid astrocytomas is reported between 0 and 14 years of age.
- Environmental influences. Regular contacts with pesticides, petroleum products, solvents, polyvinyl chloride, etc. Play a particularly unfavorable role.
- Genetic pathologies. The association of astrocytoma development with neurofibromatosis, tuberous sclerosis, Li-Fraumeni and Hippel-Lindau syndromes, and basal cell nevus syndrome is known.
- Craniocerebral injuries and seizure syndrome, taking anticonvulsants.
- Exposure to ionizing radiation (radon, X-rays, gamma rays, other types of high-energy rays).
Pathogenesis
Piloid astrocytoma is a type of glial tumor. The cellular basis for its development are astrocytes - star-like or spider-like cells, also called neuroglial cells. The purpose of astrocytes is to support neurons, the basic structures of the brain. From these cells depends on the delivery of necessary substances from the walls of blood vessels to the neuronal membrane. Cell structures take part in the formation of the nervous system, maintain fluid intercellular constancy.
Piloid astrocytoma in the white matter of the brain is formed on the basis of fibrous, fibrous cells, and in the gray matter - from protoplasmic cells. Both the first and the second variant provides neuronal protection from aggressive effects of chemical and other traumatic factors. Star-like structures provide nerve cells with nourishment and adequate blood flow in the brain and spinal cord. [3]
The tumor process can most often affect:
- The cerebral hemispheres associated with the processes of memory, problem solving, thinking and feeling;
- The cerebellum, responsible for vestibular and coordination regulation;
- Brain stem, located below the hemispheres and anterior to the cerebellum, responsible for respiratory and digestive functions, heartbeat and blood pressure.
Symptoms of the piloid astrocytoma
The presence of piloid astrocytoma can be suspected when there are problems with motor coordination. In most cases, this symptom indicates disturbances in cerebellar function, which is often due to the development of the tumor. In general, the clinical picture is formed by a confluence of factors such as localization, the size of the neoplasm. The presence of astrocytoma in many patients negatively affects the quality of speech, some patients complain of deterioration of memory and visual function.
Piloid astrocytoma with localization in the left side of the brain can cause paralysis of the right side of the body. Patients have severe and constant headaches, almost all types of sensitivity are affected. Most patients indicate the appearance of severe weakness, disorders of the heart (in particular, arrhythmias, tachycardia). Blood pressure indicators are unstable.
If piloid astrocytoma is located in the pituitary, hypothalamic region, endocrine function is affected. [4]
Depending on the location of piloid astrocytoma, its clinical picture also differs. Nevertheless, the first signs of pathology in most cases are approximately the same. [5] We are talking about such manifestations:
- Head pain (regular, migraine-like, intense, attack-like);
- Dizziness;
- General weakness, brokenness;
- Nausea, sometimes to vomiting, often with intensification in the wee hours of the morning;
- Speech impairments, visual and/or auditory impairments;
- Sudden unmotivated mood swings, behavioral changes;
- Seizures;
- Vestibular disorders;
- Blood pressure fluctuations.
First signs, depending on the localization of piloid astrocytoma:
- Cerebellum: coordination and vestibular disorders.
- Brain hemispheres: right - severe weakness in left limbs, left - weakness in right side of body.
- Frontal brain: personality and behavioral disorders.
- Dark part: disorders of fine motor skills, pathologies of sensations.
- Occipital part: appearance of hallucinations, deterioration of vision.
- Temporal: speech disorders, memory and coordination disorders.
Piloid astrocytoma in children
The symptomatology of piloid astrocytoma in childhood is characterized by its diversity. In some children, manifestations intensify gradually, which is more characteristic of small low malignant tumors.
In general, the pediatric clinical picture depends on both the age of the baby and the location, size, and rate of enlargement of the piloid astrocytoma. [6] The main symptoms often become:
- Pain in the head, with aggravation in the morning and relief after a vomiting fit;
- Nausea and vomiting;
- Visual impairment;
- Vestibular problems (which is noticeable even when walking);
- A feeling of weakness, numbness in half his body;
- Personality, behavioral disorders;
- Seizures;
- Speech and hearing problems;
- A constant and unmotivated feeling of fatigue, sleepiness;
- Deterioration in academic performance and ability to work;
- Weight fluctuations in one direction or another;
- Endocrine disorders;
- In infants - increase in the volume of the head, the size of the fontanel.
Stages
Astrocytoma is classified according to its microscopic characteristics. In addition, the neoplasm is evaluated according to the stage of malignancy: more pronounced structural changes indicate a higher degree of malignancy.
First- and second-degree piloid astrocytomas of the brain are among the less malignant neoplasms. The cells of such tumors appear to be low-aggressive, and their growth is relatively slow. The prognosis of such neoplasms is more favorable.
Third- and fourth-degree astrocytomas are highly malignant, aggressive. They are characterized by rapid growth and development. The prognosis is usually unfavorable.
Low malignant astrocytomas include:
- Juvenile piloid astrocytoma;
- Pilomyxoid astrocytoma;
- -pleomorphic xanthoastrocytoma;
- -giant-cell subependymal, diffuse (fibrillary) astrocytoma.
Highly malignant neoplasms include:
- Anaplastic, pleomorphic anaplastic astrocytoma;
- Glioblastoma;
- Median diffuse glioma.
Complications and consequences
Piloid astrocytoma is a low malignancy neoplasm. Its transformation to a higher grade of malignancy is rare. In patients with piloid astrocytoma, the ten-year survival rate is estimated at about 10%. However, the prognosis for young children in most cases is much worse than for adolescents and older people.
The pathology is a slowly developing tumor that grows in stages. In childhood, the disease more often affects the cerebellum and visual pathway. The basic way to eliminate the pathological process is considered to be surgery. But, unfortunately, not always piloid astrocytoma can be removed surgically. This is due to increased risks of damage to nearby vital structures of the brain.
The following factors have a particular influence on the likelihood of developing adverse effects and complications:
- The degree of malignancy of the tumor process (highly malignant astrocytomas do not respond well to treatment and may recur);
- Localization of the tumor process (cerebellar and hemispheric astrocytomas have a better chance of cure, unlike neoplasms located in the middle or brainstem);
- The age of the patient (the earlier the diagnosis and treatment, the better the prognosis);
- The prevalence of piloid astrocytoma (metastasizing to other parts of the brain or spinal cord);
- Neurofibromatosis type one.
Recurrence of piloid astrocytoma is relatively common. Moreover, tumor recurrence can be observed both within the first three years after surgical removal and in a later period. Nevertheless, some neoplasms even after partial removal stop their growth, which can be equated with cure of the patient.
Metastasis to the spinal cord in piloid astrocytoma
The basis of neoplasm formation does not belong to epithelial tissue, as it has a complex structural organization. When the process becomes malignant, metastasis outside the brain structures is rarely observed. However, numerous foci of atypical cells can form inside the brain, which are spread with the bloodstream from other organs and tissues. Malignant piloid astrocytoma of the spinal cord in this situation is difficult to distinguish from benign. Surgery to remove the neoplasm can be difficult due to the lack of clear outlines.
There is a risk of developing polyclonal tumors - so-called "neoplasms within a neoplasm". The treatment consists of a combination of medications, as the first tumor may respond to some medications and the second tumor to others.
Complex and metastatic astrocytomas are more often diagnosed in children and young people under 30 years of age. The pathology is less often found in the elderly.
Diagnostics of the piloid astrocytoma
Piloid astrocytoma is detected either accidentally or when the patient has obvious neurological symptoms. If a tumor process is suspected, the specialist should review the patient's medical history, perform a thorough examination, check visual and auditory function, vestibular function and coordination of movements, muscle strength and reflex activity. The presence of a problem often indicates the approximate localization of the neoplasm.
Based on the results of the examination alone, the doctor may refer the patient to a neurologist or neurosurgeon for consultation.
As part of the laboratory diagnosis of piloid astrocytoma, tests are performed on liquor, blood and other biological fluids in which tumor cells are most likely to be detected. Hormonal background and oncomarkers are also examined.
Liquor is obtained by spinal puncture: under local anesthesia, a special needle is used to puncture the skin, muscle tissue and spinal cord sheath. Then the necessary volume of fluid is pumped out using a syringe.
Biological fluids are often also used to detect specific microscopic fragments of genetic material. These are biomarkers and oncomarkers. Today, the diagnosis of piloid astrocytoma using oncomarkers is widely used in clinical practice.
Instrumental diagnosis can be represented by the following procedures:
- Magnetic resonance imaging and computed tomography are classic techniques for examining brain structures. Based on the images obtained, the specialist not only identifies the tumor process, but also specifies its localization and type of affiliation. At the same time, magnetic resonance imaging is considered the most optimal study, which is more informative and less harmful to the body, unlike CT.
- PET - positron emission tomography - is used to detect brain neoplasms (especially malignant aggressive tumors). Before the diagnosis, the patient is injected with a radioactive component that lingers in tumor cells.
- A tissue biopsy involves taking and examining the sample obtained. The procedure may be performed alone or as part of surgery to remove a piloid astrocytoma. A stand-alone biopsy is more often practiced if the suspected neoplasm is difficult to access or is localized in vital brain structures with a high risk of damage during surgical intervention.
- Genetic tests help identify mutations in tumor structures.
The diagnosis of piloid astrocytoma almost always needs to be clarified. For this purpose, it is possible to use other auxiliary diagnostic techniques, such as visual field studies, evoked potentials, etc.
Differential diagnosis
Neurinoma, meningioma, cholesteatoma, pituitary adenoma and many other brain tumors are visualized quite well with magnetic resonance imaging. But the detection of gliomas, distinction of astrocytomas from metastases or inflammatory foci can face some difficulties.
In particular, contrast agents do not accumulate in nearly half of benign astrocytomas, creating problems in differentiating tumor and non-tumor disease.
It is important to perform a multifaceted diagnosis to distinguish piloid astrocytoma from non-tumor brain neoplasms, inflammatory pathologies (microbial focal encephalitis, abscess, vascular lesion), and postoperative scar necrotic or granulation abnormalities.
Maximum diagnostic information is provided by a combination of magnetic resonance imaging and positron emission tomography.
Who to contact?
Treatment of the piloid astrocytoma
The range of therapeutic measures in piloid astrocytoma is determined by both the degree of malignancy and the localization of the pathological focus. In the vast majority of cases, as far as possible, surgery is preferred. If the intervention cannot be performed, the emphasis is placed on chemopreparations and radiotherapy.
Piloid astrocytoma develops gradually in most patients, so the body often triggers adaptation mechanisms that "smooth" the symptoms. Early stages of tumor development are better corrected by chemotherapy and radiation therapy. However, piloid astrocytoma of the chiasmal-sellar region often takes an aggressively malignant character and can spread regional metastases around the tumor and along the pathways of cerebrospinal fluid circulation.
In general, the following main treatment methods are used:
- Neurosurgical surgery, which consists of partial or complete removal of the pathological focus;
- Radiation therapy, which involves destroying and blocking further growth of tumor cells using radiation;
- Chemotherapy, which involves taking cytostatic drugs that slow down and destroy malignant structures;
- A radiosurgical method that combines radiation and surgery.
Drug treatment
Patients with piloid astrocytoma are especially indicated for so-called targeted therapy, which is a targeted therapy that targets tumor cells. The drugs used in this treatment affect impulses and processes at the molecular level, which results in blocking the growth, multiplication and interaction of the tumor cells.
Low malignant astrocytomas have an alteration in the BRAF gene, which controls a protein responsible for cell growth and function. Such a disorder is a BRAF V600E point mutation or BRAF doubling. In order to stop the impulses that help tumor cells to grow, appropriate medications are used.
- Vemurafenib and dabrafenib (BRAF inhibitors).
- Trametinib and Selumetinib (MEK inhibitors).
- Sirolimus and Everolimus (mTOR inhibitors).
During the use of Vemurafenib, the patient should have regular blood tests to assess electrolyte levels and monitor liver and kidney function. In addition, the patient should have systematic skin examinations and monitor changes in cardiac activity. Possible side effects: muscle and joint pain, general weakness and fatigue, nausea, loss of appetite, hair loss, rashes, redness, condylomas. Vemurafenib is taken daily at the same time. Tablets are not crushed, drink water. Dosage and duration of administration are determined individually.
Sirolimus is a drug that suppresses the immune system (immunosuppressant). The most common side effects are: increased blood pressure, kidney disorders, fever, anemia, nausea, swelling of the extremities, abdominal and joint pain. The most dangerous adverse effect of taking Sirolimus is considered the development of lymphoma or skin cancer. Throughout the course of treatment, it is important to drink plenty of fluids and protect the skin from ultraviolet exposure. The dosage of the drug is individual.
Steroid and anticonvulsant medications may be used as symptomatic treatment.
Surgical treatment
Surgery allows to remove the maximum number of tumor cells, so it is considered the main method of treatment of piloid astrocytoma. In the early stages of neoplasm development, surgery is most effective, although in some cases it is still impossible due to the risk of damage to nearby brain structures.
The operation does not require any specific preparation. The only exception is the need for the patient to take a fluorescent solution - a substance that accumulates in the neoplasm, which improves its visualization and reduces the risk of affecting nearby vessels and tissues.
Most often general anesthesia is used during surgery. If the piloid astrocytoma is located near the most important functional centers (such as speech, vision), the patient is left conscious.
Two types of surgery are commonly used to treat piloid astrocytoma of the brain:
- Endoscopic skull trepanation - involves removal of the tumor using an endoscope that is inserted through small holes. The intervention is minimally invasive and lasts on average 3 hours.
- Open intervention - involves removal of part of the cranial bone followed by microsurgical manipulation. The intervention lasts up to 5-6 hours.
After the operation, the patient is admitted to the intensive care unit. The patient stays there for approximately one week. To assess the quality of the treatment, computerized or magnetic resonance imaging diagnostics is additionally performed. If it is confirmed that there are no complications, the patient is transferred to a rehabilitation ward or clinic. The full rehabilitation period lasts about three months. The rehabilitation program usually includes therapeutic exercise, massage, psychological and speech therapy consultations, etc.
Prevention
Since the exact cause of the appearance of piloid astrocytoma scientists can not name, there is no specific prevention of pathology. All preventive measures should be aimed at maintaining a healthy lifestyle, preventing head and back injuries, and general strengthening of the body.
The basis of prevention is:
- A varied diet of healthy natural foods, with a predominant share of vegetables, fruits, herbs, nuts, seeds and berries in the diet;
- Complete exclusion of alcoholic, tonic, carbonated, energy drinks, reducing coffee consumption to a minimum;
- Stabilization of the nervous system, avoidance of stress, conflicts, scandals, fighting phobias and neuroses;
- Sufficient rest, quality sleep at night to restore the brain's performance;
- Healthy physical activity, daily walks in the fresh air, avoiding overload - both physical and mental;
- Complete cessation of smoking and drug use;
- Minimizing harmful occupational influences (negative impact of chemicals, pesticides, excessive heat, etc.).
Forecast
Piloid astrocytoma does not have an unambiguous prognosis as it depends on many factors and circumstances. Influences include:
- Age of the patient (the earlier the disease starts, the more unfavorable the prognosis);
- The location of the tumor process;
- Susceptibility to treatment, timeliness and completeness of therapeutic measures;
- The degree of malignancy.
At I degree of malignancy the outcome of the disease can be conditionally favorable, the patient can live about five to ten years. At III-IV degrees of malignancy, life expectancy is about 1-2 years. If a less malignant piloid astrocytoma is transformed into a more aggressive tumor, then against the background of spreading metastases, the prognosis is significantly worsened.

