Medical expert of the article
New publications
Causes and pathogenesis of brain astrocytoma
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
When studying the mechanism of disease development, doctors pay special attention to the causes that can cause the pathological process. In this case, there is no general theory regarding the causes of brain astrocytoma. Scientists cannot clearly name the factors that cause rapid growth of glial cells, but do not exclude the influence of such endogenous (internal) and exogenous (external) factors that usually provoke cancer.
Cause
Risk factors for the development of tumor processes include:
- High radioactive background (the longer a person is exposed to it, the higher the risk of developing malignant tumors) [ 1 ].
- Long-term exposure of the body to chemicals, which are also believed to be capable of altering the properties and behavior of cells.
- Viral diseases. We are not talking about any virus carriage, but about the presence of oncogenic virus virions in the body. [ 2 ], [ 3 ], [ 4 ]
- Genetic predisposition. It is believed that the risk of developing cancer is higher in those whose family already has cancer patients. Geneticists have found that patients with brain astrocytoma have problems with one of their genes. In their opinion, abnormalities in the TP53 gene are one of the most likely causes of the disease. [ 5 ]
Sometimes bad habits are also included in this list: alcohol abuse, smoking, although a clear connection between them and the development of the disease is not observed.
Scientists cannot clearly say why a tumor appears and what provokes uncontrolled cell division, but they rightly believe that the tendency for a tumor to degenerate is genetically determined. Therefore, different types of tumors are found in different people, differing not only in shape and location, but also in their behavior, i.e. the ability to transform from a generally safe neoplasm into cancer.
Pathogenesis
Astrocytoma by its nature refers to tumor processes developing from brain cells. But not all cells are involved in tumor formation, only those that perform an auxiliary function. To understand what astrocytoma consists of, let's delve a little deeper into the physiology of the nervous system.
It is known that nervous tissue consists of 2 main types of cells:
- Neurons are the main cells responsible for perceiving stimuli, processing information coming from outside, generating nerve impulses and conducting them to other cells. Neurons can have different shapes and numbers of processes (axon and dendrites).
- Neuroglia are auxiliary cells. The name "glia" itself means "glue". This explains the functions of neuroglia: they form a mesh (framework) around neurons and the blood-brain barrier between the blood and neurons of the brain, provide nutrition to neurons and metabolism in the brain, and control blood flow. If it were not for neuroglia, any shock to the brain, not to mention serious injuries, would end badly for a person (death of neurons, and therefore the fading of mental functions). Glial cells soften the blow, protecting our brain no worse than the cranium.
It is worth mentioning that neuroglia are a more numerous type of brain cells (about 70-80%) compared to neurons. They can have different sizes and differ slightly in shape. Small neuroglia (microglia) perform phagocytosis, i.e. absorb dead cells (a sort of cleaning company in the nervous system). Larger neuroglia (macroglia) perform the functions of nutrition, protection and support for neurons.
Astrocytes (astroglia) are one of the varieties of macroglia glial cells. They have multiple processes in the form of rays, for which they are called radiant neuroglia. These rays form the framework for neurons, due to which the nervous tissue of the brain has a certain structure and density.
Despite the fact that neurons are responsible for transmitting nerve impulses, which is what carries out nervous activity, there is a suggestion that it is the number of astroglia that determines the characteristics of memory and even intelligence.
It would seem that the tumor is formed from intensively multiplying cells, which means that the number of astroglia increases, which should lead to an improvement in mental abilities. In fact, a local accumulation of cells in the brain does not bode well, because the tumor begins to press on the surrounding tissues and disrupt their functioning.
The human brain consists of different sections: the medulla oblongata, midbrain, and diencephalon, the cerebellum, the pons, and the telencephalon, which includes both hemispheres and the cerebral cortex. All of these structures consist of neurons and the neuroglia surrounding them, i.e. a tumor can form in any of these sections.
Astrocytes are present in both white and gray matter of brain tissue (they differ only in the length of their processes, but perform the same functions). The white matter of the brain is the pathways through which nerve impulses are transmitted from the center (CNS) to the periphery and back. The gray matter includes the central sections of the analyzers, the nuclei of the cranial nerves, and the cerebral cortex. No matter where the tumor forms, it will press on the brain from the inside, disrupting the functionality of nearby nerve fibers, disrupting the work of the nerve centers.
When we found out that brain astrocytoma is nothing more than a tumor formation, readers may have a completely understandable interest: is astrocytoma cancer or a benign tumor? We would not like to disappoint our readers, because the disease is not as rare as one might assume, but this tumor is prone to degeneration into cancer, although the degree of malignancy largely depends on its type. Some neoplasms are characterized by slow growth and are quite amenable to surgical treatment, others are characterized by rapid growth and not always a good prognosis.
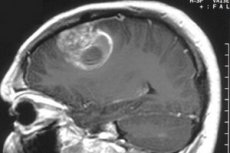
Astrocytomas may vary in shape and size, some have no clear outlines, and may grow into other brain tissues. Single and multiple cysts (cavities with semi-liquid contents) may be found inside nodular tumors (neoplasms with clear outlines and localization). The growth of such neoplasms occurs mainly due to the enlargement of cysts, which causes compression of nearby brain structures.
Nodular tumors, although they can reach large sizes, are usually not prone to degeneration. They can be classified as benign tumors that can develop into cancer purely theoretically.
Another matter is astrocytomas, prone to diffuse growth, i.e. those that capture nearby tissues, metastasize to other brain structures and neighboring tissues. They usually have a fairly high degree of malignancy (grade 3-4), and over time they acquire enormous sizes, since they are initially prone to growth, like any cancerous tumor. Such tumors tend to quickly turn from benign to malignant, so they need to be removed as early as possible, regardless of the severity of the symptoms.
Scientists already know quite a lot about glial tumors consisting of astrocytes: their types, possible localizations and consequences, behavior, ability to develop into cancer, treatment options, tendency to relapse, etc. The main question remains a mystery: astrocytes begin to behave inappropriately, which makes them multiply intensively, i.e. the mechanism of formation and development of the tumor process. The pathogenesis of brain astrocytoma remains unclear, and this is an obstacle to the development of methods for preventing the disease, the treatment of which requires neurosurgery. The molecular pathogenesis of astrocytic tumors in children is actively studied. [ 6 ], [ 7 ] And we know that brain surgery is always a risk, even with high competence of the surgeon.
Different pathways of genetic changes have been found during the progression of primary glioblastomas, characterized by gain/overexpression of EGFR and PTEN mutations, while, in contrast, secondary glioblastomas developing in younger patients exhibit frequent p53 mutations.[ 8 ],[ 9 ]
Recent studies have shown that primary glioblastomas appear to be characterized by loss of heterozygosity (LOH) 3 across chromosome 10, whereas secondary glioblastomas predominantly show LOH on chromosomes 10q, 19q, and 22q [ 10 ], [ 11 ]
Genome-wide association studies have identified inherited risk alleles in 7 genes that are associated with increased risk of glioma.[ 12 ]
Epidemiology
Brain tumors, fortunately, are far from the most common type of oncology. But this statement is more typical for the adult population. But cancer spares no one, does not look at age, gender and social status. Alas, more often than we would like to hope, it is diagnosed in young patients.
Brain and central nervous system (CNS) tumors are the most common tumors and the second leading cause of cancer death in people aged 0–19 years in the United States and Canada.[ 13 ], [ 14 ], [ 15 ]
The incidence of brain cancer in children under 15 years of age ranges from 1.7 to 4.1 per 100,000 children in different countries. The most common brain tumors were: astrocytomas (41.7%), medulloblastomas (18.1%), ependymomas (10.4%), supratentorial primary neuroectodermal tumors (PNET; 6.7%) and craniopharyngiomas (4.4%). They were located mainly in the cerebellum (27.9%) and cerebrum (21.2%). The 5-year survival rate for all brain tumors was 64%, with the worst prognosis for children with PNET. [ 16 ] Thus, childhood and adolescence can be considered as risk factors for oncology of this localization. And these statistics are not changing in the direction of decrease.
Studies have shown that brain tumors are more likely to develop in people with immunodeficiency and, conversely, diseases in which the immune system is in a state of increased activity are an obstacle to cell degeneration. Patients with certain systemic diseases are also at risk: neurofibromatosis, Tucot and Turner syndromes. The influence of such factors as high-voltage lines, mobile communications, radiation and chemotherapy for cancer of other localizations is also considered.
The biggest problem for brain oncology is the difficulty of considering the etiology of the disease, the lack of precise information about the causes of the pathology. Doctors have learned to diagnose many other types of tumors at an early stage, effective treatment regimens have been developed that can significantly prolong the life of the patient and reduce his suffering. But the brain is a complex structure to study, the study of which in humans is very difficult. Experiments on animals do not give a clear picture of what can happen in the brain of a human being.
Tumors of glial cells (astrocytes and oligodendroglial cells) are only a special variant of brain oncology. Cancer cells can also be found in other brain structures: neurons, secretory cells that produce hormones, brain membranes, and even blood vessels. But tumors of glial cells remain the most common type of brain cancer, diagnosed in 45-60% of cases of this terrible disease. At the same time, about 35-40% are astrocytoma of the brain.
Astrocytoma is classified as a primary tumor, so it is not difficult to determine the exact location of the source of cancer cells. In secondary cancer, the brain tumor is usually formed by metastases, i.e. migrating cancer cells, and its source can be located in any part of the body. But the difficulty usually lies not in determining the location of the astrocytoma, but in the fact that the tumor can behave differently.
Focal (nodular) tumors with a clear localization are more often found in children. These are mostly benign neoplasms, clearly defined on images and relatively easy to remove surgically. In childhood, astrocytomas are usually diagnosed, affecting the cerebellum, brainstem (medulla oblongata and midbrain, pons), less often the optic chiasm or optic nerve. For example, about 70% of children and only 30% of adults are admitted with a brainstem astrocytoma. Among brainstem tumors, the most common is a tumor of the pons, where the nuclei of 4 pairs of cranial nerves (facial, trochlear, trigeminal, abducens) are located. [ 17 ]
In adults, glial tumors are more often located in the nerve fibers of the cerebral hemispheres and do not have clear boundaries. Such tumors grow quite quickly, diffusely spreading to the nervous tissue, and can reach gigantic sizes. At the same time, the risk of such a tumor degenerating into a cancerous one is extremely high. Some researchers believe that astrocytoma of the brain is more often diagnosed in young and middle-aged men (60%). [ 18 ]

