Medical expert of the article
New publications
Periostotomy
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Periostotomy is a common tooth-preserving operation, the essence of which is to dissect the periosteum and partially separate it directly from the bone tissue. In most cases, this intervention is necessary to gain open access to the bone, or to cleanse it of purulent secretions. The management of periostotomy has its own peculiarities, indications and contraindications, which must be considered separately for each specific case.
Indications for the procedure
Periostotomy is performed by a dental surgeon, if the patient is found to have a localized purulent focus of phlegmonous or abscessed process, flux, necrosis of jaw tissue or periosteum.
The periosteum (periosteum) is a connective tissue outer bone sheath that provides metabolism in the surrounding tissues. The periosteum contains nerve fibers that transport nerve impulses to the brain and vessels that supply blood to the upper jaw. The underlying periosteum layer contains specific cellular structures called osteoblasts.
As the inflammatory reaction develops, the upper periosteal layer is the first to be "hit": due to the abundance of nerve endings and vessels in it, a pronounced throbbing pain appears. In the absence of treatment, inflammation spreads to the underlying layer with further involvement in the process, including bone tissue. If this happens, then bone lesions often become irreversible. Therefore, it is important to take timely action and perform periostotomy - tooth-preserving surgery, the essence of which is to dissect the periosteum, open the purulent focus, remove the purulent secretion from it, as well as, if necessary, to provide access to the jawbone.
In most cases, periostotomy is prescribed for inflammatory diseases of the periosteum and the formation of flux - an acute inflammation around the tooth root, which is accompanied by the accumulation of pus under the gum.
Additional indications for periostotomy include:
- Actinomycosis of the periosteum and jaw with the need to remove bone overgrowths;
- Serous periostitis of the jaw with the need to open the periosteum to reduce pressure on the dental tissues and prevent the development of purulent process;
- Inflammatory process after filling of dental canals;
- Purulent abscessed periostitis;
- Providing access to the root apices during intervention for upper root resection.
As part of complex measures, periostotomy is prescribed for patients with radicular cysts, jaw tumors, as well as during sinuslifting, bone grafting, prosthetics.
Preparation
The final need for periostotomy is confirmed by radiologic diagnostics. A few hours before the intervention, the patient is advised to premedicate with sedatives to optimize the effect of local anesthesia. For 24-48 hours before periostotomy it is necessary to refrain from drinking alcohol and smoking.
Using the information obtained during diagnostic measures, the doctor decides on the type of anesthesia. In addition, the following tests may be prescribed:
- CBC and urine;
- Coagulogram;
- Blood for HIV, Wasserman reaction;
- Electrocardiography.
Other preparatory recommendations:
- On the eve of periostotomy, try to rest well, avoid excessive emotional states.
- Completely refuse alcohol and smoking, do not take aspirin and other drugs without consulting your doctor.
- Have a light snack about 1-2 hours before periostotomy to avoid nausea and dizziness.
- Wear comfortable clothing that will not interfere with free movement and breathing.
- Be sure to tell your doctor if you have had any allergies to any medications.
- Be sure to tell your doctor if you show any signs of infectious disease.
It is necessary to understand: despite the fact that periostotomy is not the most pleasant procedure, modern methods and equipment allow you to carry out the intervention with maximum quality and comfort. The main point is to listen to and follow the doctor's recommendations.
Technique of the periostotomies
The first step in periostotomy is to perform anesthesia (usually local anesthesia). Upper jaw periostotomy involves injecting anesthetic twice into both maxillary halves. If a mandibular incision is to be performed, the anesthetic is injected once into the mandibular shaft area.
If the inflammation is extensive, additional anesthesia may be required in other areas, at the discretion of the physician.
Then the area of periostotomy is treated with antiseptic. The next stage is a careful dissection of soft tissues, which is performed relatively deep to obtain open access to the bone. The doctor makes every effort to maximize the quality of cleaning the formed cavity from purulent accumulations and performs the necessary manipulations in the bone area.
On average, the length of the soft tissue incision is 20 mm, sometimes more (depending on the size of the pathological focus). If periostotomy is performed in the palatine area of the oral cavity, the tissues are dissected parallel to the midline of the palate. If periostotomy is performed on the mandible, the surgeon dissects the tissue in the area where the pathological focus is better visualized.
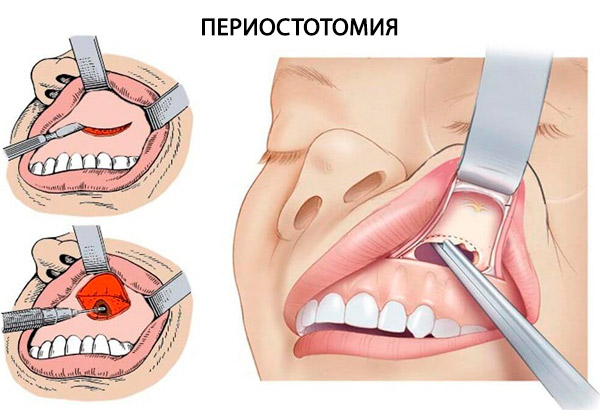
After making an incision, the doctor carefully uses special instruments to push back the periosteum and expose the bone, after which he washes the tissues with antiseptic solution.
Periostotomy of the jaws is completed with the installation of drainage - a special rubber strip that prevents adhesion of soft tissues and bone. Drainage helps minimize the likelihood of recurrence of the inflammatory process and prevents the accumulation of secretions. Drainage is removed only after the discharge from the wound has stopped.
Additionally, applications with anti-inflammatory and healing drugs of local action are applied to the wound surface. The wound edges are sutured if the incision was large.
In some cases, periostotomy of a tooth requires direct injection of medication solutions through a drain directly into the operated cavity. This procedure is often performed on patients with flux, pericoronitis, alveolitis, periodontitis, cysts or abscesses.
Periostotomy for periodontitis is only indicated when conservative treatment is ineffective. The intervention may be accompanied by the removal of a part of the tooth (for example, the root) or the complete removal of the tooth. The final decision is made by the doctor, taking into account the degree of inflammatory changes. If it is possible to perform a periostotomy, it is recommended to place a crown on the affected tooth.
Contraindications to the procedure
Periostotomy is not performed if the following contraindications are found:
- Blood diseases, leukemia, blood clotting disorders (including hemophilia);
- Oncopathologies located in the oral cavity, jaw, neck, and face;
- Concurrent radiation therapy;
- Inflammatory vascular lesions;
- Decompensated cardiovascular disease, diabetes;
- Fever, acute period of infectious diseases (contraindication is temporary, until the acute period expires and the temperature stabilizes).
All questions regarding a contraindication and the possibility of performing periostotomy are decided on an individual basis.
Consequences after the procedure
Pathologies of the periosteum are especially dangerous if the patient ignores treatment. However, even after periostotomy, the development of unpleasant consequences is not excluded, although it happens very rarely. In most cases, complications after the procedure are associated with further progression of the inflammatory reaction and the transition of the pathological process to nearby tissues, including bone tissue.
The overwhelming number of complications is due to late referral to a doctor. Sometimes the cause is incomplete opening of the purulent focus, insufficient cleansing, violations in the process of drainage.
Among the likely consequences:
- Loss of the tooth (with a repeated inflammatory process, the lesion zone expands, and pathologic changes become irreversible).
- Inflammation of bone tissue (jaw osteomyelitis).
- Gaymoritis (inflammation of the maxillary sinuses, which is characterized by a runny nose, nasal congestion, pain in the projection of the sinuses, fever).
- Blockage of the cavernous sinus (thrombosis of the cavernous sinus due to spread of infection to the sinuses of the dura mater).
- Purulent-necrotic phlegmon of the floor of the oral cavity (Ludwig's angina).
If complications occur, further treatment with medication and physiotherapy is carried out. Sometimes it is necessary to perform a repeat periostotomy.
Care after the procedure
For a more comfortable and successful recovery process, the following guidelines should be followed:
- For the first three to four hours after the periostotomy procedure, you should not eat or drink any beverages other than plain, clean, room temperature water.
- For 7-10 days after periostotomy, only pureed and chopped food in a slightly warm form may be eaten. Coarse, hot and cold food is prohibited.
- For the first 24 hours after periostotomy, it is recommended to apply cold to the cheek on the affected side (ice in a bag or towel), for 10-15 minutes.
- Carefully adhere to all doctor's appointments, take prescribed medications, perform physical therapy procedures.
- Rinse the oral cavity with antiseptic solutions, herbal infusions (infusion of chamomile, oak bark, sage, calendula, etc.).
- After each meal, you should gently rinse your mouth with a weak solution of baking soda.
- In the first time after periostotomy, it is better to limit physical activity.
- Periodic consultation with the attending physician should be made, and wound healing should be monitored.
The average period of wound healing is about 1 week. However, it can vary in one direction or another, depending on the severity of the pathology, the extent of the pathological focus, as well as the patient's compliance with medical prescriptions.
Literature
- Kulakov, A. A. Surgical stomatology and maxillofacial surgery / Edited by A. A. Kulakov, T. G. Robustova, A. I. Nerobeev - Moscow: GEOTAR-Media, 2010. - 928 с
- Dmitrieva, L. A. Therapeutic stomatology: national guide / edited by L. A. Dmitrieva, Y. M. Maksimovskiy. - 2nd ed. Moscow: GEOTAR-Media, 2021.
- Kabanova, S.L. Fundamentals of maxillofacial surgery. Purulent-inflammatory diseases:
Educational and methodical manual; in 2 vol. / S.A. Kabanova. A.K. Pogotsky. A.A. Kabanova, T.N. Chernina, A.N. Minina. Vitebsk, VSMU, 2011, vol. 2. -330с.

