Medical expert of the article
New publications
Parapsoriasis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Parapsoriasis (syn. morbus Brocq) is a clinically heterogeneous disease with an unknown pathogenesis.
Brocq first described it in 1902. He combined three dermatoses into one group that had some common features: chronicity of the course, superficial nature of the spotty-scaly rash, absence of any subjective sensations and general phenomena, resistance to therapy.
Causes parapsoriasis
The causes and pathogenesis of parapsoriasis have not been fully studied. In the development of the disease, great importance is attached to past infections ( flu, tonsillitis, etc.), the presence of foci of chronic infection (chronic tonsillitis, sinusitis, pyelonephritis, etc.), vascular changes, and immune disorders. Among the factors contributing to the development of parapsoriasis, immune disorders, allergic reactions, dysfunctions of the endocrine system, various infections, and viral diseases are noted, which play an important role in acute varioliform parapsoriasis.
Pathogenesis
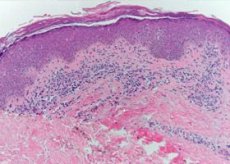
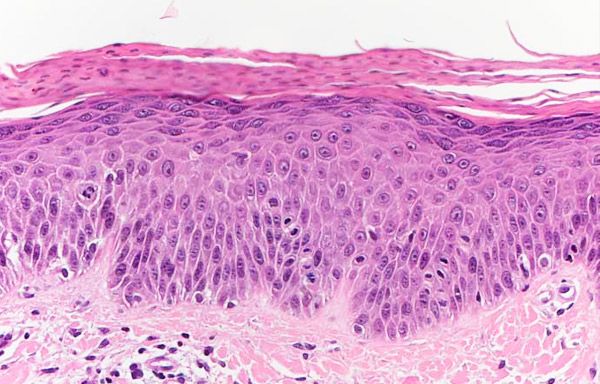
Histological examination does not reveal any specific changes. All forms of parapsoriasis have spongiosis, acanthosis, and mild parakeratosis. Characteristic features include vacuolar degeneration of basal layer cells and exocytosis. In the dermis, vessels are dilated, with an infiltrate of polymorphonuclear leukocytes, lymphocytes, and histiocytes around them. Acute parapsoriasis is characterized by hyperkeratosis, acanthosis, and vacuolar degeneration of Malpighian mesh cells with the formation of intraepidermal vesicles in some cases; in the dermis, there is a dense perivascular infiltrate with a predominance of lymphocytes; areas of tissue death with the formation of necrotic crusts.
Pathomorphology of parapsoriasis
In fresh elements of plaque parapsoriasis, papillary dermal edema, focal lymphohistiocytic infiltrates of varying intensity are observed; in the epidermis, focal parakeratosis, slight acanthosis with focal intercellular edema, and exocytosis are observed. The vessels are usually dilated, the endothelium is swollen, and lymphohistiocytic elements are detected around them.
In the large-plaque variant, the changes in the skin are more pronounced. The infiltrate is thicker, lymphohistiocytic in nature, with pronounced epidermotropism, sometimes with the formation of intraepidermal cavities filled with infiltrate cells. When studying the composition of the infiltrate in the large-plaque form of parapsoriasis using electron microscopy and cytophotometry, I.M. Raznatoisky (1982) showed that it contains many undifferentiated lymphocytes and very active histiocytes; cytophotometry yielded atypical histograms with an increase in the average DNA content above the diploid standard. S.E. Orfanos and D. Tsambaos (1982) found ultrastructural signs of Sezary cells (from 11 to 30%) in the infiltrate of large-plaque parapsoriasis, located not only in the dermal infiltrate, but also inside the epidermis, contacting with epidermal macrophages and epithelial cells. Such facts give these authors grounds to classify large-plaque parapsoriasis as a lymphoproliferative disease.
In lichenoid parapsoriasis, the skin pathohistology resembles that of other forms, but is distinguished by a denser and strip-like infiltrate consisting of lymphocytes, histiocytes, and plasma cells in the upper part of the dermis. Characteristic are the expansion and thickening of the venule walls, especially in the peripheral part of the infiltrate. The epidermis is somewhat thickened, with pronounced exocytosis with the formation of parakeratotic foci and the stratum corneum. Electron microscopic examination revealed a significant number of atypical forms of lymphocytes among the infiltrate cells, resembling Sezary cells, on the basis of which these authors classify this form, as well as the previous one, as lymphomas.
Acute lichenoid and varioliform parapsoriasis are characterized by thickening of the epidermis, focal parakeratosis, vacuolization and dystrophic changes in the cells of the spinous layer, often with the formation of intraepidermal vesicles and foci of necrosis, as well as reticular dystrophy with exocytosis of lymphoid and histiocytic elements. In the dermis - lymphohistiocytic infiltrate, both perivascular and merging. Significant changes are found in the vessels in the form of vasculitis, perivasculitis with erythrocyte diapedesis, sometimes thrombosis and necrotic changes in the vascular walls. On this basis, some authors classify this form as vasculitis.
Guttate parapsoriasis is characterized by pronounced parakeratosis and spongiosis, which may resemble seborrheic eczema or psoriasis, but differs from the latter by vacuolar dystrophy of the basal cells of the epidermis and pronounced exocytosis of the infiltrate cells. I.M. Raznatovsky (1982) found significant changes in the walls of the vessels of the superficial network and perivascular, cuff-reversible, predominantly lymphocytic infiltration in this form. However, immunological studies have not confirmed that guttate parapsoriasis is an allergic vasculitis.
Lichenoid and plaque parapsoriasis differentiates from the initial stage of mycosis fungoides. In parapsoriasis, unlike mycosis fungoides, moderately expressed proliferation of the epidermis, monomorphic lymphohistiocytic infiltrate are detected. In the dermis, there are no atypical cells in the infiltrate. Acute lichenoid varioliform parapsoriasis, due to the severity of vascular changes, should be differentiated from allergic vasculitis, from which this form differs by the absence of neutrophilic granulopites, fragments of their nuclei and fibrinoid deposits around the capillaries in the infiltrate.
Histogenesis of parapsoriasis
Immunomorphological methods have proven the immune genesis of some forms of parapsoriasis. Thus, using immunoperoxidase technique in combination with monoclonal antibodies, FM McMillan et al. (1982) found that in the infiltrate in plaque parapsoriasis there are T-lymphocytes of the T-helper and T-suppressor type with a predominance of T-helpers. In acute lichenoid and varioliform parapsoriasis, circulating immune complexes, deposits in the walls of blood vessels and in the basement membrane of the epidermis of IgM and the C3 component of the complement were found, which served as the basis for classifying this form of parapsoriasis as an immune complex disease. It was found that in the infiltrate in this form, the majority of cells are T-lymphocytes, with T-suppressors predominating. These data suggest an important role of cell-mediated immune responses in the histogenesis of this form of the disease.
Symptoms parapsoriasis
Parapsoriasis is often encountered in spring and autumn. Clinically, four forms of the disease are traditionally distinguished: guttate, plaque, lichenoid and varioliform (acute). WN Meigei (1982) classifies lymphomatoid papulosis, which is currently considered a pseudolymphoma, into the group of papular forms of parapsoriasis.

There are isolated observations of mixed parapsoriasis - guttate and plaque, guttate and lichenoid.
Plaque parapsoriasis
Depending on the size of the plaques, there is benign small-plaque parapsoriasis and large-plaque parapsoriasis prone to transformation into lymphoma. The surface of some lesions may look atrophic, wrinkled, resembling crumpled tissue paper. Telangiectasias, de- and hypopigmentation may occur, which makes the lesions similar to poikiloderma. Itching is usually absent. The appearance of itching, increased infiltration may be signs of the development of mycosis fungoides, other types of lymphomas.
The dermatosis begins with the appearance of spots or weakly infiltrated plaques of pale pink color with a yellowish-brown tint; their size varies from 3 to 5 cm, the outlines are oval, round or irregular. The lesions are usually flat, do not rise above the level of the surrounding normal skin and are located on the trunk or limbs. The elements of the rash do not tend to merge, there are small-plate or bran-like scales on their surface. Sometimes delicate wrinkles appear on the surface of the lesions, resembling crumpled tissue paper (pseudoatrophy). Subjective sensations are absent; sometimes a slight intermittent itching is observed. The dermatosis is chronic.
Guttate parapsoriasis
This type is manifested by a rash of numerous rounded nodules up to the size of a lentil, pink or light brown in color. The center of the rash is covered with brownish-gray scales. The elements of the rash are located on the skin of the trunk, upper and lower extremities, but can also appear on other areas. With this form of parapsoriasis, three phenomena are observed: the phenomenon of the wafer (when the scale is carefully removed, it separates completely), the phenomenon of hidden peeling (when scraping the surface of the rash, it is possible to cause bran-like peeling) and the symptom of purpura (when intensively scraping the rash, pinpoint hemorrhages appear). The elements disappear without a trace, sometimes leaving leukoderma spots. The disease can last for years.
Lichenoid parapsoriasis
Lichenoid parapsoriasis (syn.: lichen variegatus, parapsoriasis variegata) is an extremely rare form, the main element of the rash of which is a cone-shaped papule of round or oval outlines, reddish-yellow or reddish-brown color with a smooth, slightly shiny surface, sometimes covered with tightly seated whitish scales. The rashes are located in the form of stripes, which, crossing each other, give the lesions a reticular character. The existence of this form is not recognized by everyone. A.A. Kalamkaryan (1980) shares the opinion of S.T. Pavlov (1960) and believes that lichenoid parapsoriasis is the initial form of vascular atrophic poikiloderma Jacobi. Elements of the rash are often located on the trunk and limbs. Itching is usually absent. Lichenoid parapsoriasis is highly resistant to therapy.
Acute Mucha-Haberman parapsoriasis
Acute Mucha-Haberman parapsoriasis (syn.: acute lichenoid and lichen ossificans, parapsoriasis lichenoides et varioliformis Mucha-Haberman) differs from other forms of parapsoriasis by the polymorphism of the rashes: there are vesicular, papular, pustular, variceal, hemorrhagic rashes, necrotic crusts occupying significant areas of the skin, including the scalp, skin of the face, hands and feet. At the same time, there may be elements typical of guttate parapsoriasis. The disease begins acutely, in most cases regresses completely, leaving smallpox-like scars in place of the varioliform elements; less often, after the disappearance of acute manifestations, a picture of guttate parapsoriasis remains, which gave grounds for a number of authors to consider varioliform parapsoriasis as a variant of guttate with an acute course. At the same time, OK Shaposhnikov and N.V. Dsmenkova (1974) and other Angoras consider it a form of allergic vasculitis. Acute Mucha-Haberman parapsoriasis begins acutely and quickly becomes generalized. Some dermatologists believe that acute parapsoriasis is a variant of the drop-shaped form with an acute course. The clinical picture is characterized by polymorphism. The elements of the rash are scattered, symmetrical, and not grouped. Along with typical rashes, there are vesicular, pustular, varicella-like elements, hemorrhagic nodules, and necrotic crusts. After the rash resolves, smallpox-like atrophic scars remain. Rashes are observed on the mucous membranes of the genitals and oral cavity. Some patients experience prodromal phenomena in the form of general weakness, headache and malaise, subfebrile temperature, and enlarged peripheral lymph nodes.
Transformation of plaque and lichenoid parapsoriasis into mycosis fungoides has been noted.
What's bothering you?
What do need to examine?
How to examine?
Differential diagnosis
Guttate parapsoriasis is differentiated from psoriasis, secondary papular syphilis, lichen planus and poikiloderma of the Jacobi type; plaque parapsoriasis - with mycosis fungoides, seborrheic eczema, chronic trichophytosis of the skin; acute parapsoriasis - with chickenpox.
Who to contact?
Treatment parapsoriasis
In guttate parapsoriasis, the infection foci are sanitized. Broad-spectrum antibiotics, hyposensitizing, antihistamine, vascular (theonikol, complamin) drugs are prescribed. In chronic and subacute forms at the resolution stage, PUVA therapy is recommended. If the effect of the above treatment is not effective enough, small doses of glucocorticosteroids are prescribed.
Topical glucocorticosteroid and absorbable ointments are prescribed.
For plaque and lichenoid parapsoriasis, the same treatment measures are carried out as for guttate parapsoriasis, but treatment presents significant difficulties.


 [
[