Medical expert of the article
New publications
Ovarian hyperstimulation syndrome.
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Ovarian hyperstimulation syndrome (OHSS) is an iatrogenic complication based on the hyperergic uncontrolled response of the ovaries to the administration of gonadotropins in ovulation stimulation cycles and assisted reproductive technology programs.
The syndrome may manifest after ovulation induction with clomiphene or upon the onset of pregnancy in a spontaneous cycle.
 [ 1 ]
[ 1 ]
Epidemiology
The incidence of ovarian hyperstimulation syndrome varies from 0.5 to 14% with different ovulation stimulation schemes and does not tend to decrease. The disease has varying degrees of severity and can be fatal due to the development of thromboembolic complications or ARDS. The expected mortality rate is 1 in 450-500 thousand women. Severe forms of the syndrome, requiring hospitalization in the intensive care unit, occur in 0.2-10%. According to the Russian National Register of Assisted Reproductive Technology Methods, the incidence of severe OHSS in 2004 was 5.6%.
Causes of Ovarian Hyperstimulation Syndrome
Risk factors for developing ovarian hyperstimulation syndrome:
- age less than 35 years,
- asthenic physique,
- the presence of polycystic or multifollicular ovaries,
- maturation of more than ten follicles in the ovulation stimulation protocol,
- use of gonadotropin-releasing hormone agonist drugs and high doses of gonadotropins,
- the onset of pregnancy,
- luteal phase support with hCG preparations,
- allergic diseases.
How does ovarian hyperstimulation syndrome develop?
Ovarian hyperstimulation syndrome occurs against the background of abnormally high concentration of sex hormones in the blood plasma, negatively affecting the functions of various body systems, primarily the ovaries, and is characterized by an increase in the size of the ovaries, sometimes up to 20-25 cm in diameter, with the formation of follicular and luteal cysts in them against the background of pronounced stromal edema. The trigger for the development of the syndrome is the introduction of an ovulatory dose of chorionic gonadotropin. The development of the syndrome is based on the phenomenon of "increased vascular permeability", leading to a massive release of protein-rich fluid into the third space, the interstitium and its deposition with the development of hypovolemia, hemoconcentration, oliguria, hypoproteinemia, electrolyte imbalance, increased activity of liver enzymes, the formation of ascites, hydrothorax, hydropericardium with or without hypovolemic shock. However, the "factor X" that causes fluid transudation remains unknown. In severe cases, anasarca, acute renal failure, thromboembolic complications, and ARDS occur.
Currently, ovarian hyperstimulation syndrome is considered from the standpoint of SIRS, against the background of which massive damage to the endothelium occurs. In patients with OHSS, high concentrations of interleukins (IL-1, IL-2, IL-6, IL-8), tumor necrosis factors (TNF-a, TNF-(3)), which enhance the synthesis of prostaglandins by the ovaries, ovarian neovascularization and vascular permeability, were found in the peritoneal transudate. Under the influence of proinflammatory cytokines, systemic activation of coagulation processes occurs. The magnitude of leukocytosis correlates with the severity of SIRS. Organ-systemic damage in OHSS is similar to the damage that occurs in sepsis. The role of the microbial factor in OHSS and its contribution to the development of SIRS is currently under discussion. It is assumed that microorganisms colonizing the intestines and genitourinary tract can penetrate beyond their habitat and have an effect on the body similar to that in sepsis.
Symptoms of ovarian hyperstimulation syndrome
The severity of the syndrome is directly related to the severity of hemodynamic disorders that cause the clinical picture. The onset of the syndrome may be gradual with increasing symptoms or sudden (acute), in which a sharp redistribution of fluid in the body occurs within a few hours with accumulation in the serous cavities. When the syndrome manifests, complaints of weakness, dizziness, headache, flickering "flies" before the eyes, shortness of breath at rest and during physical exertion, dry cough that intensifies in the lying position, dry mouth, nausea, vomiting, diarrhea, bloating, a feeling of distension, tension, abdominal pain often without clear localization, rare urination, fever, swelling of the external genitalia and lower extremities arise.
In patients with ovarian hyperstimulation syndrome, respiratory failure may develop due to limited lung mobility due to ascites, ovarian enlargement, or pleural effusion. The course of severe OHSS at the manifestation stage may be complicated by acute hydrothorax, ARDS, pulmonary embolism, pulmonary embolism, atelectasis, and intra-alveolar hemorrhage. Pleural effusion is diagnosed in approximately 70% of women with moderate to severe OHSS, and the effusion may be unilateral or bilateral and occurs against the background of ascites. In OHSS, displacement and compression of the mediastinal organs due to massive right-sided pleural effusion with the development of shock have been described, as well as a fatal outcome in a woman with OHSS and hydrothorax due to atelectasis, massive hemorrhage into the alveolar lumen.
Hemodynamic disorders. In moderate and severe OHSS, arterial hypotension and tachycardia occur.
Ascites. The abdomen is distended, often tense, painful in all areas, but more often in the hypogastrium in the projection of the ovaries.
Renal and hepatic dysfunction. Urinary retention, oliguria, anuria, hepatomegaly are observed.
The course of OHSS in 80% of patients with a severe form of the syndrome is accompanied by fever. In 20% of women, fever occurs against the background of a urinary tract infection, in 3.8% - due to pneumonia, in 3.3% - an upper respiratory tract infection. Thrombophlebitis due to the installation of an intravenous catheter causes fever in 2%, inflammation of the subcutaneous fat at the site of puncture of the abdominal wall during laparocentesis - in 1% of patients. Infection of the surgical wound occurs in 1%, and post-injection abscesses (intramuscular administration of progesterone) in 0.5%. Fever of non-infectious genesis in every second patient with OHSS is probably associated with endogenous pyrogenic mechanisms. Isolated cases of sepsis in severe OHSS have been described.
Against the background of the development of the syndrome, an exacerbation of latent chronic somatic diseases occurs.
What's bothering you?
Classification
There is no single classification of ovarian hyperstimulation syndrome. Based on clinical and laboratory symptoms, four degrees of severity of the syndrome are distinguished:
- Mild OHSS. Abdominal discomfort, ovaries up to 8 cm in diameter with or without cysts, laboratory parameters are normal. Mild OHSS is called "controlled ovarian hyperstimulation", since this condition is observed in absolutely all cycles of superovulation stimulation and is currently not regarded as a pathological syndrome requiring treatment.
- Moderate OHSS. Moderate pain in all parts of the abdomen, nausea, vomiting, diarrhea, ovaries 8-12 cm in diameter with cysts, ultrasound and/or clinical signs of ascites, hematocrit does not exceed 45%, leukocytosis - 10-16x10 9 /l, hypercoagulation (D-dimer - more than 0.5 μg/ml, fibrinogen concentration - more than 400 mg/dl, APTT, INR - within normal limits).
- Severe OHSS. Hematocrit over 45%, leukocytosis 17-24x10 9 /l, hypercoagulation (D-dimer over 5 μg/ml, fibrinogen over 600 mg/dl), ovaries over 12 cm in diameter with cysts, all clinical and laboratory signs of moderate OHSS and tense ascites, hydrothorax, liver dysfunction, oliguria [diuresis less than 0.5 ml/(kg h)].
- Critical OHSS. Hematocrit over 55%, leukocytosis over 25x109/l, tense ascites, bilateral hydrothorax, hydropericardium, anasarca, enlarged ovaries up to 20-25 cm, oliguria or anuria, acute renal failure, thromboembolic complications, ARDS.
Ovarian hyperstimulation syndrome is also divided into early and late.
If OHSS occurs in the luteal phase and implantation does not occur, the syndrome suddenly and spontaneously disappears with the onset of menstruation, rarely reaching a severe form. If implantation occurs, most often a deterioration in the patient's condition is observed during the first 12 weeks of pregnancy. Late OHSS is caused by a significant increase in hCG in the blood plasma and is usually associated with implantation and early pregnancy.
Consequences and complications
Complications of ovarian hyperstimulation syndrome may proceed with the development of thromboembolic complications. The cause of thrombosis in OHSS remains unknown, but the main role in the pathogenesis of this condition is attributed to high concentrations of sex hormones, proinflammatory cytokines, hemoconcentration and a decrease in the VCP. Long periods of hospitalization, limited motor activity, decreased venous return due to an increase in the ovaries, an increase in the activity of coagulation factors, fibrinolysis inhibitors and platelets make an additional contribution to the high risk of developing thrombotic complications associated with OHSS. It has been demonstrated that in 84% of patients with thromboembolic complications that arose after ovulation induction and in assisted reproductive technology programs, their development occurred against the background of pregnancy. In 75% of cases, thrombus formation was noted in the venous bed with a predominant localization in the vessels of the upper extremities, neck and head (60%). A number of patients were diagnosed with spontaneous arterial thrombosis localized in the cerebral vessels. Less frequently, thrombi were observed in the femoral, popliteal, carotid, subclavian, iliac, ulnar, mesenteric arteries and the aorta. The literature presents an observation of the development of occlusion of the central retinal artery with loss of vision in OHSS. The incidence of pulmonary embolism in patients with OHSS and deep vein thrombosis of the lower extremities is 29%, while in women with OHSS and deep vein thrombosis of the upper extremities and arterial thrombosis, the risk of this complication is significantly lower and is 4 and 8%, respectively.
Severe cases of ovarian hyperstimulation syndrome may be accompanied by complications requiring surgical intervention - rupture of an ovarian cyst and intra-abdominal bleeding, torsion of the uterine appendages, ectopic pregnancy.
Diagnosis of ovarian hyperstimulation syndrome
The diagnosis of ovarian hyperstimulation syndrome is established on the basis of anamnesis data, a comprehensive clinical, laboratory and instrumental examination that reveals enlarged ovaries with multiple cysts, pronounced hemoconcentration and hypercoagulation in a patient who used assisted reproductive technologies or controlled ovulation induction in this cycle to achieve pregnancy.
Laboratory research
Clinical blood test
Hematocrit over 40%, hemoglobin concentration over 140 g/l, leukocytosis up to 50x10 9 /l without left shift, thrombocytosis up to 500-600x10 6 /l. Hemoconcentration (hematocrit over 55%) indicates a potential threat to life.
Biochemical blood test
Electrolyte imbalance, including hyperkalemia (more than 5.3 mmol/l) and hyponatremia (more than 135 mmol/l), leading to decreased plasma osmolarity. Hypoproteinemia (total protein more than 66 g/l), hypoalbuminemia (albumin less than 35 g/l), high C-reactive protein, increased liver transaminases up to 800 U/l, in some cases increased GGT or alkaline phosphatase, in some patients - increased creatinine concentration more than 80 μmol/l and urea more than 8.3 mmol/l.
 [ 20 ], [ 21 ], [ 22 ], [ 23 ]
[ 20 ], [ 21 ], [ 22 ], [ 23 ]
Coagulogram
Increased fibrinogen levels over 400 mg/dl, von Willebrand factor over 140%, decreased antithrombin III concentrations under 80%, D-dimer over 0.5 mcg/ml. Normal values for APTT, PTI, INR.
 [ 24 ]
[ 24 ]
Blood immunoglobulins
Decreased concentration of IgG and IgA in blood plasma. General urine analysis. Proteinuria.
Analysis of the composition of ascitic fluid
High protein content (more than 42 g/l) and albumin (more than 23 g/l), low white blood cell count, relatively high red blood cell count, high concentrations of all proinflammatory cytokines, C-reactive protein up to 135 mg/l (normal 0-8.2 mg/l), globulin fraction of proteins.
 [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ]
[ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ]
Tumor markers in blood plasma
The concentration of CA-125, reflecting massive proliferation of ovarian tissue, reaches its maximum values (up to 5125 U/ml) by the 2nd week of OHSS development, when both ovaries are most enlarged. The elevated level of the tumor marker persists for up to 15-23 weeks after the appearance of signs of ovarian hyperstimulation syndrome, despite the treatment.
Procalcitonin in the blood serum is determined in 50% of patients in the range of 0.5-2.0 ng/ml, which is regarded as a moderate systemic inflammatory reaction.
Microbiological research
When examining urine secreted from the vagina and cervical canal, atypical pathogens Pseudomonas, Proteus, Klebsiella, Enterobacter, E coli are isolated in quantities of more than 10,000 CFU/ml.
Instrumental research
Ultrasound of the pelvic organs
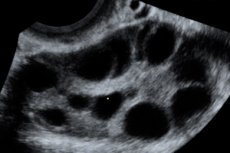
Enlarged ovaries from 6 to 25 cm in diameter with multiple cysts, the uterus is normal in size or enlarged, the presence of free fluid in the pelvic cavity and normal progressive singleton or multiple pregnancy.
Ultrasound of abdominal organs
The presence of free fluid in the abdominal cavity in an amount of 1 to 5-6 liters. Normal size and structure of the liver or hepatomegaly. Echo signs of biliary dyskinesia. When examining the kidneys, the calyceal-pelvic complex is unchanged.
Ultrasound of the pleural cavities
Presence of free fluid EchoCG. Against the background of hemodynamic disturbances, decreased EF, decreased end-diastolic volume, decreased venous return, in some cases - the presence of free fluid in the pericardial cavity.
ECG
Rhythm disturbance such as ventricular extrasystole, tachycardia, diffuse metabolic and electrolyte changes in the myocardium. Chest X-ray. Performed if ARDS and thromboembolism are suspected. A characteristic X-ray finding in ARDS is the appearance of a "ground glass" pattern and diffuse multifocal infiltrates of fairly high density (consolidation) with well-defined air bronchi, i.e. the development of extensive damage to the lung parenchyma. In pulmonary embolism, the X-ray reveals a high position of the diaphragm dome, discoid atelectasis, plethora of one of the pulmonary roots or a "cut off" root, depletion of the pulmonary pattern over the ischemic area of the lung, and a peripheral triangular shadow of inflammation.
Indications for consultation with other specialists
Due to the involvement of all organs and systems in the pathological process, an examination by a therapist is mandatory. If thrombotic complications are suspected, a consultation with a vascular surgeon is required. In the presence of pronounced hydrothorax, a consultation with a thoracic surgeon is required to decide on performing a pleural puncture.
What do need to examine?
How to examine?
What tests are needed?
Treatment of ovarian hyperstimulation syndrome
The absence of a clear concept of the pathophysiology of OHSS makes it impossible to carry out effective, pathogenetically substantiated treatment that allows effectively and promptly stopping the development of the syndrome and multiple organ disorders accompanying severe forms of ovarian hyperstimulation syndrome. Currently, there is no specific therapy for ovarian hyperstimulation syndrome, so treatment measures for these patients are reduced to pathogenetic therapy until spontaneous regression of the syndrome as the concentration of hCG in the blood plasma decreases over 7 days in cycles where pregnancy has not occurred, or 10-20 days when pregnancy has occurred. Most patients hospitalized in intensive care units are already admitted with a diagnosis of OHSS after outpatient treatment, which consists of daily assessment of weight and diuresis, limitation of excessive physical activity and sexual activity, copious drinking with the addition of solutions rich in electrolytes, and periodic blood tests. Discussion of the treatment strategy for this group of patients involves comprehensive symptomatic treatment aimed at preventing the development of PRF by restoring the CCP, eliminating hemoconcentration, electrolyte imbalance, preventing acute renal failure, ARDS and thromboembolic complications.
Stage 1 - assessment of the severity of the condition
The first step in determining the tactics of managing a patient with ovarian hyperstimulation syndrome is to assess hemodynamics and respiratory function. It is also necessary to conduct a complete physical examination with a thorough study of the condition of the limbs, head and neck area to exclude deep vein thrombosis and install a peripheral venous catheter or central vein catheterization. Subclavian vein catheterization is most appropriate, since the risk of thrombosis in this case is the lowest. Catheterization of the bladder is necessary to assess diuresis. It is necessary to examine the clinical blood test parameters, blood plasma electrolytes, protein, liver enzyme activity, creatinine, urea levels, and coagulogram parameters daily. Abdominal ultrasound is performed to determine the degree of ovarian enlargement and the presence of ascites.
Stage 2 - infusion therapy
Drug therapy of patients with OHSS should be aimed at maintaining hemodynamics and mobilizing fluid contained in the abdominal cavity by creating a negative sodium and water balance. The primary goal is to replace the volume of circulating fluid to reduce hemoconcentration and maintain sufficient renal filtration. Crystalloid and colloid solutions are used for infusion therapy of ovarian hyperstimulation syndrome.
The choice of crystalloid solution is determined by the electrolyte imbalance. When determining the amount of crystalloids administered, it is necessary to take into account that in conditions of generalized endothelial damage, the volume of these solutions should be 2-3 times less than the volume of colloid solutions, since the predominance of crystalloids aggravates the accumulation of fluid in serous cavities, and in some cases leads to the development of anasarca.
The drug of choice for restoration and maintenance of intravascular volume in patients with OHSS is hydroxyethyl starch 130/0 42 daily volume - 25-30 ml / kg. Hydroxyethyl starch 200/0 5 can also be used in the basic therapy of OHSS in a volume of 20 ml / (kg x day). However, it can accumulate in the body and with prolonged use can cause liver dysfunction and increase the level of liver transaminases, sometimes up to 800 U / l. In this contingent of patients, it is inappropriate to use hydroxyethyl starch 450/0 7 due to the high risk of allergic reactions, negative impact on kidney and liver function, deterioration of hemocoagulation parameters (prolongation of blood clotting time, risk of hemorrhagic complications). Indications for the use of dextran solutions are limited by the high frequency of allergic reactions, negative impact on the hemostasis system, release of von Willebrand factor, induction of the proinflammatory cascade, and lack of impact on the rheological properties of blood in the doses used. Infusion of dextrans under conditions of increased capillary permeability may lead to the development of the so-called dextran syndrome, accompanied by OL, impaired liver and kidney function, and the development of coagulopathy. Gelatin solutions are also not intended for infusion therapy in OHSS.
With hypoproteinemia less than 25 g/l, a 20% albumin solution is used, the daily volume is 3 ml/kg. It is recommended to use only a 20% albumin solution, since the oncotic pressure of a 20% solution is about 100 mm Hg, and the oncotic pressure of a 5% solution is about 20 mm Hg. Under conditions of high permeability of the vascular endothelium, infusion of a 5% albumin solution, in contrast to a 20% solution, leads to a more intensive exchange with the extravascular pool and a sharp increase in oncotic pressure in the interstitium, which leads to an increase in interstitial hyperhydration of the lungs.
Diuretics are justified in case of oliguria, peripheral edema, reaching hematocrit values of 36-38%. Premature or excessive prescription of diuretics can provoke aggravation of hypovolemia and hemoconcentration, increasing the risk of thrombotic complications. Furosemide is mainly used - 20-40 mg once intramuscularly or intravenously slowly for 1-2 minutes.
Principles of infusion therapy for ovarian hyperstimulation syndrome
After the initial dose of crystalloid and colloid solutions has been administered, the volume of further infusion therapy is determined taking into account the following parameters: diuresis - less than 1 ml/(kg h), hematocrit less than - 40%, mean arterial pressure - more than 70 mm Hg, central venous pressure - 8-10 mm H2O. When the specified parameters have been reached, infusion therapy is stopped. It is advisable to administer the total daily volume of infusion solutions in fractions throughout the day. Failure to comply with these approaches results in the development of hemodilution, which provokes rapid accumulation of fluid in the serous cavities and deterioration of the patient's condition. A typical mistake in the treatment of women with OHSS is the unjustified prolongation of infusion therapy when hemodynamic parameters have normalized and an attempt to completely stop the development of OHSS as an iatrogenic condition.
Stage 3 - prevention of complications
Prevention of thrombosis and thromboembolism
The basis for preventing thrombotic complications in ovarian hyperstimulation syndrome is the elimination of hemoconcentration. Antithrombotic therapy is indicated when laboratory signs of hypercoagulation appear. LMWH is used for this:
- calcium nadroparin (daily dose - 100 anti-Xa IU/kg 2 times subcutaneously),
- dalteparin sodium (100-150 anti-Xa IU/kg 2 times subcutaneously),
- enoxaparin sodium (1 ml/kg/day) 1-2 times subcutaneously).
Laboratory monitoring - determination of plasma anti-Xa activity 3 hours after LMWH administration, which allows maintaining an effective dose of the drug within the safe therapeutic range and thus minimizing the likelihood of bleeding. Antithrombotic drugs are continued until blood coagulation parameters are normalized. Monitoring is carried out by determining the concentration of D-dimer in plasma using a quantitative method. The duration of LMWH administration is determined individually, and in some cases it may exceed 30 days.
Prevention of infectious complications
Taking into account the positive effect of prescribing immunoglobulin preparations in preventing secondary infections in other diseases accompanied by protein loss, one can expect the effectiveness of this therapy in patients with OHSS. However, for the final confirmation or refutation of this hypothesis from the standpoint of evidence-based medicine, it is necessary to conduct studies. Currently, the indication for empirical antibacterial therapy is the risk of secondary infection in patients in critical condition or with unstable hemodynamics. The empirically selected drug is changed based on the results of bacteriological testing. When prescribing empirical antibacterial therapy, it is necessary to be guided by information on the severity of the disease, risk factors for infection, and the characteristics of antibiotic resistance in a given ICU.
Nutritional support
It is administered per os to all patients with severe and critical OHSS. It is necessary to follow the recommendations:
- energy value 25-35 kcal/(kgxday),
- glucose - less than 6 g/(kg x day),
- lipids - 0.5-1 g/(kg x day),
- proteins - 1.2-2 g/(kg x day),
- standard daily set of microelements and vitamins.
Stage 4 - surgical methods
Indications for laparocentesis in women with ovarian hyperstimulation syndrome:
- progressive tense ascites,
- oliguria less than 0.5 ml/dkg/min),
- an increase in creatinine concentration over 80 μmol/l or a decrease in its clearance,
- hemoconcentration with a hematocrit value of more than 40%, not amenable to drug correction.
Transabdominal or transvaginal access can be selected for laparocentesis. Enlarged ovaries create technical difficulties, which is why the use of ultrasound control is extremely important. Long-term drainage of the abdominal cavity (transabdominal laparocentesis) from 14 to 30 days with portioned removal of peritoneal transudate with apyrogenic cystoFix® catheter has a number of advantages, as it allows avoiding one-time evacuation of a large volume of peritoneal transudate and thereby eliminating sharp fluctuations in intra-abdominal pressure that cause hemodynamic disorders, stabilizing the patient's condition, and avoiding repeated punctures of the abdominal cavity to remove ascitic fluid in this category of patients. The total volume of evacuated ascitic fluid during the treatment of severe OHSS can range from 30 to 90 liters.
In patients with hydrothorax against the background of ovarian hyperstimulation syndrome, a wait-and-see approach is justified. When hydrothorax is formed, a puncture of the pleural cavity is performed only in the case of severe progressive respiratory failure.
Criteria for initiation of respiratory support in severe and critical ovarian hyperstimulation syndrome:
- lack of spontaneous breathing and pathological breathing rhythms,
- decrease in respiratory index to less than 200 mm Hg,
- life-threatening cardiac arrhythmias,
- persistent tachycardia over 120,
- severe hypotension,
- tachypnea over 40,
- involvement of accessory respiratory muscles.
In the case of ARDS development and transfer to mechanical ventilation, the following is used:
- small respiratory volumes (6 ml/kg),
- inspiratory pressure <30 cm H2O,
- PEEP (>10 cm H2O),
- The alveolar recruitment maneuver is used.
Surgical treatment for ovarian hyperstimulation syndrome is justified only in the presence of acute pathology of torsion of the appendage, rupture of the ovarian cyst, bleeding from the ovarian cyst. In case of ovarian torsion, laparoscopic untwisting of the ovary is most effective. A typical mistake in the treatment strategy for patients with uncomplicated OHSS is emergency surgery and resection of about 30-50% of the ovarian tissue or bilateral oophorectomy.

