Medical expert of the article
New publications
Osteophytes of the knee joint
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Bone overgrowths in the area of the joint surface, often in the form of spikes and sharp protrusions, are called osteophytes. Osteophytes of the knee joint provoke severe pain in the knee, almost unresponsive to the use of painkillers. The formation of osteophytes is associated with pathological changes in bone tissue. Marginal osteophytes are a frequent sign of osteoarthritis of the knee and other diarthrodial joints. These bony outgrowths are formed in the periosteum at the junction of cartilage and bone covered by synovium in diarthrodial joints. [1], [2] Treatment is long and sometimes quite complex, combined.
Epidemiology
According to the statistics of the World Health Organization, osteophytes of the knee joint are more often suffered by patients 35 years and older. Specialists explain this trend by excessive load on the knees, increased physical activity.
The prevalence of this pathology in industrialized countries is about 30-60%.
The most striking and frequent symptom of the disease, with which patients turn to doctors - acute pain when moving the knee.
In about 20-30% of people, osteophytes may be present without any symptoms. According to some reports, osteophytes are present in more than 80% of people over the age of 79, with only 13% of them being diagnosed.
Men are more prone to the onset of symptoms associated with knee osteophytes at an earlier age. However, the clinical picture is more pronounced in female patients.
The presence of osteophytes is one of the diagnostic criteria for a condition such as gonarthrosis (osteoarthritis of the knee). About 13% of women and 10% of men aged 60 years and older have symptomatic osteoarthritis of the knee. The proportion of people with symptomatic knee osteoarthritis is likely to increase due to the aging of the population and the level of obesity or overweight in the general population. [3]
Causes of the osteophytes of the knee joint
Osteophytes of the knee joint occur as a result of bone remodeling during some pathological process. Osteoarthritis and the changes associated with it lead to damage to the cartilage below which the bone is located. This adversely affects the protection of the bone tissue. As a result, the load pressure on the bone increases, pathological changes affect it. Compensatory mechanisms are triggered, bone tissue thickens, and osteophytes arise under the load.
Accelerate the course of the pathology:
- Advanced gonarthrosis;
- Older age and the changes associated with it;
- Bone hypermineralization.
However, osteophytes of the knee joint are not always due to pathological processes and can act as one of the signs of age-related changes in the bone and joint apparatus.
In the formation and progression of the disease are involved factors, both general and specific impact. Thus, knee joints are most often affected under the influence of excess weight, synovitis, subchondral lesions of the tibia.
Risk factors
Regular loads on the knee joint gradually lead to the start of degenerative processes, wear and tear of the cartilage tissue of the joint. If at the same time there are such factors as age over 30 years, joint injuries, foot pathologies (deformities, etc.), wearing uncomfortable shoes, the negative impact on the bone structures of the knee increases many times over.
In the process of wear and tear of the articular tissues, the load directly on the knee joint and the ligamentous apparatus increases, which entails thickening of the ligaments, increased friction and, as a result, the growth of osteophytes.
Degenerative changes begin at a relatively young age. In most cases, it is a slowly developing pathology that hardly makes itself known until the growths begin to affect the nerve structures.
Factors that can accelerate degenerative processes may be as follows:
- Congenital features of the musculoskeletal system;
- Nutritional features;
- Lifestyle, bad habits;
- Traumatic injuries, including sports overloads, traffic accidents, etc.
Among the most frequent factors in the appearance of osteophytes of the knee joint is osteoarthritis, often contributing to the pathology in patients over 55 years of age.
Pathogenesis
The formation of marginal osteophytes begins with dysregulation of chondrogenesis involving differentiation of chondrogenic cells located in the periosteum, resulting in the formation of a cartilage-like structure called a chondrophyte. The chondrophyte then undergoes ossification to form a chondroosteophyte, and the entire structure eventually turns into bone to form an osteophyte. [4], [5] Pathologic bone growths appear against the background of ossification processes of the periosteum layer, ligamentous apparatus and other tissues adjacent to the knee joint. In the normal state of the skeletal system, osteophytes do not grow.
The problem mainly affects large joints, such as elbows, shoulders, ankles, knees, and hips. Vertebrae, rib joints and clavicles may also be affected.
According to pathogenetic directions, osteophytes are categorized into the following types:
- Post-traumatic - formed after traumatic injury with periosteum detachment or bone fractures. The process is particularly activated when infectious agents enter the tissues - in particular, this occurs in open fractures.
- Degenerative-dystrophic - develops against the background of intensive destruction of the articular cartilage with damage to the subcartilaginous bone. An example is deforming arthrosis of the knee with limited range of motion.
- Post-inflammatory - arise due to inflammatory reactions, including against the background of tuberculosis, osteomyelitis, rheumatoid arthritis, brucellosis and so on.
- Systemic, endocrine - associated with certain skeletal changes, endocrine disorders. An example is the formation of osteophytes in patients with acromegaly.
- Osteophytes due to central nervous system lesions - arise when the nerve innervation of the articular tissues is disturbed.
- Postload - formed due to physical overload in the area of exposure of the periosteum to the contractions of the attached musculature.
- Osteophytes that form due to microdamage of the joint capsule or its impingement between the joint surfaces during periods of sudden movement activity.
Although marginal osteophytes have been identified as a sensitive and early sign of the presence of cartilage lesions in patients with osteoarthritis, the exact pathogenesis of osteophytes is only beginning to be understood. The cytomorphologic findings and gene expression patterns during osteophyte formation resemble those of fracture marrow healing and endochondral growth plate ossification. [6] It has recently been shown that osteophyte formation and the presence of cartilage lesions are physically independent phenomena. [7] Previously published studies have shown that osteophyte growth is due to the release of cytokines from damaged cartilage rather than mechanical actions on the joint capsule, that synovial tissue plays an important role in the regulation of osteophyte formation, and that exogenously administered cytokines can induce or inhibit osteophyte formation. [8], [9], [10]
Two cytokines that play a central role in the initiation of chondrogenesis, the first step in osteophyte formation, are transforming growth factor beta (TGF-β) and bone morphogenetic protein-2 (BMP-2). TGF-β and BMP-2 are present in high concentrations in osteophytes obtained from patients with osteoarthritis of the knee and hip, [11], [12] as well as in the synovial fluid of animals after acute cartilage injury. [13] TGF-β and BMP-2 have also been shown to induce chondrogenesis in vivo by direct injection into the knee joint of animals and in vitro by exogenous injection into mesenchymal cells in culture, whereas inhibitors of these cytokines have been found to prevent chondrogenesis. [14], [15]
Symptoms of the osteophytes of the knee joint
The first signs of osteophytes are regular pain and joint crunching. It is noteworthy that the severity of the disease on the radiograph does not always correspond to the intensity of the symptomatology. There are cases when the knee joint had significant destruction, nevertheless, clinical manifestations were practically absent. There are also opposite situations, when pathological changes on the radiograph are small, and the symptomatology is vivid and multifaceted.
The size of the osteophytes themselves is more important than the size of the articular gap.
In patients suffering from osteoarthritis of the knee joint:
- Bone growths significantly increase the risk of chronic pain syndrome;
- Both the size and the number of osteophytes influence the strength of pain manifestations;
- The presence of osteophytes increases the risk of ligamentous damage.
Other possible symptoms:
- Dull pain radiating to the heel, thigh;
- Numbness or tingling in the affected leg;
- Progressive weakness in the limb;
- Gait changes, limping.
Symptomatology increases with physical activity and decreases after a period of calm.
Due to the fact that the clinical picture in osteophytes of the knee joint is similar to that in some other joint diseases, it is necessary to fully examine patients to clarify the diagnosis.
Conditionally specific signs of pathologic growths in the knee joint can be considered:
- So-called "starting" pain, which appears at the moment of starting to walk or descend stairs, with localization on the anterointernal surface of the knee (sometimes "goes" to the lower leg or thigh);
- Increased pain at the moment of flexion of the joint;
- Sometimes - weakening and atrophic changes of the quadriceps muscle, painful sensations on probing in the projection area of the joint gap or periarticular zones.
Many patients have an outward curvature of the knee as well as joint instability.
Stages
The main four stages of osteophytes of the knee joint are distinguished:
- The first stage is characterized by discomfort and slight pain in the knee associated with little physical activity.
- The second stage is characterized by a longer and more intense pain, which disappears only after a long period of rest. Some active movements may be restricted, and pain on probing the knee is almost constant.
- The third stage is characterized by a significant increase in pain intensity. Stiffness of movements in the morning appears.
- The fourth stage is accompanied by constant pain in the knee with a pronounced increase with load. The periarticular muscles atrophy, motor activity is limited.
Forms
Osteophytes significantly increase the risk of chronic pain syndrome in the knee joint. If the growths are large or pointed, they can damage the ligaments, menisci. However, the prognosis and intensity of clinical manifestations largely depends on the type of bone formation.
Edge osteophytes of the knee joint occur at the edges of bone segments. Such growths are most often caused by age-related degenerative changes, intensive and frequent loads on the knee area, excessive body weight, and sedentary lifestyle.
Large growths pose a direct threat to the mobility of the affected limb. At the same time, small osteophytes of the knee joint may become an incidental finding during radiologic or tomographic examination and may not show any symptoms.
Complications and consequences
Osteophytes of the knee joint can cause complications, which primarily depends on the size of the growths, their number, location and stage of development. Complications can be moderate and severe, affecting the general health of the patient.
Among the most common adverse effects are:
- Compression of nerve endings, resulting in severe pain, weakness, forced position and restricted mobility of the affected limb;
- Complete immobilization of the knee;
- Degenerative processes, muscle atrophy;
- Limb deformity.
Over time, a person with osteophytes of the knee joint loses the ability to maintain physical activity for long periods of time. At first, there are difficulties in walking long distances, then - short distances. Then it becomes necessary to use various support devices (sticks, crutches, etc.).
The course of the pathology becomes especially severe at advanced stages of development, when there is a curvature of the articulation, violation of its function. The length of the limb changes, there are problems with walking. Progressive narrowing of the articular gap leads to knee block. At the same time, arthritis, reactive synovitis, etc. Develop. In the most unfavorable development of events is formed ankylosis - a complete loss of mobility due to the fusion of the articular surfaces with the growth of inelastic fibrous tissue. Blood circulation is disturbed, the supply of nutrition and oxygen to the tissue suffers, which only worsens the situation.
As joint function deteriorates, the load on the entire musculoskeletal system is unevenly distributed. Overloaded segments also undergo pathological changes, further aggravating the patient's condition. Deformities of the feet and spinal column, pelvic misalignment, etc. May develop.
Further, in the absence of treatment, bursitis, myositis, osteonecrosis, etc. Occur. Almost all structures of the musculoskeletal system suffer, and the person becomes disabled.
Diagnostics of the osteophytes of the knee joint
There are no laboratory values that are unique to knee osteophytes. However, tests are still prescribed, in particular:
- In the differential diagnosis (the absence of inflammatory changes in the general blood test, absence of antibodies to cyclic citrullinated peptide, normal uric acid content in the blood should be noted);
- To determine likely contraindications to a particular treatment method (clinical blood and urine tests, blood chemistry);
- To exclude an inflammatory reaction (evaluation of erythrocyte sedimentation rate and C-reactive protein).
Synovial fluid analysis is performed in cases of synovitis, suspected arthritis. In general, in non-inflammatory osteophytes, synovial fluid is clear, sterile, moderately viscous.
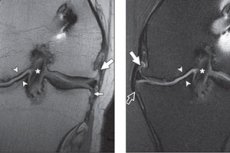
Instrumental diagnostics in this situation is more indicative. In this case, the most accessible and informative method is considered to be X-ray, which allows detecting the narrowing of the joint gap, the direct presence of osteophytes and subchondral sclerosis.
The width of the joint gap is measured in the narrowest area. The norm for the knee joint is from 6 to 8 mm. Depending on the degree of narrowing and the extent of osteophytes, the doctor determines the radiologic stage of the pathological process:
- Questionable radiologic manifestations (no or little narrowing, osteophytes appear as small shallow acuminations).
- The manifestations are minimal (narrowing is small, osteophytes are single in the area of articular margins).
- Manifestations are moderate (moderate narrowing, outgrowths are not isolated small, there are signs of subchondral osteosclerosis and slight curvature of the articular surfaces).
- The manifestations are intense (narrowing is pronounced, outgrowths are multiple and large, there are signs of subchondral osteosclerosis and distortion of bony epiphyses).
Radiography of the knee joints is performed according to the standard technique, using straight/posterior projection and passive flexion (both knees must be in contact with the cassette and in the same plane as the hip joints, patella and the ends of the big toes). One radiologic examination is usually sufficient. Repeated X-rays are necessary if the doctor suspects the attachment of another disease, if a surgical operation in the joint area is planned.
Other possible instrumental studies include:
- MRI;
- CT scan;
- Ultrasound;
- Radiologic densitometry.
If synovitis of the knee joint is detected, a joint puncture is performed with the withdrawal of synovial liquor with further analysis to determine the presence of inflammatory crystalline processes.
Arthroscopy is more sensitive than MRI for detecting superficial cartilage lesions. [16], [17] However, there are significant areas in the posterior femoral condyles that are hidden from arthroscopy and therefore better evaluated with MRI. [18]
The false-positive rate for marginal osteophytes detected on radiographs reaches 53% for patellofemoral, 44% for medial and 33% for lateral, with arthroscopy used as the reference standard [19] and reaches 41% for patellofemoral and 17% in tibial-femoral, with MRI used as the reference standard. [20], [21]
Differential diagnosis
Usually, osteophytes of the knee joint are diagnosed without much difficulty during radiologic examination.
As part of the differential diagnosis, such criteria as the detection of limited motor capabilities, pain during passive extension and flexion of the knee, as well as the nature of radiologic changes are used:
- Narrowing of the joint gap;
- Peculiarities of the shape and location of osteophytes;
- Presence of subchondral sclerosis, cysts, etc.
Not only osteophytic growths may be present in the knee joint, but also enthesophytic protrusions, which are very similar to each other. Enthesophytes are isolated zones of ossification that are located in the area of attachment of the ligamentous apparatus, tendons and joint capsule to the bone tissue. In the knee joint, enthesophytes are more often found in the area of the patella - in the area of attachment of the patellar ligament and the tendon of the 4-coronary thigh muscle. Both osteophytes and enthesophytes can cause quite intense pain syndrome.
In general, the differential diagnosis is made with other known joint diseases.
Who to contact?
Treatment of the osteophytes of the knee joint
How to get rid of osteophytes in the knee joint? Treatment measures are always combined, using pharmacological and non-pharmacological methods. Completely eliminate the growths in this way will not be possible, but treatment successfully contributes to the elimination of pain syndrome, improvement of joint function, prevention of further progression of the disease.
Patients are prescribed therapeutic physical therapy: especially recommended are water exercises, aerobic exercise, which successfully reduce the intensity of pain in the knee joint.
For knee relief at pronounced stages of the pathological process, it is necessary to use a supportive cane in the hand opposite the affected knee. In advanced cases, it is recommended to walk with crutches or walkers.
In case of disturbed joint biomechanics prescribe the wearing of supinators, insoles, knee braces, orthoses, which unload the articulation.
An important role is played by physiotherapy, which is actively used, especially in the early stages of pathology. In addition, medications are also used. First of all, we are talking about prolonged means of basic therapy, which include chondroitin sulfate, glucosamine g / h or sulfate, their combinations, as well as diacerein, Rumalon, avocado or soy preparations, alflutop, chondrogard. These drugs have an accumulative effect, anesthetize, stop the development of inflammation, and in general - slow the progression of osteophytes and osteoarthritis. Take these drugs for a long time, annually for at least six months. The effect appears after about 1.5-3 months, and after discontinuation of the course of reception is maintained for 1-2 months. Another advantage of such medications is the reduction in their use of nonsteroidal anti-inflammatory drugs, which significantly reduces the likelihood of adverse side effects.
In order to enhance the bioavailability of the drug substance, such prolonged preparations may be administered by injection (intramuscularly). An example is Hondrogard, a drug for intramuscular or intra-articular administration. The active component is chondroitin s/n in an amount of 100 mg/mL. Hondrogard is effective and safe, and intra-articular and intramuscular injections can be alternated, which contributes to persistent pain relief.
With mild pain and the presence of contraindications to the use of nonsteroidal anti-inflammatory drugs successfully used Paracetamol in an amount not exceeding 3 g per day. If there are no negative reactions of the body, the drug is prescribed for a long period of time. If such treatment is ineffective, side effects appear, pain increases, inflammatory processes develop, non-steroidal anti-inflammatory drugs are prescribed.
It is important to take into account that these drugs, if taken for a long time, can cause a number of undesirable side effects - in particular, from the digestive system, cardiovascular system, liver, kidneys. Therefore, drug selection and dosage adjustment is carried out individually.
For osteophytes of the knee joints, the following type of local treatment is most relevant:
- The first stage - application of Diclofenac ointment (gel) for up to 1-1.5 months;
- Second stage - Ketoprofen ointment for 1.5-3 months;
- Third stage - again Diclofenac for 1.5-3 months.
The topical form of non-steroidal anti-inflammatory drugs rarely causes adverse events from the digestive system, kidneys and cardiovascular system, so it is safer than the oral form, although it may cause dermatological side effects. It is recommended to use up to 10 cm of topical agent on the knee joint area at a time. [22]
If the problem persists, the feeling does not improve, intra-articular therapy is used - a kind of treatment of osteophytes of the knee joint without surgery. Corticosteroids are injected into the affected inflamed joint, not more than 1-2 times a year in one joint. Triamcinolone (20 to 40 mg), Methylprednisolone (20 to 40 mg), Betamethasone (2 to 4 mg) are used. If the inflammatory process in the joint is absent, hyaluronic acid preparations are administered. Their effect is also cumulative, but it persists for six months to a year.
If this treatment is ineffective, the therapy is replaced by the use of opioid analgesics or antidepressants. Tramadol is used for a short period of time for severe pain. Initially, 50 mg per day is prescribed, then the dose is increased if necessary (up to 200-300 mg per day).
Of the antidepressants, Duloxetine is the most suitable, as it successfully relieves pain, eliminates stiffness, and somewhat improves the quality of life of patients with knee osteophytes.
If the above therapy also proves ineffective, surgery is considered.
Physiotherapy treatment
All patients with osteophytes of the knee joint (if there are no contraindications) are shown physiotherapy:
- Cryotherapy (especially if there are signs of an inflammatory reaction);
- Heat treatment;
- Percutaneous electroneurostimulation;
- Ultrasound therapy;
- Laser therapy;
- Acupuncture, massage, therapeutic baths (mud treatment, radon, sulfide baths).
Herbal treatment
Phytotherapy is actively used in osteophytes against the background of general conservative treatment. It should be borne in mind that it is impossible to completely replace pharmacotherapy with herbal treatment. In addition, even medicinal plants have their contraindications to use, so the use of certain preparations should be coordinated with your doctor.
We recommend paying attention to the following folk medicine recipes:
- Decoction on the basis of birch buds. One tablespoon of dried birch buds pour 1 liter of boiling water and put on low heat for 30 minutes. Then remove the decoction from the fire, cover with a lid and kept until it cools down. The remedy is taken 200 ml three times a day.
- Coniferous baths. Green pine buds from young pine trees are boiled with boiling water, boiled over low heat for half an hour, insist until cool, filter and add the decoction to the bath (about 2-3 liters per bath).
- Chamomile baths. 100 g of dried chamomile flowers and leaves insist for 60 minutes in 2 liters of boiling water. The infusion is added to the bath.
- Chestnut tincture. Dried fruits of horse chestnut crushed, 20 g of crushed raw materials poured 0.4 liters of alcohol. Infused for a week, filtered. Use for rubbing and compresses on the affected knee joint.
- Compress of black radish. The root vegetable is peeled, rubbed on a coarse grater, laid on gauze and applied to the affected knee in the form of a compress. Wrapped. Withstand for several hours (effectively used at night).
- Elderberry decoction. Pour 30 g elderberries 200 ml of water, bring to a boil and remove from the fire. Kept under a lid until cooled, filtered. Divide the resulting remedy into three parts, drink three times a day.
As mentioned above, for successful treatment, herbal remedies are used in combination with medications and physical therapy prescribed by the attending physician. Only in this case, it is possible to achieve a steady improvement in health. It should also be noted that it will take some time to obtain such an effect. Therefore, you need to be patient and clearly follow the recommendations of doctors.
Surgical treatment
Technical removal of osteophytes of the knee joint is possible with the so-called arthroscopic debridement. The surgeon makes a couple of punctures in the area of the affected articulation, introduces thin catheters equipped with a camera, illumination, instrumentation. Using the necessary tool, the specialist "grinds" the surface of the joint.
It should be realized that such surgery is not always indicated, and its results are often short-lived. Debridement is practiced:
- In stage 1 or 2 osteoarthritis (no more);
- With preserved knee function;
- When the lower limb axis is normal or deviated by less than 5´;
- In the absence of indications for endoprosthesis or corrective osteotomy.
In advanced cases, when there is a threat of disability, arthroplasty and endoprosthesis are performed.
In the course of endoprosthetics, the surgeon recreates the damaged segments of the joint using artificial elements - implants. As a result, the limb axis is restored and the range of motion is improved.
Prevention
The risk of knee osteophyte formation is greatly reduced by factors such as:
- Moderation of physical activity, avoidance of excessive joint loading;
- Adequate organization of workplaces, regular exercise, walking, swimming;
- Timely referral to doctors for infectious and other diseases;
- Weight control;
- Avoiding trauma to the lower extremities.
If any suspicious signs of osteophytes are detected, treatment should begin the sooner the better. It is important to seek medical attention immediately, undergo an examination and all necessary treatment program.
It should not be forgotten that the most beneficial nutrition for joint health is a balanced diet. The musculoskeletal apparatus must receive sufficient amounts of all the necessary substances. Moreover, dishes should be properly cooked, without prolonged heat treatment and frying. It is recommended to use fresh vegetable products, steamed or baked dishes, stewed with the addition of a small amount of liquid.
Another of the main principles of preventing the formation of osteophytes is the observance of a drinking regimen. An adult should drink about one and a half liters of clean drinking water daily, except for tea, coffee and other drinks. Drink water in the morning after waking up, half an hour before meals, and before physical activity.
Food "enemies" of joints: coffee and strong tea, sorrel and spinach, animal fats and offal, sweets and alcohol, artificial additives (stabilizers, flavor enhancers, etc.), trans fats and refined foods.
Forecast
Numerous clinical studies have shown that marginal osteophytes detected on radiography are the most sensitive but least specific sign for predicting the presence of cartilage lesions in the same region of the knee joint. [23]
Outgrowths in the knee joint in the absence of treatment can cause a number of complications, which depends on the speed and degree of formation of pathological changes, on the characteristics of the location of osteophytes. Such complications can be both moderate and pronounced, affecting various functions and conditions.
Most often, lack of treatment leads to gradual limitation of joint function up to immobilization of the knee, to the appearance of severe pain as a result of compression of nerve endings, to the restriction of movement (mobility).
In general, the prognosis for patients is not always unambiguous and the same. It largely depends on the timeliness and competence of treatment measures, on the individual characteristics of the body. About the relative favorability of the prognosis can be said if a person seeks medical help in the early stages of pathology, follows all the recommendations of doctors, including adjusting lifestyle and nutrition. Otherwise, osteophytes of the knee joint progress, the patient's condition gradually deteriorates, up to disability. The main step to preserving the health of the musculoskeletal system is regular medical examinations, which allow to identify probable disorders in the early stages of development.
Knee osteophytes and the army
Osteophytes are usually secondary and are a consequence of some other pathological process in the body - in particular, osteoarthritis. If the diagnosis reveals degenerative changes in the joint structures, then doctors prescribe appropriate therapeutic measures. Depending on the degree of destruction and tissue changes, the intensity of the clinical picture and the impact of the pathology on the general condition of a particular patient, the medical commission decides on the possibility or impossibility of his service in the army.
Recognizing a person as unfit for service is possible:
- If osteophytes of the knee joint are multiple, accompanied by severe pain syndrome without response to treatment;
- If there is severe limitation of movement, joint swelling, joint curvature, requiring the wearing of special devices and shoes.
If pathological changes persist for a long time, and treatment does not bring a positive result, the conscript can receive an exemption for health reasons.
In order for the representatives of the military commission to make the appropriate decision, the conscript must provide all necessary medical documentation, including diagnostic results (X-rays, MRI), transcripts, observation sheets, statements, etc., as well as documents confirming the regular treatment of the conscript in hospitals.
Most often with osteophytes of the knee joint, service in the army becomes impossible:
- If there is a significant destruction of cartilage, maximum narrowing of the joint gap with limitation of joint functionality;
- If progressive deforming osteoarthritis of other joints is detected.
In the absence of symptoms and normal function of the affected knee, the conscript is assigned the status of "fit for military service".
If during the period of passing the medical commission the conscript is found to have an acute stage of inflammatory disease, he is prescribed appropriate treatment and given a temporary deferment, including the subsequent stage of rehabilitation.

