Medical expert of the article
New publications
Osteodystrophy
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Osteodystrophy is a general term that describes a variety of disorders and changes in bone structure and function. These changes can be caused by a variety of medical conditions and diseases. Osteodystrophy can include the following:
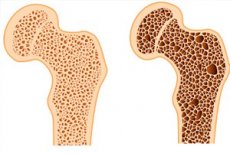
- Osteoporosis: This is a condition in which bones become less dense and more brittle due to loss of mineral density. This increases the risk of fractures.
- Osteomalacia: This is a condition in which bones become soft and deformed due to a lack of minerals such as calcium and phosphate.
- Osteitis: Inflammation of the bones that may be associated with infection or other diseases.
- Osteodystrophy of renal origin: This is a change in bone structure and function that can develop in people with chronic renal failure due to the inability of the kidneys to efficiently process calcium and phosphate.
- Osteodystrophy associated with neuromuscular or genetic conditions: Some neuromuscular or genetic conditions can cause changes in the bones, such as osteoporosis or bone deformities.
- Rickets: It is a childhood condition that is associated with deficiency of vitamin D, calcium and phosphorus and leads to bone deformities.
- Other medical conditions: Some diseases such as cancer, hyperparathyroidism (increased secretion of parathormone), and certain medical procedures such as surgical removal of the stomach or long-term treatment with glucocorticosteroids can also cause osteodystrophy.
Treatment of osteodystrophy depends on its cause and the specific changes in the bones. Doctors may prescribe treatments that address the underlying medical condition, correct nutrient deficiencies, as well as physical rehabilitation and medications to strengthen bones and reduce the risk of fractures. It is important to see a physician for an accurate diagnosis and to develop an appropriate treatment plan.
Causes of the osteodystrophies
The causes of osteodystrophy can be varied and depend on the specific type of osteodystrophy. Here are some of the main causes that can cause different forms of osteodystrophy:
- Paradoxical hyperparathyroidism: This is a condition in which parat hormone, the hormone that regulates calcium levels in the blood, becomes overactive. This can lead to bone demineralization and the development of osteoporosis.
- Chronic renal failure: Patients with chronic renal failure may have impaired calcium and phosphorus metabolism in the body, which in turn leads to bone demineralization.
- Osteomalacia: This is a bone mineralization disorder that can be caused by a deficiency of vitamin D, which is necessary for normal bone formation.
- Hypercalcemia: Elevated blood calcium levels can lead to calcium deposition in bones and other tissues, which can affect bone health.
- Hypophosphatemic disorders: Certain genetic disorders can cause a lack of phosphate in the blood, leading to impaired bone mineralization.
- Endocrine disorders: Some endocrinedisorders such as hypoparathyroidism, hyperthyroidism and others can affect bone metabolism.
- Medications: Some medications, including glucocorticoids and antiepileptic drugs, can negatively affect bone health.
- Genetic factors: Some forms of osteodystrophy can be inherited genetically.
Symptoms of the osteodystrophies
The symptoms of osteodystrophy can vary depending on the specific type of osteodystrophy and the cause that causes the condition. However, common symptoms of osteodystrophy may include the following:
- Bone pain: Patients with osteodystrophy may experience pain in different parts of the body, especially in the bone area.
- Bone fragility: A decrease in bone mineral density can make bones more brittle and increase the risk of fractures.
- Bone deformities: In some cases, osteodystrophy can lead to bone deformities, especially in children.
- Weakness and reduced physical activity: Bone pain and weakness can limit movement and physical activity.
- Impaired growth and development in children: Children with osteodystrophy may have delayed growth and development due to deformities and limitations in movement.
- Symptoms associated with the underlying medical condition: If osteodystrophy is the result of another medical condition, there may be other symptoms associated with that condition.
- Racitis: If osteodystrophy is associated with vitamin D deficiency, symptoms may include bone pain, deformities, and increased risk of fractures.
- Symptoms of other comorbidities: If osteodystrophy is associated with other medical conditions, such as hyperparathyroidism or chronic renal failure, symptoms characteristic of these conditions may also occur.
Diagnostics of the osteodystrophies
Diagnosis of osteodystrophy usually involves the following steps:
- Gathering medical and medical history: The physician begins to gather information about the patient's medical history, including symptoms, how long they have been present, risk factors (such as having chronic conditions or taking certain medications), and family history of illness.
- Physical Exam: Your doctor may perform a physical exam to look for signs associated with osteodystrophy, such as bone soreness, skeletal deformities, decreased joint mobility, and other changes.
- Laboratory tests: A variety of laboratory tests may be needed to diagnose osteodystrophy, including:
- Blood tests: Measuring levels of calcium, phosphorus, magnesium, alcal phosphatase, parathormone (PTH), vitamin D, and other markers of bone metabolism.
- Markers of bone metabolism: Determination of the level of markers such as CTX (carboxytelectin), NTX (non-telopeptide bone tissue) and others that may indicate the activity of bone metabolism processes.
- Instrumental tests: These may include x-rays, computed tomography (CT) scans, or magnetic resonance imaging (MRI) of the skeleton to detect changes in bones, joints, and other tissues.
- Densitometry (DXA): This is a special x-ray test to measure bone density and determine if you have osteoporosis or osteopenia.
- Bone biopsy: In some cases, it may be necessary to take a sample of bone tissue for detailed analysis and a definitive diagnosis.
Who to contact?
Treatment of the osteodystrophies
Treatment of osteodystrophy depends on its cause and the characteristics of the disease. Osteodystrophy is a generic name for various conditions characterized by abnormalities in mineral metabolism and decreased bone density. It can be associated with different medical conditions such as osteoporosis, osteomalacia, or rickets.
Treatment may include the following:
- Correction of the underlying medical condition: If osteodystrophy is caused by other conditions such as hyperparathyroidism (elevated levels of parathormone), vitamin D or calcium deficiency, the underlying condition must be treated. In this case, your doctor may prescribe appropriate medications and diet.
- Calcium and vitamin D supply: Calcium and vitamin D supplements are often recommended for patients with osteodystrophy to strengthen their bones. The dosage and form of the preparations may vary depending on individual needs.
- Bone-strengthening medications: In some cases, your doctor may prescribe bisphosphonates, a series of medications that help increase bone density. Recombinant parathormone therapy may be another option.
- Physical activity: Regular physical activity, especially moderate bone-strengthening activities such as walking and lifting weights, can help strengthen bones and improve bone density.
- Diet: It is important to consider diet and intake of calcium, vitamin D, and other important nutrients. Talk to your doctor or dietitian about proper nutrition.
- Avoiding risk factors: Avoid risk factors that can worsen bone health, such as lack of physical activity, smoking and excessive alcohol consumption.
- Regular medical check-ups: Regular consultations with your doctor will help monitor your bone health and the effectiveness of treatment.
Forecast
The prognosis of osteodystrophy depends on its specific form, cause and severity, as well as the success of treatment and management of the underlying problem. It is important to note that osteodystrophy can take many forms and have a varied course, so the prognosis can vary considerably.
The following are some common points that may affect the prognosis of osteodystrophy:
- Cause of osteodystrophy: If osteodystrophy is caused by a reversible factor such as vitamin D deficiency or calcium deficiency, the prognosis can be good with proper treatment and correction of the deficiency.
- Chronicity: Some forms of osteodystrophy, such as osteoporosis, can be chronic and progressive. The prognosis in such cases depends on the effectiveness of measures to prevent bone loss and treat osteoporosis.
- Age: The age of the patient can affect the prognosis, as bone mass usually decreases with age. In young adults and children, osteodystrophy may have a more favorable prognosis.
- Associated conditions: Prognosis may be worse if osteodystrophy is accompanied by other serious diseases or complications.
- Treatment and management: Proper treatment and management of the condition can improve prognosis. This may include the use of medications, lifestyle changes, physical activity and diet.
- Genetic factors: In hereditary forms of osteodystrophy, prognosis may depend on specific genetic mutations and family history.
List of authoritative books and studies related to the study of osteodystrophy
- "Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism" - by Clifford J. Rosen, Juliet E. Compston, et al. (Year: 2021)
- "Osteoporosis and Osteoarthritis" - by Kathleen A. Culhane-Pera (Year: 2007)
- "Renal Osteodystrophy" - by Juliet E. Compston, et al. (Year: 2009)
- "Osteoporosis: Diagnosis, Prevention, Therapy" - by Pierre D. Delmas (Year: 2013)
- "Bone Diseases: Macroscopic, Histological, and Radiological Diagnosis of Structural Changes in the Skeleton" - by Claus Peter Adler (Year: 2021)
- "Metabolic Bone Disease and Clinically Related Disorders" - by Louis V. Avioli (Year: 2013)
- "Renal Bone Disease: Molecular, Translational and Clinical Perspectives" - by Beate Lanske, Marc K. Drezner (Year: 2020)
- "Osteoporosis: Pathophysiology and Clinical Management" - by Eric S. Orwoll, Michael Bliziotes (Year: 2003)
- "Handbook of Pediatric Bone and Mineral Metabolism" - by Jürgen W. Spranger, Ekkehard H. Pralle (Year: 2012)
- "Metabolic Bone Disease: Volume II" - by Louis V. Avioli (Year: 1993)
Literature
Kotelnikov, G. P. Traumatology / edited by Kotelnikov G. P.., Mironov S. P. - Moscow: GEOTAR-Media, 2018.

