Medical expert of the article
New publications
Mastocytosis (urticaria pigmentosa)
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Mastocytosis (synonym: urticaria pigmentosa) is a disease based on the accumulation of mast cells in various organs and tissues, including the skin. Clinical manifestations of mastocytosis are caused by the release of biologically active substances during mast cell degranulation. The disease is rare, occurs equally in men and women, often in children (75%).
Causes and pathogenesis of mastocytosis
There is no single point of view regarding the origin of urticaria pigmentosa. It is considered a consequence of benign or malignant proliferation of histiocytes, compared with histiocytosis, and classified in the group of tumors of the hematopoietic and lymphoid tissue (WHO, 1980). The role of mast cell growth factor produced by fibroblasts and keratinocytes and other cytokines is assumed. Opinions are expressed about the nevoid nature of mastocytoma. Familial cases of the disease indicate a possible role of genetic factors. There is no generally accepted classification. Usually, a distinction is made between cutaneous, systemic, and malignant (mast cell leukemia) forms.
Labrocytes (mastocytes, mast cells) play an important role in the development of mastocytosis. In the lesion, proliferation of mastocytes is observed. Subsequently, under the influence of immune (immune complexes, antibodies) and non-immune (medicines, heat, cold, friction, pressure, UV rays, emotional stress, food products, etc.) activators, degranulation of mastocytes and release of histamine, peptidase, and heparin occurs. Under the influence of these biologically active substances, an increase in vascular permeability, expansion of capillaries, venules, and terminal arterioles are observed, leading to a decrease in pressure, contraction of large blood vessels, stimulation of gastric secretion, etc.
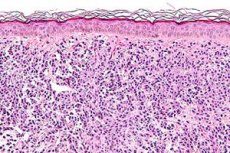
Histopathology of mastocytosis
The peculiar coloration of the elements of mastocytosis of the skin is caused by an increase in the number of melanocytes in the epidermis and the deposition of a significant amount of pigment in its lower rows, which, apparently, can be explained by complex intercellular relationships between melanocytes and mast cells.
Pathomorphology of mastocytosis
Depending on the clinical picture, the pathohistology of the skin in this disease varies. In the maculopapular and telangiectatic forms, tissue basophils are located mainly in the upper third of the dermis around the capillaries. There are few of them, and the diagnosis can only be made after staining with toluidine blue, which metachromatically stains them pinkish-lilac.
In nodular or plaque tinea, tissue basophils form large tumor-like clusters, infiltrating the entire dermis and even the subcutaneous layer.
The cells are usually cuboidal, less often spindle-shaped; their cytoplasm is massive and eosinophilic.
In diffuse mastocytosis, dense ribbon-like proliferates of tissue basophils with round or oval nuclei and clearly defined cytoplasm are present in the upper dermis. Tissue basophils in urticaria pigmentosa are distinguished by a complex composition of the carbohydrate component, which includes heparin, sialic acid-containing and neutral mucopolysaccharides, so they are stained with toluidine blue at pH 2.7 and give a positive PAS reaction.
In all the described forms of pigmented urticaria, with the exception of tedeangiectatic, eosinophilic granulocytes may be found among tissue basophils.
In forms of pigmented urticaria accompanied by the formation of vesicles or blisters, the latter are located subepidermally, and in old elements due to the regeneration of the epidermis, intraepidermally. The blisters contain tissue basophils and eosinophilic granulotypes. Pigmentation in this disease is caused by an increase in the amount of pigment in the cells of the basal layer of the epidermis, less often - by the presence of melanophages in the upper part of the dermis.
Symptoms of Mastocytosis
There are two forms of mastocytosis: cutaneous and systemic. The cutaneous form is subdivided into generalized cutaneous (urticaria pigmentosa, persistent spotted telangiectasia, diffuse mastocytosis) and mastocytoma (a tumor, usually solitary).
Urticaria pigmentosa is the most common form of cutaneous mastocytosis. At the onset of the disease, often in children, itchy pink-red spots appear, which transform over time into blisters. The blisters leave behind persistent brownish-brown spots. In adults, the disease begins with the formation of hyperpigmented spots or papules. The spots and papules are flat, up to 0.5 cm in diameter, have a rounded shape, sharp borders and a smooth surface without signs of peeling. They are located on the skin of the trunk, are few in number, have a light gray or pinkish-brownish color. Over time, the papules spread to other areas of the skin (upper and lower extremities, face), have a spherical shape, dark brown or dark brown color, sometimes with a pinkish-red tint. Often the process stops, persisting for many years, and can then progress to the development of erythroderma, affecting internal organs, which ends in death.
Pigmented urticaria in children is benign. The disease begins with the appearance of itchy urticarial rashes, which after several years transform into papular elements. At the onset of the disease, blisters (vesicles) may appear on apparently healthy skin or on spots and papules, characterized by swelling and a distinct pink-red hue. Clinically, pigmented urticaria in children is characterized by a clear exudative component. Sometimes the elements disappear without a trace. The phenomenon of inflammation, or the Darier-Unna phenomenon, is of great importance: when rubbing with fingers or a spatula or a needle prick, the elements become edematous, the pink-red color and itching of the skin intensify. Exacerbation is noted after friction, pressure, thermal procedures (hot baths, insolation).
The cutaneous form may manifest itself as maculopapular, bullous rashes, diffuse, including erythrodermic, telangiectatic changes, and also quite rarely as an isolated lesion - mastocytoma. Most often, small-spotted and papular rashes are observed, spreading mainly in childhood. They are located mainly on the trunk, somewhat less often on the limbs, rarely on the face, have round or oval outlines, reddish-brown color. After friction, the elements acquire an urticaria-like character. At the same time, there may be nodular formations, usually few in number, with more intense pigmentation. Expulsions can merge, forming plaque and diffuse lesions, in rare cases they acquire a pachydermic character with a sharply expressed diffuse infiltration of the skin.
The persistent spotted telangiectotic form occurs in adults, looks like freckles, and small telangiectasias are visible on a pigmented background.
Diffuse mastocytosis is characterized by thickening of the skin, which has a doughy consistency, a yellowish tint and resembles a pseudoxanthoma. Deepening of skin folds is noted. The lesions are often localized in the axillary fossa, inguinal folds. Cracks and ulcers may appear on the surface of the lesions.
The vesicular and atrophic forms are also described: the blisters are tense, with transparent or hemorrhagic contents, acantholytic cells are absent in them, Nikolsky's symptom is negative.
Nodular mastocytosis occurs predominantly in newborns and children in the first 21 years of life.
Clinically, there are three types of nodular mastocytosis: xanthelasmoid, multinodular, and nodular-confluent.
The xanthelasmoid variety is characterized by isolated or grouped flat nodules or nodular elements up to 1.5 cm in diameter, oval, with sharp borders. The elements have a dense consistency, a smooth or orange-peel surface, and a light yellow or yellowish-brown color, which makes them similar to xanthelasmas and xanthomas.
In multinodular mastocytosis, multiple hemispherical, dense, nodular elements with a smooth surface, 0.5-1.0 cm in diameter, pink, red or yellowish in color, are scattered throughout the skin.
The nodular-confluent variety is formed as a result of the fusion of nodular elements into large conglomerates located in large folds.
In nodular mastocytosis, regardless of its varieties, the Darier-Unna phenomenon is weakly expressed or not detected. Most patients have urticarial dermographism. A characteristic subjective symptom is itching of the skin.
Systemic mastocytosis is characterized by damage to internal organs. The disease manifests itself as mast cell leukemia (a malignant form of mastocytosis).
The erythrodermic form, which is also rare, occurs in adults without blistering reactions, unlike in children.
Diffuse-infiltrative, heleangitactic and erythrodermic forms of mastocytosis are considered potentially systemic diseases.
Bullous mastocytosis develops in children in infancy or early childhood. Blisters can be on the surface of maculopapular rashes or plaque lesions, sometimes they are the only skin manifestation of the disease (congenital bullous mastocytosis), which is considered prognostically less favorable.
Solitary mastocytoma has the appearance of a small tumor-like formation or several closely located nodules, on the surface of which blisters are typical in children. The prognosis for this type of urticaria is the most favorable. In most cases, pigmented urticaria that develops in childhood regresses on its own by puberty. On average, systemic lesions are observed in 10% of patients, mainly in the case of mastocytosis in adults.
What's bothering you?
What do need to examine?
How to examine?
What tests are needed?
Who to contact?
Treatment of mastocytosis
Treatment of mastocytosis (urticaria pigmentosa) is symptomatic. Antihistamines are recommended. In the case of a widespread skin process and severe dermatosis, glucocorticosteroids, PUVA therapy, and cytostatics (prospidin) are used. Corticosteroid ointments are used externally.


 [
[