Medical expert of the article
New publications
Malignant eyelid tumors
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

In the 60-70s of the 20th century, an independent clinical direction was identified in ophthalmology - ophthalmooncology, which should solve the issues of diagnostics and treatment of tumors of the visual organ. Tumors of this localization are characterized by high polymorphism, unique clinical and biological course. Their diagnostics is difficult, for its implementation a set of instrumental methods of research is required, which ophthalmologists are proficient in. Along with this, knowledge of the application of diagnostic measures used in general oncology is necessary. Significant difficulties arise in the treatment of tumors of the eye, its adnexa and orbit, since a large number of anatomical structures important for vision are concentrated in small volumes of the eye and orbit, which complicates the implementation of therapeutic measures while preserving visual functions.
Epidemiology
The annual incidence of tumors of the organ of vision according to patients' appeals is 100-120 per 1 million population. The incidence among children reaches 10-12% of the indicators established for the adult population. Taking into account the localization, tumors of the adnexa of the eye (eyelids, conjunctiva), intraocular (choroid and retina) and orbit are distinguished. They differ in histogenesis, clinical course, professional and life prognosis.
Among primary tumors, the most common are tumors of the adnexa of the eye, the second most common are intraocular tumors, and the third most common are tumors of the orbit.
Tumors of the eyelid skin account for more than 80% of all neoplasms of the visual organ. The age of patients ranges from 1 year to 80 years and older. Tumors of epithelial genesis predominate (up to 67%).
Causes malignant eyelid tumors
Malignant tumors of the eyelids are mainly represented by skin cancer and meibomian gland adenocarcinoma. Excessive ultraviolet radiation, especially in people with sensitive skin, the presence of non-healing ulcerative lesions, or the influence of the human papillomavirus play a role in their development.
Symptoms malignant eyelid tumors
Basal cell carcinoma of the eyelids
Basal cell eyelid cancer accounts for 72-90% of malignant epithelial tumors. Up to 95% of cases of its development occur at the age of 40-80 years. The favorite localization of the tumor is the lower eyelid and the internal commissure of the eyelids. Nodular, corrosive-ulcerative and scleroderma-like forms of cancer are distinguished.
Clinical signs depend on the form of the tumor. In the nodular form, the tumor borders are quite clear; it grows for years, as the size increases, a crater-like depression appears in the center of the node, sometimes covered with a dry or bloody crust, after removal of which a moist painless surface is exposed; the edges of the ulcer are callous.
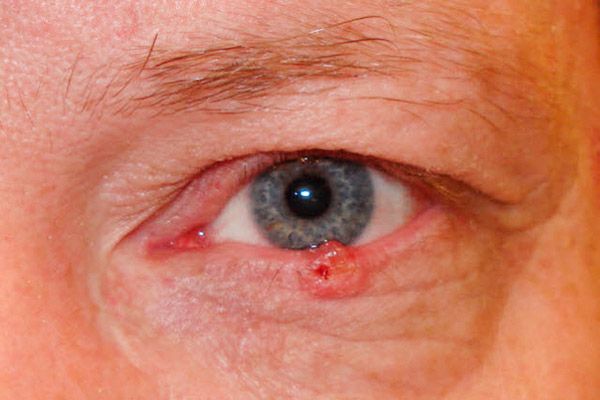
In the corrosive-ulcerative form, a small, almost invisible, painless ulcer with raised, ridge-like edges appears at first. Gradually, the ulcer area increases, it becomes covered with a dry or bloody crust, and bleeds easily. After the crust is removed, a rough defect is exposed, with lumpy growths visible along the edges. The ulcer is most often localized near the marginal edge of the eyelid, covering its entire thickness.
The scleroderma-like form in the initial stage is represented by erythema with a weeping surface covered with yellowish scales. As the tumor grows, the central part of the weeping surface is replaced by a fairly dense whitish scar, and the progressive edge spreads to healthy tissue.
 [ 17 ]
[ 17 ]
Squamous cell carcinoma of the eyelids
Squamous cell carcinoma of the eyelids accounts for 15-18% of all malignant eyelid tumors. It mainly affects older people with skin sensitive to sun exposure.
Predisposing factors include xeroderma pigmentosum, oculocutaneous albinism, chronic skin diseases of the eyelids, long-term non-healing ulcers, and excessive ultraviolet radiation.
At the initial stage, the tumor is represented by a mild erythema of the skin, most often of the lower eyelid. Gradually, a seal with hyperkeratosis on the surface appears in the erythema zone. Perifocal dermatitis appears around the tumor, conjunctivitis develops. The tumor grows for 1-2 years. Gradually, a depression with an ulcerated surface forms in the center of the node, the area of which gradually increases. The edges of the ulcer are dense, bumpy. When localized at the edge of the eyelids, the tumor quickly spreads into the orbit.

Treatment of eyelid cancer is planned after receiving the results of a histological examination of the material obtained during a tumor biopsy. Surgical treatment is possible if the tumor diameter is no more than 10 mm. The use of microsurgical equipment, laser or radiosurgical scalpel increases the effectiveness of treatment. Contact radiation therapy (brachytherapy) or cryodestruction can be performed. If the tumor is localized near the intermarginal space, only external irradiation or photodynamic therapy can be performed. If the tumor grows into the conjunctiva or orbit, subperiosteal exenteration of the latter is indicated.
With timely treatment, 95% of patients live more than 5 years.
Adenocarcinoma of the meibomian gland (gland of the eyelid cartilage)
Adenocarcinoma of the meibomian gland (a gland of the eyelid cartilage) accounts for less than 1% of all malignant eyelid tumors. The tumor is usually diagnosed in the fifth decade of life, more often in women. The tumor is located under the skin, usually of the upper eyelid, in the form of a yellowish node resembling a chalazion, which recurs after removal or begins to grow aggressively after drug treatment and physical therapy.
After removal of the chalazion, a histological examination of the capsule is mandatory.
Adenocarcinoma may manifest as blepharoconjunctivitis and meibomitis, grows rapidly, spreads to the cartilage, palpebral conjunctiva and its vaults, lacrimal ducts and nasal cavity. Given the aggressive nature of tumor growth, surgical treatment is not indicated. For small tumors limited to eyelid tissue, external irradiation can be used.
In case of metastases in regional lymph nodes (parotid, submandibular), they should be irradiated. The presence of signs of tumor spread to the conjunctiva and its vaults necessitates orbital exenteration. The tumor is characterized by extreme malignancy. Within 2-10 years after radiation therapy or surgical treatment, relapses occur in 90% of patients. From distant metastases, 50-67% of patients die within 5 years.
Melanoma of the eyelids
Eyelid melanoma accounts for no more than 1% of all malignant eyelid tumors. The peak incidence is between the ages of 40 and 70. Women are more often affected. The following risk factors for melanoma development have been identified: nevi, especially borderline nevi, melanosis, and individual hypersensitivity to intense solar radiation. It is believed that sunburn is more dangerous in the development of skin melanoma than in basal cell carcinoma. Risk factors also include an unfavorable family history, age over 20, and white skin color. The tumor develops from transformed intradermal melanocytes.

The clinical picture of melanoma of the eyelids is polysymptomatic. Melanoma of the eyelids can be represented by a flat lesion with uneven and unclear edges of a light brown color, on the surface - nested more intense pigmentation.
The nodular form of melanoma (more often observed when localized on the skin of the eyelids) is characterized by a noticeable prominence above the skin surface, the skin pattern in this area is absent, pigmentation is expressed to a greater extent. The tumor quickly increases in size, its surface is easily ulcerated, spontaneous bleeding is observed. Even with the lightest touch of a gauze napkin or cotton swab to the surface of such a tumor, a dark pigment remains on them. The skin around the tumor is hyperemic as a result of the expansion of perifocal vessels, a halo of sprayed pigment is visible. Melanoma early spreads to the mucous membrane of the eyelids, lacrimal caruncle, conjunctiva and its vaults, to the tissues of the orbit. The tumor metastasizes to regional lymph nodes, skin, liver and lungs.
Treatment of eyelid melanoma should be planned only after a complete examination of the patient to detect metastases. In case of melanomas with a maximum diameter of less than 10 mm and the absence of metastases, it can be surgically excised using a laser scalpel, radio scalpel or electric knife with mandatory cryofixation of the tumor. The lesion is removed through and through, retreating at least 3 mm from the visible (under the operating microscope) borders. Cryodestruction is contraindicated in melanomas. Nodular tumors with a diameter of more than 15 mm with a rim of dilated vessels are not subject to local excision, since metastases are usually already observed in this phase. Radiation therapy using a narrow medical proton beam is an alternative to orbital exenteration. Regional lymph nodes should also be irradiated.
The prognosis for life is very severe and depends on the depth of tumor spread. In the nodular form, the prognosis is worse, since vertical invasion of tissues by tumor cells occurs early. The prognosis worsens when melanoma spreads to the costal margin of the eyelid, intermarginal space and conjunctiva.
What do need to examine?
How to examine?
Who to contact?

