Medical expert of the article
New publications
Keratoma
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
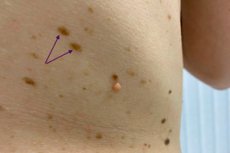
A keratoma is a benign tumor that develops on the skin and is characterized by an overgrowth of keratinized cells that make up the upper layer of the epidermis (the outer layer of the skin). These neoplasms usually appear as flat, furrowed, or raised areas of skin that can come in a variety of colors, including brown, black, pale, or pigmented.
These tumors are usually benign and not life threatening. However, it is important to watch for any changes in the skin masses and see a doctor if the keratoma begins to grow, change color, become painful or cause concern, as they can sometimes be associated with other skin problems. If the doctor thinks the keratoma may be suspicious for malignant changes, it may be removed.
Causes of the keratomas
Keratomas usually develop due to a variety of factors including:
- Age: As we age, the skin undergoes a natural aging process that can lead to the development of keratomas. Keratomas most commonly appear in adults and older people. Read also: senile keratoma.
- Genetic predisposition: In some people, a family history of keratomas may increase the likelihood of their occurrence.
- UV radiation: Prolonged exposure to ultraviolet (UV) radiation from the sun or sunlamps may increase the risk of developing keratomas.
- Trauma or irritation: Trauma, pressure, friction, scratching or irritation of the skin can contribute to the development of keratomas.
- Viral infections: Some viral infections, such as human papillomavirus (HPV), may be associated with the appearance of keratomas.
- Hormonal changes: Hormonal changes, such as pregnancy or the use of hormonal medications, can affect the skin and contribute to the appearance of keratomas.
- Tobacco smoking: Some studies have linked smoking to an increased risk of keratomas.
Pathogenesis
The pathogenesis of keratoma is related to the overgrowth and accumulation of keratinized cells in the upper layers of the skin (epidermis). Here's how it happens:
- Epidermal hyperproliferation: Initially, there is increased division and multiplication of epidermal cells. This can be caused by various factors such as exposure to ultraviolet (UV) radiation, trauma, hormonal changes or viral infections.
- Keratin accumulation: As a result of increased cell proliferation, keratinized cells begin to accumulate in the upper layers of the epidermis. Keratin is a protein that forms a tough, irreducible horny part of the skin.
- Formation of furrows and ridges: Keratinized cells form into hard, flat or protruding areas on the skin, which are called keratomas. These formations can vary in color and shape depending on the type of keratoma and other factors.
- Location: The location of keratoma formation can vary and it can appear on different parts of the body including face, neck, back, chest, limbs, etc.
- Benign: It is important to note that keratomas are usually benign and not life-threatening. However, in rare cases, they may undergo changes and become suspicious for malignant changes, in which doctors are required to perform biopsy studies to confirm the diagnosis.
In general, the pathogenesis is associated with hyperproliferation and keratinization of the epidermis, resulting in the formation of characteristic cutaneous masses on the skin surface.
Symptoms of the keratomas
The symptoms of a keratoma can vary depending on its type and characteristics. Here are the common signs that may accompany a keratoma:
- Protruding mass: A keratoma is usually a flat or protruding skin involvement that may have an uneven or raised surface.
- Color: The color of a keratoma can vary from brown and blackish to yellowish, pale or even black, depending on the type of keratoma and other factors.
- Size: Keratomas can also vary in size. They can be small and less than a centimeter in diameter or larger.
- Shape: The shape of a keratoma can be varied, including flat, furrowed, spiky, or other shapes.
- Feelings: Keratomas usually do not cause pain or itching. However, in some cases, especially if they are large or thick, they may cause minor irritation or discomfort.
- Changes over time: Keratomas can remain stable for many years, but they can also change in color, size, or shape over time.
- Self-transition: Some keratomas may eventually disappear without any treatment, but this does not always happen.
Forms
Keratomas can have different types, depending on their characteristics and origin. Some of the most common types of keratomas are listed below:
- Seborrheic Keratomas (Seborrheic Keratosis): These are the most common types of keratomas. Seborrheic keratomas are often brown in color and have an uneven, rough surface. They can appear on the face, neck, back, chest, and other parts of the body.
- Actinic Keratomas (Actinic Keratosis): Saline keratomas are usually caused by prolonged exposure to ultraviolet (UV) radiation from the sun. They often appear on exposed areas of the skin such as the face, ears, hands, and neck. Saline keratomas may be flatter and darker than rusty keratomas and may have a rough texture.
- Hyperkeratosis: This term can be used to describe areas of the skin where there is an excessive accumulation of keratin. Hyperkeratosis can be caused by a variety of factors and may not always represent a separate tumor.
- Keratoacanthoma (Keratoacanthoma): This is a benign skin tumor that can resemble skin cancer, but most often it remains limited and does not spread. Keratoacanthomas may be protruding and have a central ulceration.
- Dermatofibroma (Dermatofibroma): This is a hard tumor that is usually brownish-red or brown in color. It may be protruding and have a dense texture.
- Darier's Disease: This is a rare genetic disorder characterized by the appearance of keratomas and other skin changes. It is hereditary and requires close medical supervision.
- Follicular keratomas (Keratosis Pilaris): This is a condition in which small white or skin-like bumps appear on the skin, usually on the upper extremities. They may have a texture that resembles chicken skin.
These types of keratomas can vary in appearance, localization, and possible causes.
Diagnostics of the keratomas
Keratoma diagnosis is usually based on the external characteristics of the mass and a physical examination by a dermatologist. The doctor takes the following steps for diagnosis:
- Visual inspection: The doctor carefully examines the skin mass to assess its size, color, shape, texture, and other characteristics. This helps distinguish keratomas from other skin growths such as molars or warts.
- Medical History: The doctor may ask questions about the length of time the keratoma has existed, changes in its appearance, any symptoms (if any), and other factors that may be associated with the keratoma.
- Biopsy: In some cases, especially if the keratoma is worrisome or a malignant change is suspected, the doctor may decide to perform a biopsy. In a biopsy, a small tissue sample from the keratoma is taken for laboratory analysis to ensure that it is a benign mass and to rule out skin cancer.
- Dermatoscopy: Dermatoscopy is a technique in which the doctor uses a special device called a dermoscope to examine skin growths in more detail. This allows the structure and characteristics of the keratoma to be better defined.
After these diagnostic methods are performed, the doctor will be able to make a final diagnosis and determine whether the mass needs to be treated or removed.
Differential diagnosis
Differential diagnosis of keratoma involves identifying and distinguishing this benign mass from other skin changes and pathologies. It is important to perform the differential diagnosis with an experienced dermatologist, as many skin diseases and masses have similar symptoms. Below are some points that may help in the differential diagnosis of keratoma:
- Seborrheic keratosis: Seborrheic keratosis is also a benign growth and may resemble a keratoma in appearance. However, seborrheic keratosis is usually brownish-black in color and may be slightly oily to the touch.
- Squamouskeratosis: This is a precancerous skin condition caused by long-term exposure to ultraviolet rays. Squamous keratosis can be similar to solar keratoma, but it is usually harder and rougher to the touch, and has an increased risk of developing into squamous cell skin cancer.
- Melanoma: melanoma is a malignant skin tumor that can sometimes mimic a keratoma in color and shape. However, melanoma is more likely to have irregular color, jagged edges, and may change in size over time. Any suspicion of melanoma requires immediate consultation with a physician.
- Basalioma: basalioma is the most common type of skin cancer. It may look like an early keratoma, but it can ulcerate, bleed, and have a depression in the center.
- Scabies: Sometimes scabies symptoms can be similar to keratoma symptoms, including itching and redness. However, scabies usually has characteristic symptoms such as a furrowed rash, redness in skin folds, and sores.
- Intraductal papillomatosis of the breast: This is a benign mass that can occur in the nipple area and has a similar appearance to a keratoma. However, it usually occurs on the nipples and may be associated with nipple discharge.
The best way to make a differential diagnosis and rule out malignancy is to consult a dermatologist. The doctor will perform an examination, possibly take a biopsy for laboratory analysis to confirm the nature of the mass and determine the best method of treatment or removal.
Who to contact?
Treatment of the keratomas
Keratoma treatment depends on its characteristics and medical necessity. In most cases, keratomas are benign and may not require treatment, especially if they are not bothersome or uncomfortable. However, in some cases, treatment or removal of the keratoma may be necessary. Treatment is decided by a dermatologist and may include the following methods:
- Observation and evaluation: If the keratoma is small, symptom-free, and not bothersome, the doctor may decide not to treat it immediately. Instead, he or she will observe the mass regularly to monitor any changes.
- Removal: If a keratoma is causing cosmetic concern, irritation, or a suspected malignant change, your doctor may recommend removal.
- Biopsy: If the physician suspects that a keratoma may be malignant or if it has atypical features, a biopsy may be recommended for further evaluation.
- Symptom Management: If a keratoma causes itching, irritation, or soreness, your doctor may prescribe treatment to relieve symptoms. This may include applying ointments or creams to help reduce itching and irritation.
It is important to see a dermatologist for a professional evaluation and consultation. The doctor will be able to determine the best approach to treating or managing your case based on individual factors.
Keratoma ointments
Keratoma treatment may involve the use of various ointments and creams, however, it is important to remember that a keratoma is a benign growth and its treatment is usually done to improve appearance or discomfort. Below are some ointments and creams that can be used in the treatment of keratoma:
- Salicylicointment: Salicylic acid-based ointment can help soften the top layer of the tumor and help it peel off. This method is called keratolytic treatment.
- Urea(urea)ointment: Urea ointment can also help soften and moisturize the neoplasm, which may make it easier to remove.
- Retinoidcreams: Retinoids, such as tretinoin, can help to speed up skin cell renewal and reduce the thickness of keratomas. However, their use requires a doctor's supervision as they can cause skin irritation.
- HomeopathicOintments: Some homeopathic ointments, such as flower wax ointment, can also be used to moisten and soften swelling.
It is important to note that ointments and creams can only help in cases where the keratoma is not causing significant concern or discomfort. If you suspect a malignant change or if the neoplasm is causing severe discomfort, it is best to see a dermatologist. Your doctor may recommend removal methods such as cryotherapy (freezing), surgical removal, or laser removal for more effective treatment.
Keratoma removal
Keratoma removal may be recommended by your doctor in the following cases:
- Cosmetic considerations: If the keratoma is located in a prominent location and is of cosmetic concern, the patient may wish to have it removed.
- Due to friction or irritation: If the keratoma is located in an area where it is exposed to friction from clothing or shoes, it may cause irritation or discomfort.
- Suspicion of skin cancer: If your doctor suspects that a keratoma may be malignant or if it shows atypical signs (such as changes in color, shape, or size), it may be recommended for biopsy and removal.
There are various methods for keratoma removal and the choice of method depends on its size, location and characteristics. Some of the methods for keratoma removal include:
- Excision: The doctor removes the neoplasm with a small surgical procedure. This may require stitches.
Keratoma excision is a method of keratoma removal using a small surgical procedure. This method is usually performed by a dermatologist or surgeon and involves the following steps:
- Preparing the area: The skin around the tumor is cleaned and disinfected.
- Anesthesia: The patient may be offered local anesthesia in the area of removal to reduce pain.
- Excision: The doctor uses a surgical instrument such as a scalpel to gently cut the keratoma out of the skin. In the case of large keratomas, sutures may be used to close the wound.
- Stitches and post-procedure care: If necessary, the doctor may use stitches to close the wound. There may be temporary changes in the skin after the procedure, such as redness and swelling. Your doctor will give instructions on wound care and may recommend the use of ointments or antiseptics.
The advantages of excision include complete removal of the keratoma and the ability to biopsy if the doctor suspects malignant changes. However, this method can leave a scar, especially with large excisions.
The decision on the method of keratoma removal will depend on the characteristics of the mass, its location, and the doctor's judgment.
- Electrocoagulation: This method uses an electric current. It is often used for small masses.
Keratoma electrocoagulation is one method of keratoma removal that uses an electric current to burn and remove the keratoma. This method is usually performed by a dermatologist or surgeon and involves the following steps:
- Preparing the area: The skin around the tumor is cleaned and disinfected.
- Anesthesia: Depending on the size and location of the neoplasm, the doctor may use local anesthesia to reduce the patient's pain.
- Electrocoagulation procedure: The doctor uses a special device called an electrocoagulator to apply an electric current to the keratoma. This causes the tissue to heat up and coagulate, which means the keratoma is burned and removed. The procedure can be spot-on and controlled, allowing the doctor to remove the keratoma layer by layer.
- Aftercare: Redness, crusting, or slight soreness in the area of removal may occur after the procedure. Your doctor will give instructions on wound care and may recommend the use of ointments or antiseptics.
The benefits of electrocoagulation include less bleeding and good control over the procedure. However, as with any surgical procedure, there can be risks and complications such as scarring or changes in skin pigmentation.
Electrocoagulation is an effective method for keratoma removal, and the decision to use it is made by the doctor based on the characteristics of the keratoma and the patient.
- Laser removal: Laser removal can be effective for small masses and usually leaves no stitches.
Laser keratoma removal is one method of keratoma removal that can be effective for small and benign keratomas. The laser keratoma removal procedure is usually performed in a dermatologist's or surgeon's office and may include the following steps:
- Preparing the area: The skin around the tumor is cleaned and disinfected.
- Anesthesia: Depending on the size and location of the neoplasm, the doctor may apply local anesthesia around the mass to reduce pain and discomfort.
- Laser removal procedure: The doctor uses a laser device to aim a laser beam at the keratoma. The laser beam is pinpointed on the skin to remove the keratoma. The procedure may take only a few minutes.
- Post-procedure care: After keratoma removal, there may be temporary changes to the skin such as redness, crusting, or minor abrasions. Your doctor will give instructions on how to care for the treated area, including the application of ointments and wound care.
Advantages of laser keratoma removal include less bleeding, less risk of infection, and more precise removal of the mass than some other methods. However, this method can be more expensive and require a longer recovery time than some other methods.
After the procedure, it is important to follow the doctor's recommendations and care for the wound to avoid complications and ensure good healing.
- Cryotherapy: This method involves freezing the neoplasm with liquid nitrogen, which causes it to detach.
Cryotherapy is a keratoma removal method that uses extremely low temperatures to freeze and destroy the keratoma. This method is often used to remove benign growths on the skin. The cryotherapy procedure involves the following steps:
- Preparing the area: The skin around the tumor is cleaned and disinfected.
- Cryotherapy procedure: The doctor uses a special device called a cryoapplicator or cryopistol to apply liquid nitrogen or other refrigerated gas to the keratoma. This causes extreme cooling and freezing of the tissue of the neoplasm.
- Thawing: After a keratoma is frozen, the tissue begins to thaw and necrotic tissue forms, which eventually breaks away from healthy skin.
- Aftercare: After cryotherapy, the area is usually crusted or ulcerated and will heal over time. Your doctor may recommend the use of ointments or antiseptics to care for the wound.
The benefits of cryotherapy include no need for stitches, less bleeding, and good effectiveness for keratoma removal. However, the healing process can take some time, and in some cases, multiple cryotherapy sessions may be required.
The decision on the method of keratoma removal will depend on the characteristics of the mass, its location, and the doctor's judgment.
- Chemical removal: Your doctor may apply special chemicals to the tumor to make it peel away.
Chemical keratoma removal is a method that uses chemicals to break down and remove the neoplasm from the skin. This method can be used to remove the tumor, especially if it is small and benign. The procedure for chemical keratoma removal involves the following steps:
- Preparation of the area: The skin around the neoplasm is cleaned and disinfected.
- Chemical application: A doctor or medical professional applies a chemical that contains active ingredients that can destroy keratomas. These agents may include salicylic acid, trichloroacetic acid (TCA), urea, and other substances.
- Dwell time: The chemical is left on the tumor for a certain amount of time, depending on the drug used and the doctor's instructions.
- Removing the chemical: After thechemical has aged on the neoplasm, it is removed and the area is rinsed thoroughly.
- Aftercare: Redness, swelling, or crusting may occur after chemical removal of a keratoma. Your doctor will give instructions for wound care, including the use of ointments or antiseptics.
Benefits of chemical removal include no surgery and no stitches, as well as the ability to have the procedure done in a doctor's office. However, as with any removal method, there may be temporary changes to the skin and risks of complications.
- Radiofrequency keratoma removal is one of the methods of removing benign skin growths. This method is often used in dermatology and cosmetology to effectively and painlessly remove the growths. Here's how the radiofrequency removal procedure works:
- Preparation: The doctor will do a preliminary evaluation of the tumor to make sure it is suitable for radiofrequency removal.
- Anesthesia: The procedure is usually performed using local anesthesia. This helps to avoid pain and discomfort during the procedure.
- Procedure: The doctor uses a special device called a radio wave machine. This device generates radio wave energy that creates high-frequency electrical discharges. These discharges target the neoplasm, destroying its cells and stopping bleeding in parallel. The procedure is spot-on and removes the keratoma layer by layer.
- Healing: After keratoma removal, a crust forms on the skin, which usually disappears within a few weeks. It is important to follow the doctor's recommendations for the care of the treated area to avoid infection and speed up the healing process.
Radiofrequency removal is generally considered a safe and effective method. The procedure usually takes a small amount of time and most patients can return to their daily activities the same day. However, as with any procedure, there are some risks and these may include minor scarring, skin discoloration in the area of removal, and long-term healing.
Keratoma treatment with folk remedies
Treating keratoma with folk methods at home can be effective if you prefer alternative methods. However, it is important to remember that folk methods may not be suitable for all cases and do not always guarantee success. Before using folk remedies, be sure to consult a dermatologist to ensure that the keratoma does not show signs of malignant growth and you can use these methods safely. Here are some folk methods that can be tried for treatment:
- Garlic: Some people claim that applying a small amount of garlic to a keratoma can help in shrinking it. However, garlic can cause skin irritation, so you should be careful when applying it.
- Onions: Fresh onions can also be used to treat this tumor. Apply a piece of onion on the mass and secure it with a bandage. Change the onion every few hours.
- Apple cidervinegar: Soak a piece of absorbent cotton in apple cider vinegar and apply it to the neoplasm. This may help in softening it.
- Soda: Mix baking soda and water to form a paste and apply it to the keratoma. Leave it on for a few minutes and then rinse it off. This method can be repeated several times a week.
- Aloe vera: Aloe vera gel can help moisturize and reduce inflammation around the swelling.
- Honey: Apply some honey to the keratoma and secure with a bandage. Honey can help reduce inflammation.
- Coconut oil: Massaging the neoplasm with coconut oil several times a day can help soften it.
Keep in mind that results from folk methods can vary, and they do not always guarantee keratoma removal. If you notice an increase in size, change in color or shape of the mass, see a doctor for professional evaluation and possible removal.
The decision on the method of keratoma removal is best made in consultation with a dermatologist, who will evaluate and suggest the best treatment option for your particular case.
After the tumor is removed, it is important to follow your doctor's recommendations for wound care and preventing possible complications.
Prevention
Keratomas often develop on the skin as a result of long-term exposure to the sun's ultraviolet rays and skin aging. A number of recommendations can be followed to prevent keratomas and minimize their appearance:
- Sun protection: Use sunscreen with SPF (Ultraviolet Protection Factor) when going out in the sun. Wear wide-brimmed hats and protective clothing. Avoid prolonged exposure to sunlight, especially during periods of peak sun activity.
- Avoid tanning beds: Using tanning beds can also increase the risk of developing keratomas. Therefore, try to avoid or minimize the use of tanning beds.
- Moisture and skin care: Mo isturize your skin regularly by using skin care creams and lotions. Hydrated skin may be less likely to develop keratomas.
- Avoid trauma and grated: Try to avoid mechanical trauma and grated skin.
- Regular check-ups: Perform regular skin self-checks and contact your dermatologist if you notice new or changing growths on your skin.
- Healthy Lifestyle: Lead a healthy lifestyle, including a balanced diet, moderate physical activity and quitting smoking, as this can reduce the risk of developing skin problems.
- Regular checkups with a dermatologist: If you have a predisposition to keratomas or already have a certain number of growths, regular visits with a dermatologist can help with early detection and removal of new growths if necessary.
Forecast
The prognosis of keratomas is usually favorable, as they are benign growths on the skin. In most cases, these tumors do not pose a threat to the patient's life and health. However, the prognosis may change depending on the following factors:
- Keratoma type: There are several different types of these neoplasms, and some may be more prone to change or become malignant. For example, a seborrheic type keratoma has a low chance of malignant transformation, while an actinic type keratoma (solar keratosis) may be associated with a risk of developing skin cancer.
- Removal and treatment: In most cases, keratomas can be safely removed. After removal, it is important to monitor the healing process and consult a doctor if necessary.
- Following your doctor's recommendations: If you already have keratomas or are at an increased risk of developing them, it is important to follow your doctor's recommendations and have regular skin checks.
Following your doctor's advice, protecting your skin from sunlight, and removing the tumor in a timely manner can help maintain a favorable prognosis and prevent complications.
A few classic books and authors in the field of oncology that may be helpful
- "Cancer: Principles & Practice of Oncology" - Authors: Vincent T. DeVita Jr, Theodore S. Lawrence, Steven A. Rosenberg, et al.
- "The Emperor of All Maladies: A Biography of Cancer" - Author: Siddhartha Mukherjee
- "Oxford Textbook of Oncology" - By David J. Kerr, Daniel G. Haller, Cornelis J. H. Van de Velde, et al.
- "Principles and Practice of Gynecologic Oncology" - Authors: Dennis S. Chi, Andrew Berchuck, Robert L. Coleman, et al.
- "The Biology of Cancer" by Robert A. Weinberg.
- "Clinical Oncology" - Authors: Martin D. Abeloff, James O. Armitage, John E. Niederhuber, et al.
- "Oncology: An Evidence-Based Approach" - Authors: Alfred E. Chang, Patricia A. Ganz, Daniel F. Hayes, et al.
Literature used
- Chissov, V. I. Oncology: National Manual. Brief edition / ed. By V. I. Chissov, M. I. Davydov - Moscow: GEOTAR-Media, 2017. I. Chissov, M. I. Davydov - Moscow: GEOTAR-Media, 2017.
- Butov, Y. S. Dermatovenerology. National guide. Brief edition / edited by Y. S. Butov, Y. K. Skripkin, O. L. Ivanov. - Moscow: GEOTAR-Media, 2020.

