Medical expert of the article
New publications
Keratitis in children
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Interstitial keratitis
Reasons:
- leprosy;
- tuberculosis;
- onchocerciasis;
- herpes simplex;
- measles.
Nummular keratitis
Multiple small opacities in the anterior corneal stroma:
- adenoviral keratitis;
- herpes simplex;
- chickenpox - herpes zoster,
- Epstein-Barr virus;
- sarcoidosis;
- onchocerciasis.

Epidemic keratoconjunctivitis
Bacterial keratitis
Predisposing factors
- Injury.
- Surgical intervention.
- Immunodeficiency.
- Long-term exposure of the cornea to adverse factors;
- Dry eye syndrome.
- Wearing contact lenses.
- Severe general diseases.
- Trichiasis.
- Ionizing radiation - dry eye syndrome.
- Long-term instillation of steroid drugs.
- Use of keratotoxic drugs.
Infectious agents
Certain clinical manifestations may indicate the causative agent of the disease.
- Pseudomonas causes rapidly progressing corneal ulcers with leukomalacia. The process especially often affects young children and patients using contact lenses.
- Moraxella causes conjunctivitis of the outer canthus.
- Staphylococcus spp.
- trauma, surgery or prolonged exposure to adverse factors;
- Staph, aureus can provoke the development of a corneal ulcer with accompanying hypopyon.
- Streptococcus:
- use of contact lenses;
- local damage to corneal tissue;
- chronic dacryocystitis;
- rapidly progressing corneal ulcers with undermined edges.
- Gonococcus.
- Gram-negative flora:
- E. coli;
- Aerobacter,
- Proteus spp.;
- Klebsiella spp.
They have affinity for the cornea, especially in the presence of underlying diseases.
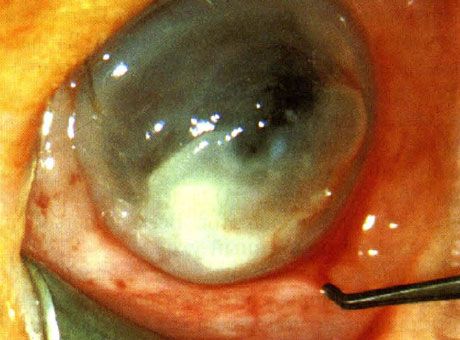
Pseudomonas keratitis in a newborn. No predisposing factors identified
 [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ]
[ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ]
Eyeball injection in early childhood
- Conjunctivitis:
- discharge, conjunctival injection;
- lacrimation, visual acuity is not reduced.
- Keratitis:
- conjunctival injection, discomfort, lacrimation;
- discharge, photophobia.
- Endophthalmitis:
- pain, low vision, mixed injection;
- lacrimation, discharge.
- Uveitis:
- pain, photophobia, blurred vision;
- mixed injection, lacrimation.
- Chorioretinitis:
- low vision, floaters in front of the eye, eyeball injection;
- subconjunctival hemorrhage, eyeball injection.
- Glaucoma:
- pain, mixed injection;
- photophobia, low vision.
- Conjunctival infiltration in leukemia:
- local infiltration;
- conjunctival injection.
- Vascular system malformations:
- Sturge-Weber syndrome;
- disturbance of development of orbital vessels.
- Sclerites:
- pain, deep injection;
- pain when moving.
- Episcleritis:
- local conjunctival and subconjunctival injection;
- lacrimation, mild discomfort, feeling of "dryness" in the eye, injection, scanty discharge.
- Foreign body:
- local injection, sensation of "sand" in the eye;
- foreign body sensation.
- Injury:
- direct trauma;
- closed head injury causing the development of carotid-cavernous fistula.
Viral keratitis
The main manifestation of viral keratitis caused by the herpes simplex virus is punctate opacities of the cornea. Sometimes, in acute primary infection, opacities are transformed into dendritic keratitis, usually combined with skin lesions. Antiviral drugs such as idoxuridine, triflurotimidine or acyclovir are prescribed.
Keratitis characterized by the formation of deep infiltrates without signs of purulent inflammation (for example, discoid) occurs. In these cases, treatment is carried out with antiviral agents in combination with steroid drugs.
Other viral keratitis that are not prone to purulent inflammation and ulceration include adenoviral keratitis, keratitis in molluscum contagiosum, papillomatous and warty forms of the disease, and the Epstein-Barr virus.
Keratitis of fungal etiology
Keratitis caused by fungal flora occurs in weakened children or in the presence of concomitant diseases of the organ of vision. Examples are immunologically weakened children receiving general steroid therapy, patients with long-term non-healing wounds, as well as those who have suffered an eye injury or suffer from dry eye syndrome.
Pathogens
- Actinomyces.
- Candida.
- Nocardia.
- Fusarium.
- Mold.

Bilateral Candida keratitis in a severely immunocompromised child
Characteristic signs are leukomalacia, torpid course, resistance to antibiotics and the emergence of satellite foci.
Keratitis caused by protozoa
Acanthamoeba keratitis occurs in contact lens wearers and salt water bathers. Acanthamoeba causes chronic, slow-healing ulcers and corneal stromal infiltrates in association with anterior uveitis. Instillations of 0.1% propamidine isethionate, 0.15% dibromopropamidine, and miconazole or neomycin are effective.
Where does it hurt?
What do need to examine?
How to examine?
Who to contact?
Treatment of keratitis in children
All dead, necrotic tissue is removed. Contact lenses are discontinued. Any unfavorable factors should be identified and eliminated. In some cases (young child), it is advisable to prescribe sedatives. All patients require qualified care.
Treatment is prescribed immediately, before the flora sensitivity to antibiotics is detected. Antibiotic instillations are recommended every hour (or every half hour). It is desirable that the antibiotics do not contain preservatives that have a toxic effect on the cornea. Chloromycin, gentamicin or cephalosporin solutions are used.

