Medical expert of the article
New publications
Hypospermia
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
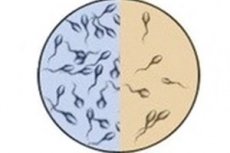
The concentration of spermatozoa in one milliliter of semen less than the lower reference (physiologically normal) limit is defined as hypospermia (from Greek hypo - below) or oligospermia (from Greek oligos - few, insignificant).
In addition, when sperm counts are low, significant abnormalities in sperm morphology and motility may be detected, called oligoasthenoteratozoospermia.
Epidemiology
According to a review published by the journal Human Reproduction Update. Male factors are responsible for about half of all infertility problems.
But how widespread oligospermia is, experts do not know exactly, because it is usually detected only when a couple can not conceive a child and turns to doctors.
According to some data, idiopathic hypospermia occurs in 60% of men with infertility. Genetic factors account for 15-30% of cases of oligozoospermia, and 7.5-10% of cases are due to microdeletions of the Y chromosome.
Causes of the hypospermia
The complex process of producing sperm requires normal functioning of the testicles (testicles), as well as the hypothalamus and pituitary glands of the brain, which produce the necessary hormones.
Although in clinical practice oligospermia is recognized as idiopathic in many patients, the causes of reduced sperm counts are many and varied.
Thus, testibular insufficiency is associated with varicocele or hydrocele; cryptorchidism (testicular failure); swelling or testicular cysts (and/or its epididymis); scrotal trauma with testicular hematoceles; genitourinary infections; testicular tumors; previous mumps or previous testicular surgery.
Possible causes of hypospermia include defects in the seminal tubules and ducts of various etiologies, including cystic fibrosis in cystic fibrosis; testicular compression by a large inguinal hernia; and retrograde ejaculation (resulting from trauma, tumor, or surgery on the urogenital tract and prostate).
Very often the causes of hypospermia are disorders of hormonal regulation of spermatogenesis, among others:
- Hypergonadotropic (primary) hypogonadism, such as in congenital klinefelter syndrome (syndrome 47 XXY) - with increased levels of FSH (follicle-stimulating hormone) and LH (luteinizing hormone) against a background of decreased or normal testosterone levels;
- Hypogonadotropic or secondary hypogonadism with a congenital form as kallman syndrome (Kallman);
- Hyperprolactinemic hypogonadism (in pituitary neoplasms or hypothyroidism);
- Glucocorticoid excess in icenko-Cushing syndrome (hypercorticism), etiologically related to an ACTH (adrenocorticotropic hormone) secreting pituitary tumor;
- Androgen resistance syndrome (or Morris syndrome) - with congenital androgen receptor deficiency, which is a protein encoded by a gene located on the proximal long arm of the X chromosome.
Genetic causes also include:
- Microdeletions (structural rearrangements) of the Y chromosome;
- Mutations in the BRCA2 tumor suppressor gene, which is located on the long arm of chromosome 13;
- Mutations in the gene encoding the testicular protease enzyme USP26, which is specifically expressed in testicular tissue and regulates protein metabolism during spermatogenesis.
Risk factors
A man's reproductive health is related to his overall health, so risk factors for hypospermia are considered to be:
- Smoking, alcohol abuse, drug use;
- Anabolic steroid use and hormone treatment;
- Testicular overheating;
- Sedentary work;
- Overweight (obesity);
- The negative effects on the testicles of herbicides, pesticides, benzene, heavy metals, radiation, and chemotherapy and radiation therapy;
- Celiac disease (gluten enteropathy);
- Renal failure;
- Hyperthyroidism;
- Congenital adrenal hyperplasia.
Pathogenesis
The mechanism of sperm count reduction depends on its underlying cause. Thus, the pathogenesis of hypospermia after mumps (mumps), the causative agent of which is a virus of the family Paramyxoviridae, is due to its complication in the form of parotitis epididymitis, orchitis, orchoepidididymitis (inflammation of the testis and its appendage), leading to testicular atrophy and abnormal spermatogenesis. Also read - spermatozoa and spermatogenesis
The spermatogenesis impairment leading to decreased sperm concentration seen in scrotal trauma, varicocele, cryptorchidism, infections or tumors of the testicles and prostate is due to the action of antisperm antibodies, produced by the body against sperm antigens.
Spermatogenesis is carried out by several types of specialized cells with the participation of a number of hormones. Every hour and a half, the hypothalamus secretes gonadotropin-releasing hormone (GnRH), which causes the pituitary gland to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Once in the testes, FSH stimulates Sertoli cells (which provide trophic support for developing spermatozoa and support spermatogenesis) and LH stimulates testosterone-producing interstitial cells (Leydig cells).
For example, decreased sperm production in secondary hypogonadism is due to decreased LH secretion, which in turn leads to decreased testosterone production in the testes (intratesticular testosterone), the main hormonal stimulus of spermatogenesis.
Elevated FSH levels indicate abnormal spermatogenesis in cases of hypergonadotropic hypogonadism.
Decreased spermatogenesis in Icenko-Cushing's syndrome is the result of secondary testicular dysfunction due to decreased LH production and decreased testosterone levels.
And the origins of the problem with the number of sperm produced by the testicles in the presence of hyperthyroidism or liver disease lie in the increased levels of sex hormone binding globulin (hSBG) synthesized by the liver, which causes androgen deficiency.
Symptoms of the hypospermia
Men with hypospermia have no clinical symptoms. This pathology is divided into three categories or stages: mild (with a sperm count of 10-15 million /ml); moderate (with 5-10 million sperm in one ml of ejaculate) and severe (when the sperm count is less than 5 million /ml).
Sperm concentration fluctuates and oligospermia may be temporary or permanent.
Complications and consequences
Complications and consequences of hypospermia are manifested by a problem with fertility (ability to conceive) up to male infertility.
Diagnostics of the hypospermia
Hypospermia is detected when a couple is unable to conceive and seeks medical attention.
How the diagnosis is made (instrumental and differential) and what tests are necessary, in detail in the publication - male infertility - Diagnosis
Who to contact?
Treatment of the hypospermia
For most cases of hypospermia, including idiopathic hypospermia, there are no direct medications with recognized efficacy. Such drugs as Clomiphene citrate (50 mg tablets 1-2 times a day, therapy course - 1.5 months), and in case of pituitary hypogonadism - injectable gonadotropic drug Menotropin have been experimentally tested and started to be used. Also used are combined low doses of estrogen and testosterone, Acetyl-L-carnitine, vitamins C, D and E. That is, therapy is carried out as part of the treatment of infertility. More in the material - male infertility - Treatment
From the latest "findings" of Western specialists (confirmed by randomized controlled trials) - as a means to stimulate sperm production in men with oligospermia - it is suggested to take ramipril, which is an ACE (angiotensin-converting enzyme) inhibitor used for the treatment of arterial hypertension.
Hypospermia can also be treated with stem cells isolated from the patient's adipose tissue, which are propagated in a laboratory and injected into the patient.
Herbal treatments may be used in addition, and most commonly recommended are seeds of fenugreek of the hay family (Trigonella foenum-graecum) of the legume family, extract or powder from the root of licorice naked (Glycyrrhiza glabra) of the same family, and Withania somnifera of the nightshade family, which is called ashwagandha in Ayuverda,
And varicocele, cryptorchidism, testicular tumors, or problems with the seminal ducts may require surgical treatment.
Also read tips for increasing sperm count.
Prevention
There are no special measures to prevent hypospermia, but general recommendations for a healthy lifestyle. If possible, the etiologic cause of the disease should also be treated.
Forecast
Hypospermia has no effect on life expectancy, and the prognosis for a man's ability to become a father without resorting to assisted reproductive technologies depends largely on the cause of low sperm count.
List of authoritative books and studies related to the study of hypospermia
- "Male Infertility: A Clinical Guide" - by David R. Meldrum (Year: 2011)
- "Spermatogenesis: Methods and Protocols" - by Zhibing Zhang, Meijia Zhang (Year: 2013)
- "Male Infertility: Understanding, Causes, and Treatment" - by Charles M. Lindner (Year: 2014)
- "Spermatogenesis: Biology, Mechanisms and Clinical Outlook" - by Isabelle S. Desrosiers, L. Ian L. Ian (Year: 2009)
- "Male Reproductive Cancers: Epidemiology, Pathology and Genetics" - by Peter Boyle, et al. (Year: 2009)
- "Hypogonadism in Men" - by Stephen J. Winters, et al. (Year: 2015)
- "Spermatogenesis: Methods and Techniques" - by Shuo Wang, et al. (Year: 2016)
- "Infertility: Diagnosis and Management" - by Stuart S. Howards, Eric A. Klein (Year: 2004)
- "Spermatogenesis: Experimental and Clinical Studies" - by Rosario Pivonello (Year: 2016)
- "Hypogonadism in Men: Clinical Features, Diagnosis, and Treatment" - by Adrian S. Dobs, Kate Strohecker (Year: 2017)
Literature
Lopatkin, N. A. Urology: National Guide. Brief edition / Edited by N. A. Lopatkin - Moscow: GEOTAR-Media, 2013.

