Medical expert of the article
New publications
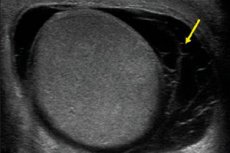
Testicular hematoceles
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Hematocele is a medical term meaning a pathological accumulation of blood in body cavities. Most often, this pathology occurs in the male genital area - in particular, in the scrotum and vaginal membrane of the testicles. Therefore, when mentioning this pathology, most specialists mean testicular hematocele.
The vaginal tunic is a kind of protective barrier surrounding the testicles (each testicle separately). This tunic should not be confused with the scrotum, which is a skin-muscle bursa.
Hematocele usually results from bleeding from damaged blood vessels. This happens with traumatic injuries, surgical manipulations. In some patients, the appearance of pathology is associated with the development of testicular cancer, when the tumor grows and disrupts the integrity of the scrotal blood supply. [ 1 ]
Treatment options range from conservative therapy to surgery.[ 2 ]
Epidemiology
Hematocele due to trauma and other damage to the scrotum organs accounts for less than 1% of all similar cases involving other organs. The low prevalence of this pathology is due to the anatomical localization of the scrotum, the strength of the vessels and protein membrane, as well as the protective function of the cremasteric muscles, which quickly react when there is a risk of injury.
And, despite this, extensive hematocele poses a fairly large threat to health, since aggravating pathological processes can lead to the loss of the testicle, which will negatively affect fertility, can provoke the development of hypogonadism and will negatively affect the psychosocial plan. In addition, the production of antisperm antibodies can cause the formation of immunogenic infertility, adversely affecting the quality of seminal fluid.
Most often, hematocele is detected in patients aged 16-40 years. According to statistical information, traumatic injuries to the scrotum are the most common among all injuries to the urogenital tract in men. [ 3 ]
Hematocele is often unilateral (in almost 99% of cases), and the right testicle is affected more often than the left: experts attribute this to the peculiarities of the location of the right testicle relative to the pubis and the inner femoral surface.
According to the research results, sports and industrial injuries are the leading causes of hematocele (approximately 74% of cases), of which road traffic accidents account for about 13% of cases. Animal bites are the rarest causes.
Drug treatment is used at the first or second stage of the pathology. An indication for surgical intervention may be a hematocele, the size of which exceeds the volume of the intact testicle more than three times, as well as a tense form of hematocele, provoking severe pain syndrome.
Causes hematoceles
The most common cause of hematocele is considered to be closed or blunt trauma to the genitals – in particular, the scrotum area. The trauma may be the result of a direct blow, a bruise as a result of an unsuccessful landing, domestic or industrial damage, an accident, etc.
Less often, the pathology is provoked by various medical manipulations and procedures:
- unsuccessful puncture of a venous or arterial vessel;
- damage to the vascular wall during the treatment of hydrocele - dropsy of the testicle, which leads to the appearance of blood elements in the exudative fluid;
- complications during testicular biopsy (for example, with chronic orchitis, etc.).
In extremely rare (almost isolated) cases, hematocele is the result of such a systemic pathology as hemorrhagic diathesis – we are talking about a specific blood disease with a tendency to excessive bleeding. In some patients, it is not possible to establish the cause of hematocele at all. [ 4 ]
Risk factors
Our health is influenced by many factors, and those that lead to the development of diseases and injuries are called risk factors: they often coexist and interact with each other, leading to one problem or another. For example, playing certain sports increases the risk of developing hematocele. These sports include:
- cycling, motorsports;
- horse riding;
- hockey, football;
- wrestling, kickboxing and other martial arts;
- rugby;
- golf;
- artistic gymnastics.
These are the sports that are most often associated with blunt trauma to the genitals. To prevent injury, it is important to remember to use special protective equipment.
Other factors may include:
- surgical, urological manipulations in the scrotum area;
- animal bites (there is also a risk of infection);
- domestic and industrial injuries.
Pathogenesis
Hematocele is formed:
- as a result of traumatic injury to the scrotum;
- as a result of a puncture of a blood vessel during a puncture of the tunica vaginalis of the testicle (for example, during a procedure to remove fluid contents in patients with hydrocele);
- when collecting material for a testicular biopsy in patients with chronic hemorrhagic inflammation of the vaginal membrane, which is accompanied by hemorrhage into the intermembranous space and the formation of granulation tissue with a dense capillary network on the inner part of the membrane.
The development of hematocele is based on damage to the integrity of a blood vessel without an open wound surface. Against the background of increased pressure, blood flows out and accumulates between the membranes, in the cavity. Partially leaked blood seeps through the surrounding tissues, causing a characteristic change in the color of the skin of the scrotum. Under the influence of the breakdown of red blood cells, the color range may change.
Over time, small hematoceles may dissolve or undergo a series of successive pathological changes. During the opening of a “fresh” hematocele, no change in the color or structure of the blood is observed (rarely, the blood becomes thicker under the influence of platelets). [ 5 ]
When old hematoceles are opened, a change in the color and thickness of the blood is observed, which becomes dark burgundy or even black. If an infection occurs, suppuration begins, and the cavity between the membranes is filled with purulent exudate.
With the development of atrophic processes, tissue degeneration occurs, with deterioration of blood circulation and a decrease in the size of the affected testicle.
Symptoms hematoceles
The clinical picture of hematocele generally depends on the period of the disease. At the initial stage, coagulated blood can be found in the tissues, and at later stages, clots of old, "old" blood are detected. Over time, such blood clots undergo structuring: together with an increase in the volume of connective tissue, this entails a deterioration in the blood supply to the testicle. If medical assistance is not provided, the process leads to atrophy.
Hematocele may be accompanied by a large number of symptoms, which may appear separately or in combination with each other.
The most common symptoms are:
- The appearance of pain in the area of hemetocele development. Pain often occurs gradually, as pressure on the surrounding tissues increases. Depending on the presence of an inflammatory process, the nature of the pain can range from sharp stabbing to mild aching. Pain may radiate to the groin area, the leg on the affected side, and to the pelvic organs.
- Change in skin color. The skin in the scrotum area on the affected side changes color, from reddish to purple. Often, the color intensity reflects the stage of the pathological process: thus, at the initial stage, a barely noticeable redness may be observed, which gradually intensifies and changes. If blood circulation is impaired, a bluish tint appears.
- An increase in the size of the scrotum, associated with swelling, accumulation of blood between the tissues. The size often increases slightly, and pronounced swelling indicates impaired blood circulation.
- Erectile dysfunction caused by pain and other pathological symptoms.
- Impaired fertility associated with changes in the nature of seminal fluid due to a long-standing hemetocele focus and established chronic pathological processes.
- Itching that occurs against the background of swelling and/or an infectious process.
Systemic symptoms may include:
- increased body temperature (if an infectious and inflammatory process occurs);
- deterioration of general well-being, decreased performance and tolerance to physical activity (with the development of intoxication).
As complications develop, additional pathological signs may be detected:
- fever, increase in temperature;
- signs of intoxication, anemia;
- change in testicular density, decrease or increase in size;
- apathy, general weakness, irritability, sleep disturbance;
- decreased sexual desire caused both directly by the pathology and by a background decrease in testosterone production;
- impaired fertility, infertility.
Typical early signs of hematocele may include:
- swelling of the scrotum area;
- prolapse of the scrotum;
- change in the color of the skin in the scrotal area to reddish and purple;
- pain syndrome in the testicular area.
Temperature readings usually remain within normal limits (unless an infectious process is present). If medical assistance is not provided, complications such as orchitis, epididymitis, etc. often develop.
Any of the above symptoms is considered a more than compelling reason for an urgent visit to a specialist - a urologist. It is important to consult a doctor in a timely manner not only if hematocele develops after injuries and surgical manipulations, but also without any apparent reason. Hematocele of unknown origin may be the result of an increasing neoplastic process. In particular, a testicular tumor may be the "culprit". [ 6 ]
Stages
The scale and nature of pathological changes varies, depending on the term of existence of hematocele.
At the initial stage, coagulated blood is detected, after some time - brownish "old" blood and a substance of a mushy consistency. Even later, the formation of blood clots with pronounced connective tissue proliferation is noted, and in some patients - with the appearance of plaques of a calcareous, cartilaginous or bone nature.
At a late stage, as a result of pressure on surrounding tissues and circulatory disorders in the testicle, atrophic degenerative processes may develop, characterized by a gradual decrease in the size of the testicle. This, in turn, entails a permanent reduction in the production of the male hormone testosterone and seminal fluid.
Forms
Classification of hematoceles is carried out with the purpose of dividing them into groups, selecting treatment tactics, determining the advisability of performing surgery, and assessing the prognosis of the pathology.
Practicing physicians point out the following types of hematocele:
- By localization - in the lungs, in the tissues of the scrotum, in the pelvic area (pelvic, parametric hematocele).
- By the nature of damaged vessels (small-vessel, large-vessel hematocele).
In addition, hematocele is distinguished by the complexity of the pathology:
- mild form (insignificant damage that does not require treatment);
- moderate form (the lesion is of significant size, requires conservative therapy);
- severe form (large lesion, characterized by significant dimensions, occurring with possible complications, requiring surgical intervention).
In general, scrotal injuries are divided into the following degrees of severity:
- Grade I – hematocele without visible damage to the testicle and its membranes.
- Grade II – hematocele with rupture of the protein membrane without visible damage to the testicle.
- Grade III – rupture of the protein membrane with loss of parenchyma less than half of the volume.
- Grade IV – rupture of the parenchyma with loss of more than half of the volume.
Complications and consequences
Posttraumatic hematocele can lead to the development of temporary infertility, which sometimes lasts up to several months. Subsequently, sperm production is most often restored, but the worst development of events is not excluded. Experts suggest that severe trauma can even lead to inhibition of testosterone production and its active transformation into estradiol, which can entail not only a disorder in the production of seminal secretion, but also a deterioration in potency.
Another possible complication of hematocele is an infectious process affecting the testicular tissue. The inflammatory reaction can spread to surrounding tissues: appendages, spermatic cord, etc.
Inflammatory process of the epididymis (epididymitis) is accompanied by pronounced swelling and pain in the scrotum. Ultrasound shows an increase in the epididymis, hypoechogenicity (against the background of hematocele, echogenicity increases). If untreated, epididymitis is complicated by orchitis and abscess.
Inflammatory reaction in the testicular tissue (orchitis) occurs as a result of trauma or hematocele, the infection can spread retrogradely from the prostate gland or bladder through the vas deferens. Inflammation usually begins in the epididymis, but soon moves directly to the testicle, so the pathology is often diagnosed as orchiepididymitis. Isolated orchitis is less common and occurs as a result of hematogenous infection. [ 7 ]
On ultrasound, orchitis looks like enlarged testicles with preserved homogeneity of the internal structure, or there is a blurred, unclear parenchymatous pattern against the background of the normal configuration of the organ. With a strongly expressed inflammatory process, due to edema, the parenchyma may have a homogeneously reduced echo density, or non-uniform density. Acute orchitis on Doppler ultrasound demonstrates increased blood circulation.
In the presence of atrophic changes, the echo density of the testicle remains reduced, and a weakening of blood flow is recorded.
Acute inflammation can provoke the development of an abscess.
Diagnostics hematoceles
When diagnosing hematocele, they most often mean a pathological accumulation of blood between the visceral and parietal layers, localized near the vaginal membrane of the testicle. In addition, blood may also be present in the scrotum. In the first example, they talk about intravaginal pathology, and in the second - about extravaginal.
Blood accumulation – testicular hematocele – requires careful differential diagnostics, especially if it is not possible to determine the causes of the pathology. Even with minimal suspicion of a tumor process or the slightest doubt, the doctor should refer the patient to narrow specialists for further detailed diagnostics. The sooner the cause of the disease or tumor process is identified, the more favorable the prognosis will be and the easier the treatment will be.
Quick diagnostic appointments will relieve a man from unnecessary nervous and mental stress caused by a long wait.
Currently, the most optimal method for diagnosing hematocele is ultrasound. This procedure is non-invasive, fast and painless, helps to assess structural and functional changes, and can be performed several times without any harm to the patient. However, any examination is performed only after a thorough collection of anamnesis, assessment of the symptoms of the disease, examination and palpation of the area of the pathological focus.
For ultrasound diagnostics, sensors with an emitted frequency of at least 5-10 MHz are used. If the scrotum area is sharply painful (with orchitis, epididymitis), then local superficial anesthesia may be required. Vascular studies are performed using color Doppler mapping. Power Doppler is used to assess the condition of the testicular parenchyma.
Echography is prescribed for scrotal injuries, any increase in size and configuration disorders, local temperature increase, skin color change, pain, detection of atypical palpable formations, suspected hematocele and other similar pathologies. Additionally, ultrasound of blood flow through the vessels of the testicle and its parenchyma may be prescribed.
On ultrasound, mature testicles normally have a smooth rounded surface, a homogeneous fine-grained structure with average echo density. The mediastinum is quite clearly seen as a line of high echogenicity in the sagittal plane. The epididymis is better defined by longitudinal scanning: it is located along the posterior border and has a club-shaped form. It has a head, body and tail, without clearly defined anatomical boundaries. The body of the epididymis is flattened, and its tail flows into the vas deferens. Ultrasound examination helps to detect tumor processes, inflammatory reactions, hydro and hematocele. A healthy testicle and epididymis are surrounded by a protein and serous membrane. The protein membrane is represented by a thin continuous strip with a high-intensity reflected echo signal. The physiological fluid in the scrotum has a volume of 1-2 ml and has the appearance of an echo-negative bracket measuring from 1 to 3 mm in the area of the upper testicular pole. [ 8 ]
In case of asymmetrical damage, diagnostics begin with the healthy side as a reference point. The scrotum area is necessarily examined from the front and back.
Usually, an ultrasound scan is enough to establish a diagnosis and prescribe appropriate therapy. Only in some cases, computer and magnetic resonance imaging, Doppler scanning of the testicular vessels are used to clarify certain points.
In cases of severe damage that causes a hematocele, it is often necessary to refer the patient for surgery to revise the testicle.
Tests
General clinical laboratory tests are not mandatory for hematocele. But they allow the doctor to diagnose concomitant pathology in the body and monitor the course of treatment.
It is possible to take the following material for analysis:
- blood;
- urine;
- ejaculate;
- urethral smear.
Information obtained during general clinical diagnostics often does not indicate any specific disease, but shows the state of the body as a whole and helps to narrow the diagnostic search.
In case of hematocele, the following laboratory tests may be performed:
- general urine analysis;
- examination of secretions from the genitourinary organs;
- microscopy of secretions from the genitourinary organs;
- general clinical analysis of prostate secretion;
- spermogram (semen analysis);
- blood test (hemoglobin content, quantity and quality of red blood cells and white blood cells, erythrocyte sedimentation rate, assessment of blood clotting quality, etc.).
To assess the condition of the genitourinary system, the following indicators are considered:
- physical properties of urine fluid (color, density, transparency, odor);
- the presence of protein in the urine (as well as urobilin, hemoglobin, glucose, acetone);
- sediment study.
Instrumental diagnostics
In traumatic injuries that require urgent surgery (for example, testicular rupture, extensive hematoma), early diagnosis helps prevent permanent complications such as ischemic atrophy and infectious processes.
Scrotal injury shows signs of hematocele on ultrasound imaging – sometimes in the form of post-traumatic epididymitis, epididymal hematoma, infarction or hematoma of the testicle, hyperemia of the testicle, its swelling and rupture. If there is a rupture, then a “broken” line, testicular fragmentation, disruption of configuration and echo density are shown on ultrasound imaging. In case of extensive hemorrhage, color Doppler mapping is required to assess the state of the vascular network and determine the tactics of surgical intervention.
In echography of hematocele, heterogeneity of the fluid is noted, and a large number of small moving echogenic structures are determined in the lumen.
Ultrasound examination of scrotal injuries is prescribed to characterize the damage, to confirm or exclude a testicular rupture (which subsequently helps to assess the prognosis of the pathology), to distinguish hematocele from a soft tissue hematoma, to monitor the dynamics of the patient's recovery after surgery, or to determine indications for drug treatment. [ 9 ]
Differential diagnosis
Hematocele should be distinguished from other benign formations (cysts, hydrocele, spermatocele, tuberculous or non-tuberculous epididymo-orchitis, varicocele, inguinal hernia, syphilitic gumma) and from malignant processes (carcinoma, lymphoma).
Epididymal cysts are found mainly in middle-aged patients. Such cysts are multiple and often bilateral. Externally, they are defined as fluctuating elements that can be palpated in the back of the testicle, separately from the testicle itself. It happens that the cyst shifts to the front: in such patients, it is palpated in front of the testicle.
Spermatocele has much in common with cystic formations. It is characterized by its location above the testicles in the area of the vaginal membrane.
Hydrocele is formed by the accumulation of liquid contents in the cavity of the vaginal membrane. Such a disease can be primary or secondary: primary pathology is most often idiopathic (without an obvious cause), and secondary pathology usually becomes a consequence of tumor processes, injuries and infectious diseases. The clinical picture of hydrocele is as follows: the edematous zone around the testicle is palpated, in some cases the testicle is not palpated. When the testicle is transilluminated, light passes through.
Hematocele is an accumulation of blood in the cavity of the vaginal membrane. The pathology may be the result of trauma or a complication of testicular carcinoma. Symptomatically, hematocele is similar to hydrocele, but when the testicle is illuminated, light does not pass through. If left untreated, the hematocele shrinks and becomes denser: at this stage, the disease should be distinguished from testicular carcinoma.
The tuberculous form of epididymoorchitis is relatively rare. The main manifestations of this pathology are the formation of a dense, not very tense edema of irregular configuration, thickening of the vas deferens. The movement of the testicles in the scrotum is often limited.
In the non-tuberculous form, generalized edema of the appendage and testicle occurs. But regardless of the presence of pain syndrome, such a disease has many clinical signs of a tumor process, which also requires differentiation.
Varicocele is also accompanied by an enlargement of the testicle, but its cause is the expansion of the grape-like branches of the internal spermatic vein or directly of the spermatic venous vessel. Varicocele is better diagnosed when the patient is in an upright position. If the development of such a process occurs too rapidly, then one may think about the existence of renal cell carcinoma. [ 10 ]
An inguinal hernia differs from a hematocele by the impossibility of palpating the upper border and a positive cough impulse test.
As for malignant tumors, they are most often found in men aged 20 to 40 years. The most common development of such processes occurs from germ cells, resulting in the formation of teratoma or seminoma. Tumors are compacted edema, covering all parts of the testicle. Many patients complain of severe pain.
In old age, lymphoma is more common.
An enlarged, painful, and reddened scrotum may also indicate damage to other organs, even those located relatively far from the external genitalia. For example, blood may flow into the scrotum as a result of abdominal trauma, and in newborns, as a result of hemorrhage into the adrenal gland.
If a man seeks medical help with signs of hematocele, the doctor should carefully collect anamnesis and perform all stages of local and general examination. This will help to confidently make the correct clinical diagnosis.
Treatment hematoceles
In case of a small hematocele, treatment may be limited to conservative measures:
- applying ice packs, dry ice to the scrotum area;
- taking analgesics, anti-inflammatory drugs;
- ensuring absolute rest for several days, complete abstinence from physical activity for the entire period of treatment.
If there is a risk of secondary infection, antibiotic therapy is prescribed. After the patient's condition has normalized and acute signs of hematocele have disappeared, physiotherapy procedures can be used, the action of which is aimed at resolving the problematic accumulation of blood (magnetic therapy, ultra-high-frequency therapy).
If the conservative method is ineffective, surgical treatment is used. The type of surgical intervention and the technique used to perform it are selected depending on the size of the hematoma, the patient's age, and the presence of complications. [ 11 ]
Conservative therapy consists of the following measures:
- use of a suspensory;
- applying cold to the scrotum;
- taking analgesics and nonsteroidal anti-inflammatory drugs;
- strict bed rest for at least two days;
- prescribing antibiotic therapy if there is a suspicion of the development of epididymitis or an infectious process in the genitourinary system;
- If conservative treatment is ineffective, a repeat ultrasound and Doppler examination is required.
Scrotal revision is prescribed:
- if it is impossible to determine the diagnosis;
- if there are symptoms of testicular damage;
- when the protein shell is destroyed;
- with an expanding hematocele focus, or with the development of massive bleeding;
- in the absence of blood flow according to ultrasound information with color Doppler mapping.
First aid for hematocele consists of the following actions:
- Apply cold to the damaged area (ice wrapped in a towel to prevent frostbite) to constrict blood vessels and slow down the inflammatory process. Apply a cold compress every 3-4 hours, holding it for about 15-20 minutes.
- The patient is given an analgesic (Ibuprofen, Analgin, Nimesil).
- Provide the victim with maximum rest in a horizontal position.
A man with a hematocele must be examined by a doctor. After diagnosis, he will prescribe the necessary treatment measures. [ 12 ]
Medicines
Medicines are prescribed in accordance with the cause of the development of hematocele, which is determined by a specialist during diagnosis.
In case of infectious nature of pathology, antibacterial or antiviral medications are used taking into account the resistance of microorganisms. If an infectious disease transmitted sexually is detected, then treatment is prescribed depending on the pathological pathogen. The non-specific nature of hematocele requires the use of antibiotics of a wide spectrum of activity, with a selection from several groups.
Ibuprofen |
Non-steroidal anti-inflammatory drug, relieves pain and slows down the development of the inflammatory process. Tablets are taken orally whole, with water, 1-2 tablets no more than three times a day. It is not advisable to take the drug for more than five days in a row, due to its irritating effect on the mucous membrane of the digestive tract. |
Nimesulide |
An anti-inflammatory and analgesic drug intended for oral administration (the treatment period with Nimesulide is no more than 15 days). As a rule, 100 mg of the drug is taken twice a day after meals. Possible side effects: abdominal pain, nausea, diarrhea, dizziness. |
Actovegin |
A drug that stimulates tissue metabolism, improves tissue trophism and regeneration. Taken orally before meals - on average 2 tablets three times a day. Treatment can be long-term - up to several months. Possible side effects: allergic reactions. |
Dipyridamole |
Antiplatelet agent, antithrombotic drug used at the stage of recovery after injury. If there is a tendency to bleeding (hemorrhagic diathesis), the drug is not prescribed. Take orally between meals, without chewing, with water, 1-2 tablets three times a day. The duration of therapy is determined individually (from several weeks to six months). Possible side effects: allergy, headache, tremor, tachycardia, abdominal discomfort. |
Troxerutin |
Angioprotective, capillary stabilizing drug. Taken orally after meals, in an average dose of 2 capsules per day. Treatment can be long-term. Possible side effects: allergic reactions, headache, sleep disorders, abdominal pain, nausea. |
In general, conservative treatment includes:
- elimination of symptoms (most often the patient complains of severe pain, which is quite effectively “relieved” by analgesics);
- elimination of the immediate cause of the violation (if possible);
- creation of conditions conducive to therapy (bed rest, movement restrictions, application of a bandage or suspensory, use of angioprotectors);
- application of physiotherapy.
Physiotherapy treatment
Physiotherapy can be an effective adjunctive treatment for hematocele, along with drug therapy, and also a means of accelerating the body's recovery after surgery.
Today, medicine offers a lot of procedures and medications that can be used for hematocele. However, many medications put a fairly strong load on the body, causing the development of side effects. It is also possible that the patient has contraindications to the use of certain medications. In addition, the effect of medications may not be effective enough, since the active substance cannot get to the affected tissues in the required amount through the bloodstream. If you combine conservative treatment with physiotherapy, then, thanks to an integrated approach, you can achieve a significant improvement in the well-being and quality of life of a man, with the minimum possible drug load on the body. Physiotherapeutic procedures improve blood circulation, lymph circulation, and accelerate metabolism in the area of impact.
The effect of physiotherapy is based on the absorption of physical energy by the body's tissues and its transformation into biological reactions. It is optimal to undergo a course of electrical, radiation or magnetic therapy in order to achieve the necessary success. If the patient receives a drug simultaneously with the procedure, it accumulates mainly in the pathological focus, getting directly to the diseased organ.
During the recovery period after hematocele (including after surgery), the patient is prescribed phonophoresis of therapeutic mud, electrotherapy with pulsed currents, and intra-tissue magnetic-laser-electrophoresis of enzyme preparations.
Herbal treatment
To speed up the healing process of hematocele, people often use folk methods. We present to your attention the most popular recipes:
- A fresh white cabbage leaf is beaten with a meat hammer, applied to the scrotum area and held for at least 1.5-2 hours. The leaf can be fixed with compression underwear.
- Arnica infusion is used for internal use and for compresses. The infusion is prepared as follows: one teaspoon of flowers is poured with hot water and infused for two hours. Instead of flowers, the root of the plant can also be used. The remedy is used for cool compresses, and also taken orally 50 ml three or four times a day, between meals.
- A fresh plantain leaf is washed, lightly kneaded with fingers and applied to the damaged area (scrotum), at night. Additionally, you can take a pharmacy plantain tincture orally (according to the instructions).
- A compress of aloe leaves and honey is prepared as follows: aloe leaves are ground or minced, mixed with honey. Use for compresses at night, once a day.
- Fresh cucumbers are cut into circles and applied to the scrotum, fixed with a bandage or compression underwear. The minimum retention of the product on the affected area is 30 minutes. The procedure can be repeated several times a day.
- Fresh banana peels are applied to the hematocele site, with the inner side against the skin. This remedy helps relieve pain and speed up the resorption of blood accumulation.
In case of small hematocele, folk methods help no worse than modern medicines, and without any side effects. Most of the proposed recipes are quite simple and accessible.
Surgical treatment
The minimum volume of hematocele, in which surgical intervention is indicated, has not been determined by specialists. But most surgeons believe that if the size of the pathological focus does not exceed 1/3 of the diametrical size of the testicle, then a wait-and-see tactic with drug management of the pathology can be used. There is no need for surgical intervention if there is a small
Hematocele without a picture of testicular rupture. The combination of hematocele (regardless of its size) with intratesticular hematoma is always regarded as an indication of testicular rupture, even if there are no echographic signs of rupture.
However, there is evidence that echography is not informative enough. For example, testicular rupture was accurately detected by ultrasound scanning only in 50% of cases. To avoid errors, experts recommend early surgical intervention if a testicular rupture is suspected.
The operation is prescribed for a large volume of spilled blood, with the development of a purulent process or calcification. The intervention is best performed as early as possible: the less time has passed since the development of hematocele, the greater the chances of preserving the testicle itself and its function. In chronic cases, the surgeon has to perform an orchiectomy - an operation to remove the testicle.
Surgical manipulations may be as follows:
- stopping bleeding, removing spilled blood;
- removal of necrotic areas;
- suturing of the tissues of the shell;
- returning the testicle back into the scrotum;
- correction of torsion, release of incarceration;
- suturing of tissues with compromised integrity, damaged vessels;
- in some cases – partial or complete removal of the testicle.
After surgery, the man may be hospitalized for 5 to 8 days, depending on the complexity of the disorder and the scope of the surgery. Drains are removed after a few days. The patient is discharged home with the condition of a mandatory follow-up visit to a specialist for examination and consultation.
Prevention
Hematocele is a serious pathology that requires urgent medical attention and comprehensive diagnostics. Remote consequences of undiagnosed hematocele may include abscesses, other inflammatory and atrophic processes, erectile dysfunction, etc.
A violation can be prevented if:
- protect the genitals when participating in dangerous sports;
- to raise the level of sexual culture and sex education;
- handle pets with care;
- avoid dangerous sexual positions;
- trust the performance of therapeutic and surgical procedures only to qualified, experienced specialists.
It is equally important to follow simple preventive rules that will help keep your genitals and circulatory system healthy:
- be physically active, avoid physical inactivity;
- eat right, include in your daily diet foods rich in minerals, vitamins, beneficial microelements, and proteins;
- treat any infectious and inflammatory pathologies in a timely manner;
- give up smoking and drinking alcohol;
- have regular sexual intercourse with a trusted partner, avoid unprotected sex and withdrawal;
- Avoid overheating or overcooling the body.
If you follow all the suggested recommendations, you can minimize the risk of developing hematocele and other genitourinary system lesions. But we must not forget that with any suspicion of pathology, it is important to visit a doctor as soon as possible. Early diagnosis and competent treatment will help to avoid complications.
Forecast
The prognosis of the disease as a whole and completely depends on the duration of its course. At the initial stage, the doctor determines only a blood clot, and at a late stage, the presence of seals is noted, which over time become structured. In combination with an increasing volume of tissue, the pathological process entails a deterioration in the blood supply to the testicle, which can subsequently lead to its complete atrophy. [ 13 ]
Before starting treatment of hematocele, it is important to understand that in some patients the blood accumulation may disappear on its own, without any intervention. However, this does not always happen. Many men have to undergo a whole range of measures, including drug therapy. An ice pack is applied to the scrotum, analgesics and anti-inflammatory drugs are prescribed. The patient is prescribed a gentle bed rest, complete rest with the maximum possible limitation of motor activity. In the case of a pronounced hematocele, a puncture is performed, which is often ineffective, and even worse - it can provoke repeated bleeding or the development of a purulent process. If it is not possible to remove the blood that has spilled into the cavity, then surgical intervention is used to avoid testicular atrophy. With proper and timely treatment, the prognosis is considered favorable.

