Medical expert of the article
New publications
Hypokinesia of the heart
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
In some patients, an electrocardiogram reveals a condition called cardiac hypokinesia - for most patients, this term is incomprehensible and raises a lot of questions. If we consider this concept literally, it means: "hypo - little, kinesis - movement", that is, low mobility - in this case, of the heart muscle. In many people, this pathology is associated with changes in the myocardium after a heart attack. In this case, the passage of the contractile wave deteriorates in the scarring area, which entails the appearance of hypokinesia.
Epidemiology
Absolutely all patients who have had a myocardial infarction subsequently show cardiac hypokinesia on the cardiogram. As a rule, this happens approximately two months after the infarction.
Hypokinesia can be detected with equal frequency in both male and female patients, mainly after 50 years of age.
Causes areas of cardiac hypokinesia
The causes of hypokinesia may be different. This condition is almost never independent: as a rule, it is a consequence of other problems with the heart.
The main reasons can be considered:
- atherosclerosis of the coronary vessels, with subsequent development of myocardial ischemia;
- inflammatory process, myocarditis;
- myocardial infarction, acute heart failure.
- The listed reasons are considered the most common. Among the relatively rare reasons, the following can be distinguished:
- exposure to radiation;
- cardiac sarcoidosis;
- hemochromatosis;
- systemic scleroderma.
Doctors conclude that due to the complexity of the disease and the presence of many reasons for its occurrence, it is quite difficult to focus on any one factor. Therefore, doctors focus their treatment on slowing down the further spread of the process.
Risk factors
Risk factors for the development of cardiac hypokinesia include:
- disorder of fat metabolism, high cholesterol in the blood;
- long-term high blood pressure, hypertension;
- long-term smoking, including passive smoking;
- overweight;
- unfavorable heredity, genetic abnormalities (for example, narrowing of the blood vessels of the heart);
- frequent and deep stress, hormonal disorders;
- viral, microbial, fungal infections (rubella, meningitis, aspergillosis, etc.);
- allergic processes;
- systemic inflammatory processes;
- chronic intoxication, including alcohol or drug intoxication.
Pathogenesis
In case of stenosis, ischemia or metabolic changes in the myocardium, increasing dystrophic, atrophic changes or death of muscle fibers occur. Necrotic foci or micro scars remain in the damaged areas.
Damage to receptors leads to decreased sensitivity of cardiac tissue to oxygen, which only worsens the state of hypokinesia.
Since there are several pathogenetic variants of the development of the pathological process, several varieties of cardiac hypokinesia can be distinguished. Thus, ischemic hypokinesia occurs with prolonged insufficient blood circulation: in this case, the myocardium is almost completely affected. Postnecrotic hypokinesia is formed in the area of a previous infarction. In addition, a mixed variant of cardiac hypokinesia development is possible.
Symptoms areas of cardiac hypokinesia
Since cardiac hypokinesia is not an independent pathology, but is considered only a sign of other cardiac problems, its symptoms are usually associated with the underlying pathology. If the elasticity of the vessels is not impaired, the conduction system is not damaged, then hypokinesia can occur without any obvious symptoms. Symptoms may also be absent if the degree of cardiac hypokinesia is small and superficial.
In other situations, the first signs of cardiac hypokinesia may occur:
- difficulty breathing, especially during physical exertion;
- unexplained periodic coughing fits (so-called "cardiac bronchitis");
- heart rhythm disturbances;
- strong heartbeat felt by the patient;
- a feeling of constant or severe fatigue;
- "cardiac" edema;
- periodic dizziness;
- chest pain.
Forms
Differences in the intensity and location of hypokinesia allow us to identify individual types of pathological conditions:
- focal hypokinesia - for example, after a heart attack or a localized inflammatory process;
- diffuse hypokinesia, in which all muscle fibers of the heart are uniformly affected, without the definition of clear affected areas.
Hypokinesia of the left ventricle of the heart
With left ventricular hypokinesia, there are no characteristic symptoms. There is only a clinical picture of the underlying cardiac pathology. In most patients, the compensatory period can last quite a long time, for several years, and the patient learns about the state of hypokinesia during routine diagnostic procedures.
Left ventricular hypokinesia can be suspected based on the following signs:
- constant feeling of weakness, fatigue;
- cardiac arrhythmia, ventricular tachycardia, arrhythmia;
- swelling of the extremities in the evenings;
- dry cough and difficulty breathing;
- cyanosis of the nasolabial triangle, finger phalanges;
- pain in the heart area;
- dizziness.
At the first signs of deterioration in health, you should immediately contact a doctor for diagnostic and treatment procedures.
 [ 14 ]
[ 14 ]
Hypokinesia of the cardiac apex
It can be said about such localization of hypokinesia that it is relatively rare. Postnecrotic hypokinesia occurs after an infarction, noted in leads V4, or from V3 to V5, as well as Anterior according to Neb.
The electrocardiogram may show a QS pattern in lead V4, indicating transmural myocardial infarction.
Postnecrotic hypokinesia after myocardial infarction at the apex of the heart is most often provoked by occlusion of the terminal branches of the left anterior descending artery.
Hypokinesia of the interventricular septum of the heart
This type of hypokinesia is most often associated with a congenital defect of the interventricular septum, when there is a hole in the septum separating the left ventricular and right ventricular cavities. Pathological shunting of blood occurs through it. Such an anomaly is more common than others among all congenital heart defects (frequency - up to 25%).
The interventricular septum, together with the ventricular walls, ensures the contractile and relaxing movements of the heart.
Symptoms of interventricular septal damage depend on the degree of the defect and the severity of hypokinesia.
Diffuse myocardial hypokinesia
In diffuse hypokinesia, the motor ability of all myocardial fibers suffers. As a rule, this process occurs gradually:
- angina episodes occur more frequently and become more severe;
- loss of working capacity;
- arrhythmia or aneurysm appears.
Symptoms characteristic of heart failure are observed. The severity of these symptoms depends on the stage of the pathology.
If measures are not taken to stop the process, myocardial damage can lead to severe disability and death.
Complications and consequences
The condition of cardiac hypokinesia cannot be cured completely: the goal of doctors is to stop further damage to muscle fibers. However, even timely treatment measures do not guarantee complete prevention of unpleasant consequences that may occur over time.
The most common consequences of cardiac hypokinesia are:
- chronic course of cardiac failure;
- formation of cardiac aneurysm;
- heart rhythm disturbances;
- acquired form of heart defect;
- thromboembolic complications;
- development of chronic fatigue syndrome.
For most patients, the occurrence of complications entitles them to disability benefits. To do this, they must provide medical evidence of the problem: most often, the results of electrocardiography, dynamic echocardiography, scintigraphy, as well as consultative conclusions from doctors of other specialties are required.
Diagnostics areas of cardiac hypokinesia
Cardiac hypokinesia cannot be determined by routine examination, even if the anamnesis indicates the presence of provoking factors. To diagnose cardiac hypokinesia and pathologies associated with this condition, a number of additional studies must be carried out.
Blood and urine tests will not be able to provide any necessary information regarding the development of cardiac hypokinesia. But in some cases, tests can detect other pathologies in the body that could be the primary cause of hypokinesia. For example, an inflammatory process in the heart muscle will be reflected in the blood picture by signs of inflammation, and atherosclerosis - by high cholesterol. Of course, such information will not directly indicate the presence of cardiac hypokinesia, but will only become an auxiliary type of diagnosis.
General tests are always prescribed to all patients before a treatment regimen is prescribed in order to take into account possible contraindications and avoid negative consequences.
Instrumental diagnostics are prescribed when there is a suspicion of any cardiac pathologies, including cardiac hypokinesia. The following types of studies are considered the most indicative:
- Chest X-ray – can visualize changes in the shadow of the heart and aorta, as well as other abnormalities.
- Electrocardiography is the main method that allows determining cardiac hypokinesia.
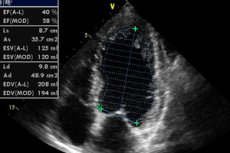
- Ultrasound examination, echocardiography – helps to accurately examine the heart and its internal structure on the monitor.
- Exercise testing and stress echocardiography – provides information about myocardial endurance and response to physical exercise.
- Daily monitoring of cardiac activity is used primarily for cardiac arrhythmia and allows you to track the work of the heart at different times of the day and in different conditions.
- MRI is used to clarify the diagnosis and for more detailed visualization of the intracardiac structure.
Differential diagnosis
Differential diagnostics usually relates to the underlying cause of cardiac hypokinesia and is built by excluding other chronic heart diseases. First of all, it is necessary to exclude atherosclerotic and myocardial forms of cardiosclerosis, chronic myocarditis, cardiomyopathy, and the so-called "heart attack on the legs". It is not difficult to detect hypokinesia during diagnostics: it is much more difficult to find the underlying cause of this disorder.
Who to contact?
Treatment areas of cardiac hypokinesia
At present, it is not possible to completely restore muscle tissue and eliminate cardiac hypokinesia. It is important not to let the process worsen and prevent complications from developing.
Treatment of cardiac hypokinesia is performed by a cardiologist. The main goals of therapy are as follows:
- eliminate the underlying cause of hypokinesia;
- eliminate factors that may aggravate the problem in the future;
- support cardiac activity;
- prevent the development of complications;
- to improve the patient's quality of life if possible.
Treatment of patients with cardiac hypokinesia is carried out taking into account the degree of organ damage, as well as the existing symptoms.
Most often, medications of the following groups are prescribed:
- ACE inhibitors;
- glycoside cardiotonic agents;
- beta-adrenergic receptor blockers;
- aldosterone receptor blockers;
- diuretics.
Prescribing a treatment regimen based on the listed drugs allows you to stabilize cardiac activity and normalize the load on the heart muscle. All prescriptions are made exclusively by a cardiologist. Self-administration of medications is unacceptable.
Dosage and method of administration |
Side effects |
Special instructions |
|
Captopril |
Take 6.25-50 mg, up to 3 times a day, with a maximum daily dose of 150 mg. |
Dizziness, orthostatic decrease in blood pressure, changes in taste sensations. |
Captopril is an ACE inhibitor. It reduces the load on the myocardium and lowers blood pressure. |
Bisoprolol |
Take 1.25-10 mg once a day. |
Facial flushing (hot flashes), dizziness, bradycardia. |
Bisoprolol normalizes cardiac activity and reduces hypoxia. |
Furosemide |
Take from 20 to 500 mg per day on an empty stomach. |
Nausea, itching, temporary hearing loss, headache, depression, dry mouth. |
Furosemide eliminates swelling, reduces stress and facilitates heart function. |
Digoxin |
Take 0.125 mg up to 2 times a day, with a maximum daily dose of 0.25 mg. |
Dyspepsia, feeling of fatigue, headache, heart rhythm disturbances. |
Digoxin is a cardiac glycoside, but it is prescribed only for a short time - only to relieve symptoms. |
Spironolactone |
Take 25-50 mg per day, in the morning or afternoon, in 1-2 doses. |
Dyspepsia, drowsiness, lethargy, menstrual irregularities in women and erectile dysfunction in men. |
Spironolactone improves cardiac compensation. It is an aldosterone antagonist. |
In case of cardiac hypokinesia, vitamins are necessarily prescribed - especially useful are complex preparations with the obligatory content of B vitamins in the composition. The drugs of choice can be Angiovit, Centrum, Neurobeks, Vitrum Centuri: these vitamin supplements help improve nerve conduction and prevent complications from the cardiovascular system.
Physiotherapy treatment
In case of various disorders of the heart – for example, cardiosclerosis or myocardial hypokinesia, doctors recommend practicing balneotherapy, using carbon dioxide, sodium chloride, iodine-bromine baths. If there is no arrhythmia, then the use of hydrogen sulfide baths is also allowed.
To improve immune protection, inductothermy is used with an effect on the adrenal glands.
If the cause of hypokinesia is atherosclerosis (cardiosclerosis), the doctor may prescribe electrophoresis procedures with novocaine to the Zakharyin Ged zones. The duration of one session is from six to 15 minutes, the frequency of implementation is every day or every other day. One course may require from 8 to 20 sessions. Such procedures will improve blood circulation and the functional capacity of the myocardium.
In mild forms of hypokinesia, patients are recommended to undergo spa treatment.
Folk remedies
In case of cardiac hypokinesia, you cannot do without folk methods of treatment. There are many known remedies and medicinal plants that help alleviate the patient's condition, improving the functioning of the cardiovascular system. For example, it is worth paying attention to such recipes.
- Mix 1 tbsp. of crushed hawthorn rhizome and 1 tsp. of caraway seeds, brew in a thermos in 300 ml of boiling water overnight. In the morning, filter the infusion and drink throughout the day.
- A unique cocktail is prepared from two raw chicken proteins, 2 teaspoons of sour cream and 1 teaspoon of honey. This cocktail should be drunk every morning on an empty stomach.
- You should eat 150 g of fresh homemade cottage cheese every day.
- Juice or compote is prepared from rowan berries (both red and black). The plant's rhizome can also be used.
- Prepare a two-hour infusion of buckwheat flowers (1 tbsp. flowers per 500 ml of boiling water). Drink the infusion 100-150 ml 3-4 times a day.
- Every morning they eat one lemon, chopped in a meat grinder and mixed with honey and sugar.
In case of cardiac hypokinesia, berries and leaves of currants, blackberries, cranberries, as well as bird cherry flowers and garlic will be beneficial.
 [ 30 ], [ 31 ], [ 32 ], [ 33 ], [ 34 ], [ 35 ]
[ 30 ], [ 31 ], [ 32 ], [ 33 ], [ 34 ], [ 35 ]
Herbal treatment
- Prepare a mixture of crushed herbs: 1 tbsp. yarrow, one and a half spoons each of hawthorn, mistletoe and periwinkle leaves. Pour 1 tbsp. of the resulting mixture into 300 ml of boiling water, leave for about an hour. Drink the resulting infusion throughout the day.
- Prepare a herbal mixture of 20 g lemon balm, 10 g lily of the valley, 30 g cinquefoil and the same amount of rue. Pour 200 ml boiling water over one tablespoon of the resulting mixture and filter after an hour. Drink 1 tablespoon three times a day before meals.
More complex herbal mixtures can also be used to strengthen the heart. The ingredients usually used are sage, peppermint, betony, clover, calendula, chicory flowers, lingonberry leaves, oregano, and sweet clover.
Depending on the indications, after consulting a doctor, infusions based on valerian rhizome and motherwort are used - such drugs are especially relevant in the presence of spasms and cardiac neurosis.
Homeopathy
There are reviews about the positive impact of homeopathic preparations on the well-being of patients with cardiac hypokinesia. What preparations are we talking about and when can they be taken?
- Arnica 3x, 3 – for overload of the heart muscle;
- Aurum - if hypokinesia is caused by hypertension or atherosclerosis;
- Barite carbonica in dilutions of 3, 6, 12 – if cardiac hypokinesia is caused by age-related cardiosclerosis;
- Phosphorus 6, 12 – for hypokinesia caused by myocardial dystrophy;
- Calcarea arsenicosa 3, 6 - with hypokinesia due to cardiosclerosis;
- Graphite 6, 12 – for cardiac muscle dystrophy;
- Krategus 0.2x – for arrhythmia against the background of cardiac hypokinesia;
- Adonis 0, 2x – for heart rhythm disturbances, shortness of breath and edema;
- Ammonicum carbonicum 6 – for cardiac hypokinesia, with symptoms such as cyanosis of the nasolabial triangle, cough and shortness of breath during physical exertion.
Homeopathic remedies are used along with drug therapy, as an auxiliary type of treatment. These drugs are harmless and quite effective if correctly selected by a qualified homeopathic doctor.
Surgical treatment
Surgical intervention for cardiac hypokinesia is a radical type of treatment and is performed only in severe and life-threatening situations. In this case, the most effective way to eliminate painful symptoms and restore adequate trophism is a heart transplant.
Transplantation is usually recommended for diffuse myocardial damage or severe cardiac insufficiency associated with deep myocarditis. In the case of relatively mild cardiac hypokinesia, transplantation is considered inappropriate: drug therapy is sufficient.
Transplantation is prescribed:
- when cardiac output decreases to less than 20% of normal values;
- patients under 65 years of age;
- if conservative treatment is ineffective.
Surgery is not prescribed unless the true cause of hypokinesia is established.
In addition to transplantation, in some cases palliative surgical treatment may be used:
- Coronary artery bypass grafting is performed in cases of coronary circulation disorders and narrowing of the vascular lumen.
- Corrective surgery for aneurysm involves removing the damaged section of the vessel or strengthening it.
- Installation of a pacemaker – used in cases of severe heart rhythm disturbances.
Prevention
Prevention of cardiac hypokinesia is the prevention of other cardiac pathologies. In this case, the number one rule is to maintain a healthy lifestyle.
For people who care about their own health, the following useful tips can be given:
- Quitting smoking will help avoid coronary spasm and oxygen deficiency in the myocardium;
- Moderate physical activity will help strengthen the heart muscle, but the activity must be moderate;
- you need to visit your doctor regularly, including a cardiologist;
- it is necessary to treat any diseases in the body in a timely manner - in particular, infectious and hormonal pathologies;
- You need to avoid stress and conflicts, eat properly and nutritiously, and watch your weight.
Regularly - about once a year, it is advisable to have your blood tested for cholesterol. As a preventative measure against increasing this level, it is recommended to monitor your diet: do not eat too salty food, avoid eating large amounts of animal fat, do not abuse coffee, strong tea and alcoholic beverages.
 [ 36 ]
[ 36 ]
Forecast
The prognosis of cardiac hypokinesia depends on many factors: the degree of damage to muscle fibers, the presence of arrhythmia, the presence and stage of cardiac failure.
With timely medical intervention, as well as compliance with all necessary preventive and therapeutic measures, the painful process can be stopped and the development of serious complications can be prevented.
If a patient is diagnosed with a condition such as cardiac hypokinesia, he or she needs regular monitoring by a medical specialist, with a systematic examination of the entire cardiovascular system.
 [ 37 ]
[ 37 ]

