Medical expert of the article
New publications
HPV type 33: symptoms, treatment
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Today, in medicine, various diagnoses and incomprehensible abbreviations appear more and more often, which only frighten a simple, unenlightened person. A striking example is the diagnosis of "HPV type 33". What is this strange diagnosis? Let's look into all the details in more detail.
What is this?
Many people have to take laboratory tests. Having received the results, you can read such a frightening diagnosis in the blood test. The first thing that comes to mind is what is this? It turns out that in other words, this abbreviation can be called the human papilloma virus. The strain code is indicated next to it - 33. This is a virus that quite often persists in representatives of the Caucasian race.
Human papillomavirus (HPV) 33, a member of the alpha-9 group, accounts for approximately 5% of cervical cancer cases worldwide.[ 1 ],[ 2 ]
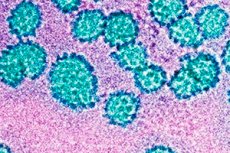
Structure HPV type 33
The structure of the virus is very specific. First of all, attention is drawn to the fact that the size of the virus can fluctuate within a fairly wide range - from 100 to 200 nm. The membrane is represented by two layers. The first layer is formed by lipids, the second is represented by a complex of glycoproteins. The components are connected to each other by non-covalent bonds.
High-risk HPV genotypes 33
The papilloma virus belongs to the Papillomaviridae family. This is a large group of viruses that cause tumors.
Twenty-eight HPV33 variants were identified, which formed five phylogenetic groups: previously identified lineages A1, A2, and B (sub) and new lineages A3 and C (sub).
HPV33 variants have been classified into two major lineages, A and B. Lineage A has been further divided into two sublineages, A1, which includes the prototype sequence [M12732.1 ( Cole and Streeck, 1986 ) [ 3 ], and A2. This classification is based on the determination that the complete genome sequence of a major variant lineage differs by approximately 1.0% from another variant lineage of the same HPV type, with differences of 0.5–0.9% defining sublineages (Chen et al., 2011 ). [ 4 ]
Sublineages A1 are distributed worldwide, although the relative frequency varies by region. Sublineages A2 were rarely detected in Africa and South America, while lineage B is specific to Africa. Sublineages C were found only in samples from Africa, and sublineages A3 were specific to Asia/Oceania, which is supported by two additional reports from China ( Wu et al., 2009 ) [ 5 ] and Japan [based on E6 only ( Xin et al., 2001 )]. [ 6 ] However, the observed rarity of lineages A3 and C must be taken into account when interpreting these results.
HPV DNA 33
The main component is the oncogene genes, which include protein components. They carry information that can trigger tumor growth. HPV 33 DNA is formed by two spirals. This enhances the properties of the virus. An important role is also given to regulatory cellular genes, which regulate the main cellular processes and transformation factors.
Life cycle HPV type 33
The life of a virus is cyclical and occurs in several stages.
At the first stage, the virus is absorbed into the host cell receptors. This process is possible due to the presence of glycoproteins in the membrane complex and the virions themselves.
The second stage is characterized by active penetration of the virus directly into the host's cellular structure. This triggers the main mechanisms of interaction of the virus with the cellular matrix. There are various mechanisms of interaction.
During the third stage, the virus moves around the cell, forming bubbles in which it is temporarily protected. The final point of virus transport is reaching the ribosomes and ER. Sometimes, viral particles and viruses themselves migrate to the nucleus.
The fourth stage can be described as the process of virion undressing. The essence of this process is deproteinization and release from the supercapsid and capsids.
At the fifth stage, the virion completely dissolves, and the process of synthesizing viruses begins, which subsequently destroy the cell and are released to the outside.
At the sixth stage, the virion is assembled and the nucleocapsid is formed. The process of self-assembly of viral particles is launched.
At the seventh stage, the viral particles leave the cell. Accordingly, the active stage of the infection begins, its progression.
Afterwards, the life cycle repeats itself, new cells become involved, and, accordingly, the disease develops and progresses.
Pathogenesis
HPV is transmitted primarily through skin-to-skin contact. Epidemiological studies clearly indicate that the risk of acquiring genital HPV infection and cervical cancer is related to sexual activity. HPV is very resistant to heat and drying, and asexual transmission can also occur, such as through prolonged contact with contaminated shared clothing [ 7 ]. A person is more at risk of acquiring HPV if he or she has had multiple sexual partners at any time or is the partner of someone who has had multiple sexual partners. Early sexual activity also puts a person at increased risk, as does a history of other sexually transmitted diseases, genital warts, abnormal Pap tests, or cervical or penile cancer in the person or a sexual partner. Using condoms may not adequately protect people from exposure to HPV because HPV can be transmitted through contact with infected labial, scrotal, or anal tissue that is not protected by a condom.
In addition to sexual activity, age is an important risk factor for HPV infection [ 8 ]. The highest metaplastic activity is observed during puberty and first pregnancy and decreases after menopause. HPV infection is most common in sexually active young women aged 18 to 30 years. The prevalence decreases sharply after age 30. However, cervical cancer is more common in women over 35 years of age, suggesting infection at a younger age and slow cancer development.
The primary immune response to HPV infection is cell-mediated; therefore, conditions that impair cell-mediated immunity, such as kidney transplantation or human viral diseases, increase the risk of HPV acquisition and progression.[ 9 ],[ 10 ]
Local immunosuppression caused by smoking and mutagenic activity of cigarette components has been demonstrated in cervical cells and may promote HPV persistence or malignant transformation similar to that observed in the lungs.[ 11 ],[ 12 ] Overall, knowing how HPV 33 is transmitted can help prevent infection.
Symptoms
There are several forms of the disease. The symptoms depend on this. In the sexual type of the disease, the mucous membranes of the genitals and the reproductive system are damaged. Pain, itching, burning, and irritation appear. Often, the symptoms resemble thrush: white discharge appears, sometimes cheesy. Warts, growths, and papillomas often appear directly on the mucous membrane of the vagina, cervical canal, and uterus.
In the cutaneous form, growths and papillomas may appear on the skin. They are mainly localized on the upper layer of the skin - the epidermis. They can be flat or elevated. It is also worth noting that warts can grow and multiply quite quickly. They can be either single or multiple. Often, warts are the only form of manifestation of this disease.
Sexually transmitted HPV infection results in one of three possible outcomes.
- The first is anogenital warts (condyloma acuminatum) on or around the genitals and anus in both men and women.
- The second outcome is latent or inactive infection, in which few people know they are infected because noticeable symptoms rarely occur and the infected area remains cytologically normal. HPV DNA is present in approximately 10% of women with cytologically normal cervical epithelium.
- The third outcome is active infection, which is associated with high-risk HPV types, in which the virus causes changes in infected cells that can lead to intraepithelial neoplasia of the penis, urethra, vagina, vulva, or cervix. High-risk HPV types include types associated with cervical cancer and types defined as intermediate risk, which are less commonly represented in cancers. These infections can lead to cervical cancer. Prospective studies have shown that 15 to 28% of women who were positive for HPV DNA developed SIL within 2 years, compared with only 1 to 3% of women who were negative for HPV DNA.
Papillomas
It looks like a wart, or a small lump that rises on a stalk. This structure is represented by connective tissue. It is covered with multilayered epithelium on top. It can rise quite strongly above the surface (on a stalk) on which it grows, and can also be flat and spread horizontally.
The growth rate is quite low, it is related to slow-growing tumors. The danger is caused by tumors located on internal organs: they can be damaged, cause bleeding. When localized in the lumen of internal organs (larynx, esophagus, intestines), they can grow and close the lumen. This causes the corresponding pathologies: suffocation, obstruction. Such tumors must be removed. The main method of treating papilloma is surgical, which consists of its excision.
HPV 33 in men
Quite often men are carriers of this virus, but the disease does not manifest itself in them. The virus can persist in the blood in an inactive form, or is simply suppressed by the immune system. But when in contact with a woman, she often becomes infected, since women have a much lower immunity, and it does not allow them to fully resist the infection.
The main manifestation is the formation of papillomas (multiple, single). For the purpose of treating HPV 33 in men, medications, herbal medicine, and homeopathic preparations are used.
HPV 33 in women
Women suffer from this virus more often. In this case, the genital form of the disease predominates. Most often, it manifests itself in the form of papillomas and condillomas located on the mucous membrane of the genitals. The danger is that there is a possibility of malignant degeneration of these neoplasms, their transformation into a malignant tumor. It is worth noting that often the only way to treat them is surgical excision. But after this, additional treatment is required, aimed at preventing relapse, preventing repeated neoplasms.
HPV 33 and moderate dysplasia
A distinctive feature is that they are potentially oncogenic, that is, they provoke the development of malignant neoplasms under certain conditions: reduced immunity, increased reactivity and sensitization, weakness, decreased endurance and resistance of the body, disruption of the biochemical cycle, normal structural and functional state of the body, as well as hormonal imbalance. Under such conditions, papillomas, fibromas, myomas, fibromyomas, fibrous growths develop. This is moderate dysplasia, which is directly related to HPV 33. This condition can be characterized as preceding cancer. There is always a potential risk of progression of these conditions and their transition to malignant tumors - sarcomas, cancers, leukemia.
HPV 33 and pregnancy
The appearance of HPV 33 during pregnancy is a bad sign, since this virus can lead to pregnancy pathologies. These can be spontaneous abortions, miscarriages, premature births, or stillbirths. Children often have developmental defects: physical deformities, various mental and functional deviations, as well as mental retardation (MR), mental retardation, speech defects, and emotional development.
But these are extreme cases that occur with a high concentration of viruses, a high viral load. Otherwise, with treatment and constant monitoring by a doctor, pregnancy can proceed normally. But there is always a risk of developing a genitourinary tract infection, bleeding, which is especially intensified during childbirth. There is an increased risk of infection of the child during childbirth.
Diagnostics
You will need an experienced virologist or immunologist. You can also contact an infectious disease specialist, laboratory doctor, biochemist, bacteriologist. If the clinic does not have such specialists, you need to contact the therapist assigned to the area, and he will refer you to the right specialist, or simply prescribe the necessary examinations. The main method of confirming the diagnosis is direct confirmation of the presence of the virus in the blood, which can only be achieved by taking the appropriate tests. Laboratory methods are used (these are the only effective and reliable research methods).
In most cases, the material of the study is blood. Virological and serological methods of research are prescribed, which allow to detect the virus itself in the blood, the products of its vital activity or DNA (its fragments). The laboratory uses various methods of analysis. But to detect the virus, it is worth using the PCR method, or DNA sequencing, with the help of which the viruses themselves are detected in the blood, and not antibodies as a reaction of the immune system to the introduction of the virus.
Type-specific PCR assays are based on sequence variations present in the E6 and E7 genes of HPV subtypes. Fourteen type-specific PCR assays for high-risk HPV types (HPV-16, -18, -31, -33, -35, -39, -45, -51, -52, -56, -58, -59, -66, and -68) target approximately 100 bp within the E7 ORF. [ 13 ]
The genome consists of over 100,000 nucleotides, 9 genes. On the inner surface there is a matrix framework. It is formed by proteins p17/18. The genome is formed by 3 structural genes and 6 regulatory ones. It is also worth noting that the virus is quite variable, especially when compared with other viruses. A number of researchers are still working on decoding the DNA of HPV type 33.
The ELISA (enzyme-linked immunosorbent assay) method is not informative, since it reacts to the amount of the antigen-antibody complex. Moreover, antibodies persist throughout life after a single illness. Therefore, it is impossible to draw a conclusion about the stage and degree of activity of the viral infection in the body.
A doctor's examination is also important. He will conduct a comprehensive examination and make a diagnosis. During a visual examination, the doctor will already be able to suspect the presence of HPV type 33, since it manifests itself with specific signs. But in order to finally confirm the disease, it is important not just to diagnose it, but to make a differential diagnosis. This means that the symptoms must be differentiated from other similar cases and similar manifestations.
Additional methods may include microscopic examination, scraping. Depending on the severity of the pathology, an immunogram, clinical and biochemical blood and urine tests, and dysbacteriosis tests may be required.
Microscopy will help to identify the virus itself or its waste products in a smear, examine the features and specific characteristics under a microscope. Based on these data, it is possible to determine the clear systematic position of the pathogen, down to the species and genus. The more accurately such identification is carried out, the more accurately and effectively it will be possible to select treatment. It is also important to obtain quantitative indicators, since the plan for further treatment and its effectiveness depend on the amount of virus in the blood (viral load).
The main method for detecting high-risk HPV remains the Pap smear (PAP). This test was named after pathologist George Papanicolaou, who introduced the test in 1949 before the cause of cervical cancer was known. Since its introduction, the Pap smear has helped reduce cervical cancer incidence and death rates by about half to two-thirds. [ 14 ] The Pap smear is a screening tool that looks for changes in the cells of the transformation zone of the cervix. Often, these changes are caused by HPV.
HPV Norm 33
From a medical and biological point of view, the norm is considered to be a complete absence of viruses in the blood. But this is an ideal case, which is extremely rare in the conditions of modern life. Therefore, there are certain conditional norms of HPV 33 in the body. But they differ greatly in different countries. There are only a few countries in which the absolute absence of the virus in the blood is considered the norm.
Treatment
Treatment consists mainly of surgical excision of neoplasms. Today, in addition to traditional surgery, there are a large number of methods for removing papillomas. Thus, the most effective methods are laser removal, cryotherapy, radio wave and radio frequency, electrocoagulation, thermal, electrothermal removal of papillomas. There is also removal of papillomas using chemicals.
Most HPV-induced changes in cervical cells are transient, and 90% regress spontaneously within 12–36 months as the immune system clears the virus.[ 15 ]
Traditionally, antiviral therapy has been used. For example, traditional drugs include inosiplex, interferon, amixin, cycloferone, podophyllin. Podophyllin, a cytotoxic agent that arrests mitosis in metaphase (also used to treat genital warts), in combination with vidarabine, a DNA polymerase inhibitor that suppresses HPV gene expression and cell growth in cervical cancer cell lines. [ 16 ]
IFN and intravaginal 5-fluorouracil have shown variable responses in clinical and in vitro studies. IFN-α is approved for the treatment of genital warts. The effects of IFN-α, IFN-β, and IFN-γ have been studied in several human carcinoma cell lines.[ 17 ]
It is important to conduct immunomodulatory therapy aimed at normalizing the state of immunity. Usually, immunostimulating therapy is required, which is based on increasing immunity. As a result, the immune system independently resists infection, its resistance and endurance increase, and the virus is suppressed.
Traditional treatment is used for prevention, postoperative recovery, or simply as an effective means of reducing the number of microflora and viral load. This can be drug therapy, various physiotherapeutic means, traditional medicine, homeopathy and phytotherapy. Preventive antiviral vaccinations are also carried out, which help prevent malignant degeneration of cells. When condillomas and papillomas are formed, their cauterization and burning are often used.
What to do if HPV 33 is detected?
First of all, you need to see a doctor who will select the appropriate treatment. The sooner the treatment is started, the more effective it will be. The doctor, based on the results of laboratory and instrumental studies, will tell you what to do. If HPV 33 is detected, drug or surgical treatment (excision of the papilloma) may be required. Antiviral, immunostimulating therapy is also used.
Is it possible to cure HPV 33?
This pathology responds well to treatment if the immune system is normal. So, if the immune system is low, various exacerbations, diseases, and relapses may be observed. The danger is that the virus is potentially oncogenic. If the immune system is normal, the virus can simply persist in the blood without causing an exacerbation of the infection.
Thus, answering the question: "Is it possible to cure HPV 33", it is impossible to give a clear answer. So, it is important to maintain immunity at normal level. Avoid overwork, stress. When conducting antiviral therapy, stimulating the immune system, vitamin therapy, it is possible to transfer the virus to an inactive state. Then it will persist in the blood without causing an acute disease. But it is almost impossible to completely eliminate the virus from the blood, a person remains a carrier of the virus and can infect others.
Prevention HPV type 33
Prevention is based on following hygiene rules, having an adequate sex life (having a regular partner, using protection when in contact with temporary partners, preventive treatment if a sexual partner has an infection. These are the main and basic preventive measures. It is also important to maintain a normal immune system - periodically consult an immunologist, get tested for viruses, latent infections, take courses of vitamins and, if necessary, immunostimulants.
It is important to eat right, include the necessary amount of vitamins and minerals in the diet, undergo regular preventive examinations, and, if necessary, undergo timely treatment. Maintaining a high level of immunity is especially important, since the development of the disease is possible only with reduced immunity and impaired microflora.
The main approaches to preventing HPV infection include both risk reduction and the development of HPV vaccines. The use of latex condoms and spermicides can reduce the risk of HPV infection. However, condoms are not completely reliable because HPV can be transmitted by contact with other parts of the body, such as the labia, scrotum, or anus, which are not protected by a condom.
A phase I, double-blind, randomized, placebo-controlled safety and immunogenicity study was conducted using a subunit vaccine consisting of a VLP generated from the entire L1 major capsid protein of HPV-16 strain 114K [ 18 ]. The vaccine was produced by inserting the L1 capsid gene into a baculovirus vector. The gene was then expressed in transfected Sf9 insect cells. An optimal dose of 50 μg of HPV-16 L1 VLP vaccine was administered by injection into the deltoid muscle at 0, 1, and 4 months. The vaccine generated high titers of type-specific neutralizing antibodies without adjuvant and was well tolerated.
As of 2017, Gardasil 9 ® is the only HPV vaccine available in the United States. Other HPV vaccines are available outside the United States. Gardasil 9 helps prevent infection with 4 types of HPV (16, 18, 6, and 11) and 5 other high-risk types: 31, 33, 45, 52, and 58. Together, these types cause about 90% of cervical cancers.
American Cancer Society Recommendations for Use of the HPV Vaccine.
- Routine HPV vaccination for girls and boys should begin at age 11–12. The vaccination series can begin as early as age 9.
- HPV vaccination is also recommended for women ages 13 to 26 and for men ages 13 to 21 who have not yet started the vaccine series or have started but not completed the series. Men ages 22 to 26 can also be vaccinated.
- HPV vaccination is also recommended at age 26 for men who have sex with men and for people with weakened immune systems (including people with HIV infection) if they have not been previously vaccinated.
- For people aged 22 to 26 years who have not yet started the vaccine or have started but not completed the series, it is important to know that vaccination at older ages is less effective in reducing the risk of cancer.
Forecast
In most cases, with proper and timely treatment, the prognosis will be favorable. HPV type 33 is quite easy to eliminate, the main thing is to maintain normal immunity, follow all the doctor's recommendations. If papillomas appear, their surgical removal (excision) may be required. This is a quick and painless procedure that practically does not require recovery. Antiviral treatment plays an important role. If left untreated, complications may arise. The most dangerous is the development of malignant neoplasms.

