Medical expert of the article
New publications
Examination of the lacrimal organs
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
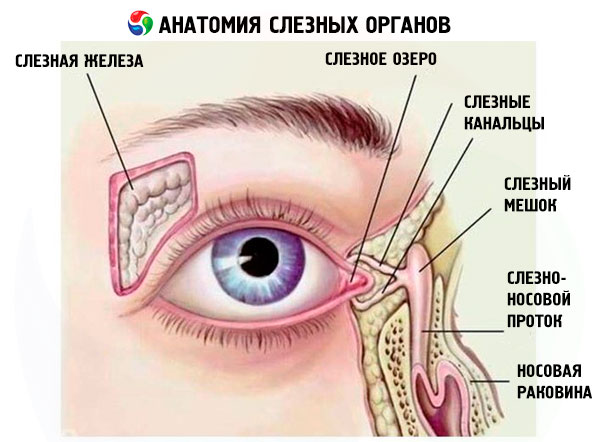
External examination of the lacrimal organs
- The marginal tear duct of both eyes is examined with a slit lamp before other lid manipulations or instillation of topical medications that may alter the clinical picture. Many patients with lacrimation do not have significant lacrimation, but on examination they have a high marginal tear duct on the affected side.
- The eyelids are examined for eversion of the punctum. Usually the inferior punctum faces the globe and is not visible without eversion of the lid margin. One of the most common causes of eversion of the eyelids and, consequently, the punctum is ectropion, which may be of involutional, paralytic, or cicatricial etiology. Such ectropion may also involve the lacrimal portion of the punctum. A rare cause of lacrimation is Centurion syndrome. In patients with this syndrome, lacrimation begins in childhood and is associated with eversion of the mid-eyelid with displacement of the punctum from the lacrimal lake due to a strongly protruding bridge of the nose. Sometimes, stagnation of tears may be caused by a large lacrimal caruncle displacing the inferior punctum outward from the globe or by obstruction of the inferior punctum by an excessive conjunctival fold (conjunctivochalasis).
- It is necessary to evaluate the dynamics of eyelid closure. Usually, when the edges of the eyelids are completely closed, the lacrimal points are connected. In patients with weakness of the lower eyelid, the upper eyelid may evert the lower one or cover the lacrimal point.
- The lacrimal punctum is best examined under a slit lamp. In addition to eversion, the lacrimal punctum may be inflamed, stenotic, or obstructed, sometimes by an eyelash. Canaliculitis is characterized by swelling of the lacrimal punctum and the release of pus when pressing on the canaliculi with a finger or glass rod. Pathology in children is represented by underdevelopment of the lacrimal punctum, an additional lacrimal punctum, or a congenital lacrimal fistula.
- The lacrimal sac is first palpated. When pressing on the lacrimal canaliculi, expression of mucous contents can be observed in patients with mucocele in the canalicular system, but in the presence of obstruction distal to the lower end of the lacrimal sac. In acute dacryocystitis, palpation is very painful, and strong pressure is best avoided. Sometimes, a compaction or tumor is detected during palpation of the lacrimal sac.
- The fluorescein retention (washout) test is performed by instilling 2% fluorescein into both conjunctival cavities. Usually, after 3 minutes, there is no fluorescein left or only a minimal amount remains. Its prolonged retention in the conjunctival cavity indicates insufficient tear drainage.
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ]
Probing and lavage
Performed only after the patency of the lacrimal point has been established. Under local anesthesia, a slightly curved, blunt lacrimal cannula on a syringe containing 2 ml of hypertonic solution is inserted into the lower lacrimal point and advanced along the canal. When attempting to enter the lacrimal sac, the middle wall of which is located opposite the bony lacrimal fossa, the cannula may rest against a hard or soft wall.
- Hard obstruction. If the cannula enters the lacrimal sac, it rests against its medial wall, through which the hard lacrimal bone can be felt. This excludes complete obstruction of the canalicular system. The doctor places a finger over the lacrimal fossa and injects the solution. If the solution enters the nose, the patient's lacrimal ducts are passable. If the nasolacrimal duct is obstructed, the solution does not enter the nose, which means either stenosis of the lacrimal ducts or a disorder of the lacrimal pump mechanism. In this situation, the lacrimal sac increases in size during irrigation and fluid is backflowed through the superior lacrimal punctum. The regurgitated material can be clear, mucous, mucopurulent, or purulent, depending on the contents of the lacrimal sac.
- Soft obstruction. If the cannula rests against the proximal junction of the common canaliculi and the lacrimal sac, i.e. the lateral wall of the sac, without reaching it, a soft resistance is felt, since the cannula rests against the soft tissues of the common canaliculi and the lateral wall of the sac. During irrigation, the sac does not increase in size. In case of lower canaliculi obstruction, reflux of the solution will pass through the lower lacrimal punctum. Reflux through the upper lacrimal punctum indicates patency of both the upper and lower canaliculi in case of common canaliculi obstruction.
Jones test
It is performed in patients with suspected partial drainage obstruction. They have more pronounced lacrimation, but the lacrimal system may be well-patented. The staining test is of no value in complete obstruction.
The canalicular test (first test) differentiates partial obstruction of the lacrimal passages from primary hypersecretion of tears. First, 2% fluorescein is instilled into the conjunctival cavity. After about 5 minutes, a cotton swab soaked in local anesthetic is inserted into the inferior nasal passage at the outlet of the nasolacrimal canal. The result is interpreted as follows.
- positive: a cotton swab removed from the nose and stained with fluorescein indicates patency of the lacrimal ducts. Lacrimation is due to primary hypersecretion, so no further investigation is necessary;
- negative: the cotton swab is not stained, therefore there is partial obstruction (location unknown) or the lacrimal pump is not working. In this situation, the test is repeated immediately.
In 22% of healthy people, the first Jones test is negative.
The nasal test (second test) identifies the probable area of partial obstruction based on the influx of fluorescein removed in the first test. Instillation of local anesthetic washes away any residual fluorescein. Saline is then injected into the lacrimal drainage system with a cotton swab at the inferior nasal passage.
- positive: fluorescein-stained saline enters the nose, indicating that fluorescein has penetrated the lacrimal sac. Thus, the functional competence of the upper lacrimal ducts is confirmed, partial obstruction of the nasolacrimal ducts is excluded;
- negative: unstained saline flows into the nose, indicating that fluorescein has not entered the lacrimal sac. This indicates partial obstruction of the superior lacrimal duct (punctum, canaliculus, or common canaliculus) or a disorder of the tear suction mechanism.

