Medical expert of the article
New publications
Uterine endometrial cancer: signs, ultrasound diagnosis, prognosis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Epidemiology
According to statistics, approximately 4.5% of patients with bloody discharge in the postmenopausal period are diagnosed with uterine cancer.
Over the past decade, economically developed regions have demonstrated a marked increase in the incidence of endometrial cancer: this pathology accounts for 13% of all oncological processes in women and is found mainly in patients aged 55 to 60 years.
According to world statistics, endometrial cancer is the most common female oncology, ranking sixth among all malignant processes (only breast cancer, cervical cancer, colorectal cancer, as well as lung and stomach cancer are more common).
Over the past ten years, mortality rates in patients with endometrial cancer have decreased relatively, but at present this pathology continues to occupy 8th place in terms of mortality rate.
Causes endometrial cancer
Endometrial cancer is a neoplasm that is related to a woman's hormonal background and is sensitive to an imbalance of steroid hormones. Proliferation processes are triggered by regulatory disorders within the hypothalamus-pituitary system: hyperplasia begins in the endometrial layer, which is an ideal basis for the formation of malignant changes.
The reasons for such phenomena may be:
- human immunodeficiency virus;
- decompensated conditions (hypertension, diabetes);
- papilloma virus;
- long-term or chaotic treatment with hormonal drugs;
- sexually transmitted infections;
- early sexual activity, early abortions (frequent abortions);
- lack of order in sexual life;
- absence of pregnancies throughout the entire reproductive period;
- frequent irregularities in the menstrual cycle, late onset of menopause.
The main factors that influence the level of estrogen in the blood (one of the causes of endometrial cancer) are considered to be:
- early menarche, late menopause;
- absence of pregnancies throughout the entire reproductive period of a woman's life;
- Incorrectly selected means for hormone replacement therapy, chaotic hormonal treatment.
One of the obvious causes of endometrial cancer, according to experts, is various damaging effects on the mucous tissues of the uterus. Such damage may include scars, adhesions, erosions, birth injuries, polypous and condylomatous neoplasms, leukoplakia, chronic inflammation (for example, endometritis, endocervicitis).
Obesity often leads to the evolution of endometrial cancer. Thus, women whose weight exceeds the norm by 20 kg are three times more likely to encounter the disease, in contrast to patients with normal weight. If the excess weight is more than 25 kg, then the risk of developing cancer increases nine times. The essence of this trend is that fat cells produce estrogens, which can make up from 15 to 50% of the total amount of estrogens in the body.
 [ 8 ]
[ 8 ]
Risk factors
What can be a risk factor for developing cancer in the uterus?
- Early or late menopause.
- Obesity.
- Long-term use of hormonal drugs (for example, due to inability to conceive, or for the treatment of other female diseases).
- Unfavorable heredity (someone in the family suffered from malignant diseases of the reproductive organs).
- Early onset of sexual activity, promiscuous sexual relations.
- Frequent sexually transmitted infections, chronic inflammatory diseases of the reproductive organs.
- Immune system failures.
- Alcohol abuse, smoking, and other types of addictions that provoke intoxication of the body.
Endometrial cancer in the elderly
Cancer processes in elderly people have their own characteristics. For example, they are more likely to have advanced malignant forms, the most aggressive morphological types of pathology. In addition, there are violations in the implementation of prescribed treatment - due to the reduced functional reserve of patients.
Most elderly women already have numerous diseases, including chronic ones, which often require constant medication. Not in all cases can such therapeutic schemes be combined without harming the patient's health. Therefore, clinical protocols in old age are rarely carried out, given the risks of complications.
The approach to treating endometrial cancer in people over 70 years of age should be very gentle: from this age, the risk of death increases threefold, and by 75 years - almost fivefold. At the same time, the indicators of overall and relapse-free survival are significantly reduced. In addition, older patients are much more likely to have contraindications to surgical intervention. Therefore, treatment is often aimed only at alleviating the condition and prolonging the life of a sick person.
Pathogenesis
Endometrial cancer belongs to the category of hormone-dependent tumor processes: this has been confirmed by a number of scientific experiments and clinical projects, during which it was possible to prove that such a disease often develops against the background of other disorders of the endocrine system and metabolism.
Among women diagnosed with uterine cancer, there is a fairly large percentage of those who have never had a child or are even virgins. They often have fibroids and feminizing tumor processes in the ovaries.
Endometrial cancer is predominantly located at the bottom, sometimes in the isthmus area. The tumor can grow outward, inward, or simultaneously in both directions (mixed type). Spread most often occurs through the lymphatic system, less often through the bloodstream or by implantation. The implantation route is tumor growth involving the parietal and visceral peritoneum: the appendages are affected, metastases spread to the greater omentum (mainly with low differentiation of the neoplasm).
There are several basic stages in the pathogenetic development of endometrial cancer:
- Stage I of functional disorders (absence of ovulation, increased estrogen levels).
- Stage II of the formation of morphological disorders (glandular cystic hyperplasia, polyposis).
- Stage III of the formation of precancerous morphological disorders (atypical hyperplasia and dysplasia of the epithelium in the third stage).
- Stage IV – formation of onconeoplasia (preinvasive cancerous tumor → minimal invasion into muscle tissue → obvious form of endometrial cancer).
- Is endometrial hyperplasia cancer?
Endometrial hyperplasia is a dangerous disease in which the mucous tissue grows in the uterine cavity. But despite the danger, hyperplasia is not cancer yet, although it is a favorable process for the development of oncology. Timely removal of the area with pathological mucous tissue allows you to stop the development of the disease and thereby prevent the development of a malignant process.
- Is atypical endometrial hyperplasia cancer?
Atypical, or atypical hyperplasia is the most insidious type of this pathology. It is this type that most often develops into a malignant tumor. However, this disease also has a favorable prognosis if timely and competent treatment is prescribed.
- Does endometrial hyperplasia progress to cancer?
Indeed, endometrial hyperplasia has a tendency to malignancy, that is, to cancerous degeneration. This is especially true for the atypical type of the disease (this type becomes malignant most often, so radical methods are often used to treat it, such as hysterectomy). In other cases, combination therapy is mainly prescribed, which involves both surgery and hormonal treatment.
- Is adenomatous endometrial hyperplasia cancer?
Adenomatous hyperplasia, also called complex hyperplasia, is characterized by the formation of atypical structural units inside the endometrial layer of the uterus. This pathology affects approximately three patients out of a hundred – that is, the disease is quite common. However, it does not belong to cancer processes: endometrial cancer can be a complication of the lack of treatment or improper treatment of this disease.
Pathogenetic variants of endometrial cancer
For medical professionals, two pathogenetic variants of endometrial cancer have been identified.
The first variant is the most common: the pathology develops in relatively young patients as a result of prolonged elevated levels of estrogens in the body and signs of hyperplasia. With this type of disease, patients often have excess weight, metabolic disorders, hypertension, and sometimes hormone-secreting neoplasms in the ovaries, glandular cystic hyperplasia of the endometrium or GCOS. Such tumors are often highly differentiated and have a relatively favorable prognosis.
The second option is low-differentiated neoplasms with a less favorable prognosis. Such pathology develops in older patients: there is no hyperestrogenism, there is atrophy of the endometrial layer.
Approximately 80% of patients diagnosed with endometrial cancer have adenocarcinoma. Approximately 5% have a tumor associated with hereditary pathologies, such as non-polyposis colorectal cancer.
 [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ]
[ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ]
Symptoms endometrial cancer
The early stage of endometrial cancer is asymptomatic. The first signs may appear in the form of bloody discharge from the vagina, watery leucorrhoea and pain in the abdominal area. The main symptom that is recorded most often is uterine bleeding: this symptom is atypical, since it can be observed in most gynecological disorders (for example, in adenomyosis, uterine fibroids).
In patients of reproductive age, endometrial cancer is most often detected against the background of long-term observation and treatment for dysfunction of the hypothalamic-pituitary system. This is a fairly common diagnostic error in endometrial cancer: doctors often make mistakes when examining young women, since oncology is suspected mainly in older patients.
The basic symptoms for which women seek medical help are:
- non-cyclic uterine bleeding;
- difficulties in conceiving;
- impaired ovarian function.
However, bleeding is a typical symptom only in the postmenopausal period. At a younger age, this symptom may only appear when a woman is diagnosed with combined endometrial and cervical cancer – that is, at a later stage of the disease.
Discharges in the form of massive serous secretion in the absence of signs of inflammation of the genitals in endometrial cancer are typical for elderly patients. Such discharges are almost always abundant, serous-watery (the so-called leukorrhea).
Pain of varying degrees is the latest sign of endometrial cancer. The pain is felt mainly in the lower abdomen or in the lumbosacral region, and is continuous or occurs as short-term contractions. Unfortunately, the overwhelming majority of patients come for medical help late, when all the symptoms of the spread of the pathological focus are already present.
Many specialists associate endometrial cancer and metabolic syndrome: patients experience high blood pressure, obesity, insulin resistance, and myocardial hypoxia. It is worth noting that this syndrome can be both a factor and a consequence of endometrial cancer. Signs of such a disorder include fatigue, apathy, irritability, and mood swings when hungry. The symptoms are not typical and require additional diagnostics.
 [ 23 ]
[ 23 ]
Stages
There are two classification options for endometrial cancer stages. One of the options was presented by the FIGO MA of Obstetricians and Gynecologists. The second option defines endometrial cancer by tnm, assessing both the size of the formation and the probability of lymphatic system involvement or distant metastasis.
According to the first version of the classification, medicine distinguishes the following stages of the disease:
- Early endometrial cancer is the so-called "zero" stage, at which the pathology is just beginning to develop without spreading. This is the most favorable stage, with complete cure rates in the range of 97-100%.
- Stage 1 is divided into several substages:
- Stage 1a is the stage of germination of the process into the tissue, without going beyond the endometrial layer;
- Stage 1B is a similar stage in which the tumor grows into the muscle layer;
- Stage 1c – tumor growth approaches the outer layer of the organ.
- Stage 2 is accompanied by the spread of pathology to the tissues of the cervix:
- Stage 2a – cancerous changes affect the cervical glands;
- Stage 2b – stromal structures are affected.
- Stage 3 corresponds to the emergence of the malignant process beyond the uterine organ, without spreading beyond the pelvic area:
- Stage 3a – appendages are affected;
- Stage 3b – the vagina is affected;
- Stage 3c – nearby lymph nodes are affected.
- Stage 4 corresponds to further spread of the tumor with metastasis:
- Stage 4a – accompanied by damage to the urinary tract and/or rectum;
- Stage 4B – accompanied by the spread of distant metastases.
Staging tnm involves taking into account three parameters: t (size of the tumor), n (lymph node involvement) and m (presence of metastases).
The parameters are decoded as follows:
- t is – precancerous pathology;
- t1a – the neoplasm is localized within the organ and has dimensions of up to 80 mm;
- t1b – the neoplasm is localized within the organ, but its dimensions exceed 80 mm;
- t2 – the pathology has spread to the cervix;
- t3 – the tumor has spread beyond the uterus, but has not left the pelvic area;
- t4 – the tumor has grown into the rectum and/or bladder tissue, or has left the pelvic area;
- n0 – lymph nodes are not involved in the process;
- n1 – lymph nodes are involved in the process;
- m0 – no distant metastases;
- m1 – there is a suspicion of distant metastases.
Forms
According to the generally accepted classification, the following histological forms of endometrial cancer are distinguished:
- Endometrial glandular cancer (adenocarcinoma) originates from endometrial glandular cells. This is a hormone-dependent process, since the condition of the glandular tissues of the endometrium undergoes cyclic changes under the influence of sex hormones - steroids. In turn, adenocarcinoma is divided into highly differentiated, moderately differentiated and poorly differentiated tumors.
- Hyperplastic endometrial cancer is a cancerous process caused by hyperplastic changes in the endometrial layer. Hyperplasia is considered the most likely basis for the development of malignant tumors.
- Mucinous endometrial carcinoma: This type includes neoplasms that show signs of mucinous differentiation, but do not have the specific characteristics of adenocarcinoma. The tumor is represented by cellular structures consisting of intracytoplasmic mucin. This type occurs in 1-9% of all glandular forms of uterine cancer.
- Serous endometrial cancer belongs to a large group of epithelial tumors. The process develops from modified or transformed epithelial tissues. The disease is dangerous, as it has a particularly hidden aggressive course and is discovered by chance.
Here is what German oncologists say about serous endometrial cancer of the uterus: “The latest studies have shown that women who carry the BRCA1 genetic mutation have a higher probability of developing serous aggressive cancer: they are recommended to have their uterus and appendages removed as soon as possible after the mutation is detected.” It was found that in four out of five cases, serous cancer developed in patients with the BRCA1 genetic mutation.
- Squamous cell endometrial cancer is a neoplasia formed from squamous epithelial structures that have become atypical. Most often, such cancer is caused by the human papillomavirus, but can also be provoked by the herpes simplex virus, cytomegalovirus, etc.
- Undifferentiated endometrial cancer is a type of tumor whose nature can only be assumed, mainly due to the underdevelopment of the cells and the lack of signs of belonging to any type of tissue. Such cells are simply called "cancer cells." Undifferentiated cancer is one of the most malignant neoplasms and has the worst prognosis.
Complications and consequences
Endometrial cancer is a complex and dangerous disease in itself, but it can also cause a host of additional complications and problems. The tumor can compress other tissues and organs, difficulties with urination may arise, hydronephrosis and purulent infection of the urinary tract may develop.
Bleeding from the genital tract occurs no less frequently, which, if a doctor is not consulted in a timely manner, can lead to death.
In advanced pathology, fistulas can form - peculiar pathological openings in the walls of the intestine, bladder, vagina. Such a complication also often becomes the cause of the patient's death.
Relapse is considered theoretically possible, so the patient is monitored for a long time after the initial treatment. The following conditions require urgent medical intervention:
- bleeding (uterine or rectal);
- sudden appearance of swelling of the lower extremities, ascites;
- the appearance of abdominal pain;
- the appearance of shortness of breath, spontaneous cough;
- loss of appetite, sudden weight loss.
Metastases, routes of metastasis
The main route of metastasis spread is lymphogenous, through the lymphatic system. Metastasis is mainly determined in the para-aortic and iliac lymph nodes.
Metastases are a kind of "pieces" of tumor that have a similar structure and properties. Why do they appear and separate from the main tumor site?
As the neoplasm - endometrial cancer - rapidly grows and develops, it gradually loses the ability to "nourish" all of its elements. As a result, some structural parts separate and are carried by lymph or blood to different parts of the body, where they take root and begin to exist independently, as a separate tumor (now a daughter tumor).
Most often, metastases “settle” in nearby lymph nodes, but they can spread further - to the lungs, liver, bones, etc. If single “siftings” can still be tracked and destroyed, then multiple metastases are almost impossible to detect: in this case, it is necessary to resort to maintenance treatment with chemotherapy drugs in order to prolong the patient's life.
Diagnostics endometrial cancer
The diagnosis of endometrial cancer is established after receiving the results of a study conducted by a gynecologist, followed by a consultation with an oncology specialist. Sometimes a so-called "second opinion" may be important - this is obtaining a consultation from an outside specialist (for example, a parallel visit to another clinic with subsequent comparison of the results). This is done in order to exclude possible errors in diagnosis, because cancer is a fairly serious and complex disease.
The doctor may initiate the following laboratory tests:
- general blood and urine tests;
- blood biochemistry;
- coagulogram;
- blood test for tumor markers – specific protein substances, the content of which increases if there is a tumor process in the body.
- Genetic analysis for endometrial cancer (or rather, if the disease is suspected) is carried out:
- patients with HPV;
- patients with an adverse heredity, whose relatives suffered from endometrial cancer;
- patients taking hormonal drugs.
A study of mutations in several gene groups is conducted, which allows determining the individual degree of risk of endometrial cancer. In turn, this will help the doctor navigate in determining further tactics of treatment and preventive measures.
Instrumental diagnostics primarily includes a smear for oncological cytology. This type of examination allows you to determine early precancerous signs of the disease: this method is available and can be used several times throughout the diagnostic course.
The standard instrumental approach involves performing a bimanual vaginal examination using speculums, as well as a similar rectal examination.
If necessary, an aspiration endometrial biopsy is prescribed. Endometrial tissue is aspirated using a Braun syringe. This method is effective in 90% of cases.
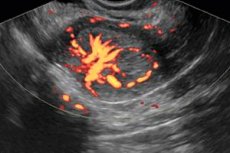
An ultrasound examination of the pelvis helps to examine changes that have occurred in nearby tissues and organs.
Important ultrasound signs are revealed when measuring the MEHO (median echo of the uterus):
- in patients of reproductive age, the Meho value is no more than 12 mm;
- in postmenopausal patients this value should not be more than 4 mm;
- an increase in the anteroposterior size exceeding standard values can be regarded as a probable sign of the development of a malignant process.
- The thickness of the endometrium in endometrial cancer is assessed as follows:
- if the median echo value is more than 12 mm, then an endometrial aspiration biopsy is performed;
- if the Meho value is less than 12 mm, then hysteroscopy with targeted endometrial biopsy is performed;
- If the value is less than 4 mm, then monitoring of the process dynamics is established.
As a rule, histology plays a decisive role in diagnosing endometrial cancer, making it possible to determine the type of morphological abnormalities. Young patients belonging to any of the risk groups are recommended to undergo cervicohysteroscopy. This diagnostic method allows assessing the spread and depth of the neoplastic reaction, as well as performing a targeted biopsy of the altered tissues.
To determine the degree of damage to the lymph nodes and adjacent tissues, X-ray diagnostics are prescribed: ileocavagraphy, irrigography, rectoscopy, pyelography, lymphography, cystoscopy.
In addition, magnetic resonance imaging of the chest and abdominal organs, as well as computed skeletal tomography, are recommended. Endometrial cancer is determined by the presence of lymph node lesions on MRI.
Differential diagnosis
Differential diagnostics is quite complex and is usually carried out taking into account all diseases of the genital area that are accompanied by similar symptoms. We are talking about cervical cancer, dysfunctional conditions, fibroids, chorionepithelioma, ovarian cancer, etc. Many of the pathologies listed can occur independently or in combination with endometrial cancer.
Endometrial hyperplasia, like endometrial cancer, have one common symptom - bloody discharge in postmenopause. Therefore, it is very important to identify these pathologies in a timely manner: first of all, the help of an ultrasound examination method is necessary.
Endometriosis is usually diagnosed laparoscopically: symptoms are often mild, but differentiation cannot be made based on the clinical picture alone.
Uterine myoma is often combined with endometrial cancer, so it is practically important to separate and identify these pathologies. A patient diagnosed with myoma undergoes both probing and a complete cytological examination (or fractional curettage) with subsequent histological assessment of the scraping. If accelerated growth of individual areas of the neoplasm is noted, and the patient's condition rapidly deteriorates, then uterine sarcoma can be suspected.
When differentiating between cervical and endometrial cancer, the patient's age criteria, as well as functional and somatic characteristics (excess weight, concomitant diseases), information obtained during an external examination (absence of atrophic changes in the genitals) and a bimanual examination are necessarily taken into account. To clarify or refute the suspected diagnosis, a complete cytological examination with an analysis of endometrial scraping is performed.
Hormone-producing ovarian cancer may occur simultaneously with carcinoma, or represent a separate pathology with signs typical of endometrial cancer. In advanced stages of ovarian cancer, when the malignant lesion spreads to the endometrium, characteristic acyclic bleeding may be observed. In this situation, bimanual examination and cytomorphological information are necessary.
Polycystic ovary syndrome (PCOS) is rarely suspected simultaneously with endometrial cancer: the disease is differentiated, first of all, from thyroid diseases, hyperprolactinemia, congenital dysfunction of the adrenal cortex. However, in some cases, combined development of pathology is possible. Laboratory studies of hormonal levels are carried out, which allows one to verify the origin of the problem.
An endometrial polyp, unlike a cancerous tumor, is easily diagnosed: it is detected during an ultrasound (with a repeat examination after menstruation). If especially necessary, an aspiration biopsy is prescribed.
Who to contact?
Prevention
Unfortunately, there are no preventive measures that would give a 100% guarantee that endometrial cancer will never appear. However, we should not forget about a number of factors that can become triggers in the development of oncology. Thus, you should monitor your weight, not take hormonal drugs without control, and systematically - at least once a year - visit a gynecologist.
If there are any problems in the form of diseases of the genital area, then they must be treated in a timely manner.
If you have any suspicious signs related to the reproductive system, you should see a doctor: even minor bleeding from the genital tract can be a harbinger of a tumor process. And you can’t forget about this.
In addition, it is important to eat right, include fiber and healthy foods in your diet, and eliminate bad habits.
And another important point is hygiene of sexual life. Prevention of sexually transmitted diseases, presence of a stable healthy partner is the key to the health of a woman's reproductive organs.
Forecast
The basic factor that determines the quality of the prognosis for endometrial cancer is the stage at which the pathology is detected. Aggravation of the malignant process is observed in approximately every fourth patient diagnosed with an early stage of the disease. A number of unfavorable factors can be identified that worsen the prognosis for a cancerous tumor:
- the patient is over sixty years old;
- unfavorable histological variation with a low degree of differentiation of the tumor process;
- deep malignant lesion of the muscular layer of the uterus (more than 50% of the myometrium);
- transition of the malignant process to the cervix;
- cancer embolism of the vascular lumens of the blood or lymphatic circulation system;
- spread to the peritoneum;
- a malignant lesion of significant size;
- low levels of progesterone and estrogen receptors in the tumor site;
- the presence of cancerous structures in the abdominal cavity swab material;
- change in the karyotype of the neoplasm;
- oncogenic expression.
Patients with endometrial cancer how long do they live? Survival, chances of life with endometrial cancer depend on the degree of prevalence and differentiation of the cancer process.
After surgery, the 5-year survival rate can range from 5 to 85%, depending on the stage of the pathology. The best prognosis is for patients with stages I and II cancer. Thus, the survival rate over a five-year period for patients with stage I is within 85-90%, and for patients with stage II - within 70-75%. Patients diagnosed with stage III endometrial cancer survive in approximately 30% of cases, and with stage IV, the five-year survival rate is only 5%.
If the disease recurs, it most often occurs within the first three years after the end of therapy. Relapse of the problem can be detected (by detection frequency):
- in the vaginal tissues;
- in the pelvic lymphatic system;
- on the periphery (at a distance from the main focus).
The 10-year survival rate for endometrial cancer ranges from 3.2 to 71.5%, with the best rates observed in patients with tumors that have progesterone receptors.
Endometrial Cancer Patient Forums
Endometrial cancer is a complex and serious disease, and sometimes it is difficult for a woman to cope with her own thoughts and fears on her own. Therefore, forums often come to the rescue, where it is possible to communicate with people who have encountered a similar problem. Each patient can share their story, give new information, or clarify for themselves some aspects related to the disease. Not only patients, but also doctors share their comments here: all this results in great support for the patient, and even in stimulation of healing. Among patients diagnosed with endometrial cancer, the most popular forums are the following:
- www.rakpobedim.ru
- www.oncoforum.ru
- oncomir.listbb.ru
- forum.sakh.com

