Medical expert of the article
New publications
Double uterus
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
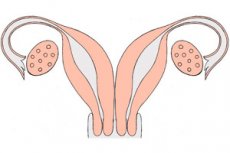
A double uterus is a very rare congenital disorder. It is a developmental defect of the reproductive organ, which during its development becomes paired, as a result of embryogenetic non-fusion of the Müllerian ducts. A double uterus has two separate cervixes and sometimes even a double vagina: each of the uteri is equipped with one horn connected to the fallopian tube, "looking" at the corresponding ovary.
Women with a double uterus do not always realize their "peculiarity", since the anomaly may not manifest itself clinically, and pregnancy is quite likely. If the disorder creates any problems with reproductive health, then they resort to surgery - the only way to correct the pathology.
Epidemiology
Double uterus is a congenital defect of the reproductive mechanism. This disorder occurs as a result of a complete failure to connect the Mullerian ducts along the midline, which leads to the formation of two separate uterine organs with a vaginal septum. This anomaly is considered rare: the incidence rate ranges from 1:1000 to 1:30000 (according to statistical information collected in the United States of America, the incidence is 1 case per 3 thousand women).
Each of the formed uteruses is connected to one fallopian tube and a corresponding ovary.
The occurrence of twin pregnancy, in which the fetus develops in a separate uterus, in patients diagnosed with a double uterus is a particularly rare case, occurring at a frequency of 1:1 million.
The occurrence of pregnancy with a double uterus is considered quite probable, provided there are no other reproductive disorders. According to statistics, infertility is observed in 12-30% of patients, and the frequency of miscarriage varies within 30-80%, with the frequency of premature births being about 28 percent. It has not yet been clarified whether such indicators are only a consequence of an organ anomaly, or whether a double uterus is combined with morphofunctional insufficiency and a failure of the hypothalamic-pituitary-ovarian hormonal mechanism, as well as a disorder in the formation of the fetoplacental system.
Gestosis during pregnancy is detected in approximately 10% of women with a double uterus, abnormal fetal position was determined in 15-20% of cases. A high frequency of surgical delivery (caesarean section) is also noted - in 45% of cases. Fetal hypotrophy was detected in 27%, low birth weight - in 15% of cases.
According to experts, women with an anomaly often experience high blood pressure during pregnancy, and preeclampsia occurs twice as often as in other pregnant women with a normal uterus.
Causes twin uterus
The urogenital system as a whole is formed during the intrauterine period from a single embryonic link, so any disruption in it can become the root cause of the formation of several defects at once. For example, a double uterus is often found in combination with other congenital diseases of the genitourinary system. Such a problem can appear in the following cases:
- in genetic disorders;
- in severe pregnancy (prolonged threatened miscarriage, gestosis, lack of nutrients, intrauterine infection of the fetus);
- prolonged intoxication during pregnancy (for example, drug-induced, professional, etc.);
- complex systemic diseases in the expectant mother.
In many cases, the true cause of the violation cannot be determined.
Hazel Johnson and the Double Uterus
Such an anomaly as a double uterus has always existed. However, close attention to the problem appeared after the story of Hazel Johnson, a woman from High Wycombe (UK), who was found to have a complete doubling, was made public. Hazel took part in a popular program on the ITV channel, where she told the whole country about her peculiarity. She pointed out, among other things, that she feels quite comfortable and practically does not suffer from the anomaly. The only problem is the beginning of the monthly cycle, which is more difficult than it should be normally.
Doctors examined the patient and concluded that there was no need for surgical correction of the defect in Hazel. However, if the woman wants to get pregnant, she will need to be constantly under the supervision of specialists - in particular, due to the small size of the double internal genitalia. Caesarean section is recommended.
Risk factors
Particularly common risk factors include:
- exposure to occupational hazards during a woman's pregnancy;
- bad habits (alcohol consumption, smoking, drug addiction);
- viral infections during pregnancy (flu, toxoplasmosis, rubella);
- intoxicating effects of medications.
There is evidence of a possible genetic predisposition to the development of reproductive organ anomalies. Thus, it was found that the risk of developing a double uterus increased in families in which cases of other developmental defects had previously been recorded - for example, doubling of the kidneys, hypoplasia, etc.
Risk factors during pregnancy include:
- acute respiratory viral infections in the first trimester of pregnancy;
- taking hormonal drugs or non-steroidal anti-inflammatory drugs, salicylates;
- gestosis.
Women at risk require thorough prenatal diagnostics, the introduction of rational pregnancy management tactics, and timely detection of disorders.
Pathogenesis
In the pathogenetic aspect, several types of development of a double uterus are distinguished:
- Complete duplication, in which there are both two uterine organs and two vaginas that are not connected to each other.
- Incomplete duplication, when there are two uterine organs and two vaginas, separated at a certain place by a muscular-fibrous membrane.
- A complete duplication with one vagina, in which there are two uterine organs and two cervixes, but one vagina.
- Uterine duplication with one cervix and vagina.
- Uterine doubling, in which there is one full-fledged organ and one rudimentary (underdeveloped) one.
- Bicornuate uterus, partially divided into two zones.
- Saddle-shaped uterus with a deformed fundus without division of the organ.
- One uterus, divided by a septum (partially or completely).
The bicornuate reproductive organ with a partially overlapping internal membrane (the so-called uterus subseptis) is divided into two halves that communicate in the cervical region. The membrane may vary in size. This defect is associated with insufficient reabsorption of the junction of the Müllerian ducts.
In the presence of a complete septal membrane (uterus septis), the entire internal uterine cavity is fenced off, forming two parts isolated from each other - from the fundus to the internal os.
The double (divided) body and common cervix (uterus bicollis unicollis) are a pair of separated uterine cavities that share a common cervical canal.
A double body with an atrophic or atretic change in one horn must be distinguished from a congenital anomaly in the development of the uterine part and post-traumatic fusion of its cavity.
The formation of a bicornuate uterus with an atretic internal cavity is due to the non-fusion of the Müllerian ducts and the fusion of their lumen. The reproductive organ itself has a powerful structure, or has a separate small cavity in the area of one horn. [ 1 ]
Symptoms twin uterus
Most patients with a double uterus do not show any pathological signs: they have a normal and regular monthly cycle, although sometimes menstrual bleeding is heavier. With complete doubling of the organ and a double vagina, problems in the intimate sphere appear. [ 2 ]
In some women, symptoms are detected somewhat later – in particular, problems associated with conception and bearing a child may arise:
- threatened miscarriage throughout the entire period of gestation;
- spontaneous termination of pregnancy at an early stage;
- late miscarriages;
- formation of habitual miscarriage;
- premature birth;
- infertility.
With a rudimentary second uterine organ, problems associated with the deterioration of the outflow of menstrual blood may arise:
- pain in the lower abdomen, which intensifies during menstruation;
- abdominal enlargement, feeling of pressure and distension.
If the rudimentary part is connected to the cervix, then the following symptoms may appear:
- spotting a few days before menstruation and for a few days after menstruation;
- heavy menstrual bleeding.
In such a situation, the risk of developing an ectopic pregnancy increases. In addition, the formation of genital endometriosis is possible, which is accompanied by the following symptoms:
- bloody discharge in the middle of the monthly cycle;
- increasing weakness, fatigue;
- algomenorrhea;
- pelvic pain;
- problems with getting pregnant;
- hypermenorrhea;
- irregularity of the monthly cycle;
- pain and discomfort during and after sexual intercourse.
Often, the patient does not even suspect that she has such a feature - a double uterus. The woman lives a normal life, gets married, gets pregnant, gives birth to a child. In most cases, everything proceeds without any specific symptoms. Difficulties may arise if we are talking not only about a double uterus, but also about a double vagina.
Some patients experience excessively heavy and particularly uncomfortable periods: such a disorder may serve as a reason to consult a doctor, where a developmental anomaly is discovered.
The altered configuration of the organ in a double uterus can negatively affect the functionality of other nearby organs: the woman feels that something is wrong with her. The discomfort can be both physical (abdominal pain, a feeling of distension and pressure) and psychological (if the patient knows about her peculiarity). Many people mistakenly associate a double uterus with female inferiority, inadequacy, the impossibility of motherhood and starting a family. The psychological mood of patients is very important for conception: if you set yourself up for failure in advance, then conception may not occur (as, incidentally, in women with a normal uterus). Problems with pregnancy also arise in the presence of concomitant disorders - for example, ovarian hypofunction, hormone deficiency, etc. A double uterus is a rare pathology, but it happens even more rarely that one or both uteruses are underdeveloped.
Double uterus and pregnancy
In most cases, a double uterus is not an obstacle to conceiving a child – but only on condition that there are no defects on the part of other reproductive organs.
When a woman becomes pregnant, she may face the following problems:
- spontaneous termination of pregnancy;
- premature birth;
- atypical position of the fetus;
- profuse postpartum bleeding.
Most often, with a double uterus, only one of the uterine organs is fully prepared for conception and gestation, while the second has somewhat weaker characteristics - it can be classified as a rudimentary organ. It is noteworthy that as pregnancy progresses, this "rudiment" also begins to increase, which occurs approximately until the fifth month, which is associated with increased hormonal activity.
For most patients, a double uterus does not pose any danger, does not impair reproductive function, and does not require medical intervention. However, pregnancy should proceed under regular medical supervision to avoid complications and disorders during the gestation process.
If a spontaneous abortion occurs, then emergency curettage of both the first and second organ is performed. [ 3 ]
In isolated cases, pregnancy was observed in two uteruses at the same time: in such situations, a woman would first give birth to one baby, and only a few weeks later to a second.
The need for medical termination of pregnancy is discussed in the following cases:
- if the embryo is not attached correctly (for example, to the interuterine septum);
- in case of hypoplasia of the uterine endometrium;
- in case of cervical insufficiency;
- when an embryo develops in a rudimentary organ that is unsuitable for implantation. [ 4 ]
Complications and consequences
The presence of a double uterus sometimes leads to diagnostic errors. As a result, incorrect treatment is prescribed, including unjustified surgical interventions such as appendectomy, tubectomy, removal of appendages, cervical canal and vaginal bougienage.
Other unpleasant consequences may include:
- difficulties with intimacy (unpleasant sensations, etc.);
- accumulation of menstrual blood in the rudimentary part of the uterus;
- infectious processes (formation of purulent cavities in the internal genital organs);
- difficulties with bearing a child (spontaneous miscarriages, premature births);
- difficulties conceiving (infertility).
Diagnostics twin uterus
The main diagnostic methods that allow detecting a double uterus are the following:
- ultrasound examination (preferably transvaginal);
- hysteroscopy, hysterosalpingography;
- magnetic resonance imaging;
- laparoscopy.
The first stage of diagnostics usually includes more accessible procedures: ultrasound and magnetic resonance imaging. But endoscopy in the form of laparoscopy and hysteroscopy are appropriate if it is necessary to combine diagnostics and treatment of the disease. In this case, it is possible not only to detect the anomaly, but sometimes also to remove the non-functioning rudimentary horn.
Instrumental diagnostics in the form of ultrasound and magnetic resonance imaging are considered the most informative, safe and accessible. They do not give radiation exposure to the body, but allow to determine precise anatomical changes in the reproductive organs. In case of complete doubling, during MRI diagnostics, two isolated uterine organs are visualized, from each of them a fallopian tube with an ovary, two isolated cervixes and two vaginas (complete vaginal septum) depart. Two cervixes and vaginas have close wall contact. Both uterine organs and vaginas can be separated from each other by the bladder and/or rectum, or touch each other by the walls. A double uterus can be completely anatomically and physiologically complete, or have an underdeveloped second half. Using T2-weighted examination, it is possible to distinguish layers of the uterus, depending on the signal intensity:
- The central hyperintense layer corresponds to the endometrium and mucous tissue that lines the uterine cavity.
- A narrow layer adjacent to the central layer, referred to as the transition region.
- The outer layer is the myometrium, which has an average signal intensity.
As additional tests, the patient is prescribed laboratory tests:
- general blood test;
- general urine analysis;
- coagulogram;
- biochemical blood test (urea, creatinine, total protein, glucose);
- hormonal studies.
The need for treatment is determined, first of all, by the presence of complaints from the patient. The doctor needs to obtain information about the quality of the woman's sexual life, whether there were attempts to get pregnant, whether there were other problems with the urogenital system (diseases, surgeries, abortions, miscarriages, etc.). The quality of the menstrual function is necessarily analyzed, the following questions are clarified:
- period of the onset of the first menstruation (at what age);
- regularity of the monthly cycle;
- profuse bleeding;
- pain at the beginning of menstruation;
- cycle duration;
- the presence of vaginal discharge in the middle of the cycle.
In addition, an examination is performed in a gynecological chair, a bimanual vaginal examination (necessary for palpation of the size of the internal genital organs, their relationship, the condition of the ligaments, mobility of the appendages, pain, etc.). [ 5 ]
Differential diagnosis
Today, there are quite a lot of modern methods of visualizing internal organs. But, despite this, the diagnosis of a double uterus can be difficult, which entails erroneous recognition of the pathology. According to statistics, incorrect diagnoses and, accordingly, incorrect prescription of therapy for a double uterus leads to unjustified surgical interventions in about 30% of cases. To avoid this, specialists recommend that, if there is a suspicion of organ doubling, mandatory MRI be performed, which allows for more accurate differentiation of diseases and provides much more information about the existing pathology.
The greatest difficulties in differential diagnosis arise with such types of uterine anomalies as complete doubling, bicornuate, presence of a septum, and saddle-shaped uterus.
Hysteroscopy and hysterosalpingography can be used to suspect an anomaly. However, these methods are not always applicable, primarily due to their invasiveness: such procedures are not used for children and young girls who have not previously had sexual intercourse. In addition, hysteroscopy and hysterosalpingography provide a picture of only the internal contours of the organ cavity, and this information is insufficient for differential diagnosis. The external contour can be examined using laparoscopy, but this method is also invasive. [ 6 ]
Among non-invasive methods for reliable interpretation of pathology, ultrasound and magnetic resonance imaging are used, allowing to evaluate both the internal and external uterine contour. Since transvaginal ultrasound is optimal, this procedure is contraindicated for children and girls before the onset of sexual activity. Therefore, preference is often given to MRI, with an analysis of the configuration in a T2-weighted image in a standard plane (coronal, drawn along the axis of the uterine body). For further differentiation, the interstitial parts of the fallopian tubes are used as control points for drawing a line between them.
Who to contact?
Treatment twin uterus
There is no need for treatment if the double uterus does not cause problems in reproductive, sexual and menstrual function, has no complications and disorders on the part of other organs. A special approach to treatment is required if the anomaly is accompanied by the accumulation of menstrual blood in the cavities of the reproductive organs. This pathology is characterized by severe pain, especially with the onset of a new monthly cycle. Some women develop infectious complications in the form of the formation of purulent inflammatory foci.
Surgical treatment is necessary if the patient has problems in the sexual aspect, problems with conception and bearing a child. The type and complexity of the intervention depend on the specific defect and its degree. In this case, surgery is the only way to correct the pathology. Surgeons usually use minimally invasive techniques, including laser technology and coagulation. One of the most common operations is hysteroresectoscopy, during which the doctor removes the septum dividing the organ into two parts.
In general, there are the following indications for surgical intervention:
- abnormal structure of the vagina that interferes with normal sexual life;
- closed rudimentary second uterus;
- underdeveloped second uterus, with a high probability of developing an ectopic pregnancy in it;
- habitual miscarriages;
- uterine septum;
- combination of double uterus and other urogynecological anomalies and pathologies.
In case of menstrual blood flow disorders, vaginal walls are dissected, contact is formed between the "working" and closed cavity, the accumulation site is opened and drained, vaginal sanitization is performed. During laparoscopy, uterine localization is examined, a procedure for emptying the site is performed, and the abdominal cavity is sanitized.
Vaginal aplasia is an indication for the use of colpoelogation (bougienage) and colpopoiesis (artificial formation of the vaginal canal from the tissue of the uterorectal serous bursa).
If a woman is found to have a thin intrauterine septum, then it is optimal to perform the Tompkins operation, which allows for the formation of a good uterine cavity. [ 7 ]
An incomplete but dense septum is an indication for the Jones operation. In order to create a single cavity in the organ, the surgeon performs a partial wedge-shaped excision of the membrane, after which he dissects its remaining parts. As a result, a sufficiently large uterine cavity is created while preserving the endomyometrium.
A bicornuate uterus with a low horn fusion is an indication for the Strassmann operation, and with a high or medium fusion, the body of the uterus is dissected under the horn fusion zone, with subsequent opening of the cavities of the first and second horns. This method of intervention facilitates recovery and reduces the trauma of the operation.
In case of complete doubling, a two-stage operation is performed, consisting of the following stages:
- dissection of the vaginal septum and formation of a single cervix;
- performing plastic surgery (metroplasty).
A complication of such an operation may be the development of isthmic-cervical insufficiency.
Prevention
There is no specific prevention of the development of a double uterus. You can limit the risk of the anomaly if you carefully prepare for pregnancy and follow all the doctor's recommendations throughout the entire period of gestation.
Experts talk about the following preventive measures:
- visit a gynecologist regularly (twice a year);
- plan and prepare for pregnancy in a timely manner (be fully examined, treat existing chronic diseases and infections);
- prevent the development of unwanted pregnancy, exclude abortions;
- register with an obstetrician-gynecologist for pregnancy in a timely manner (before the 13th week of gestation);
- During pregnancy, visit your doctor regularly (optimally once every 7-14 days, more often if indicated), and follow his recommendations;
- give up bad habits, eat normally and nutritiously, do not self-medicate, avoid intoxication.
It is ideal if a couple seeks advice from a doctor at the stage of pregnancy planning. In such a situation, the doctor has the opportunity to conduct the necessary examinations, draw up an individual plan of preventive measures necessary to create optimal conditions for the maturation of the egg, its implantation and the development of the embryo.
Forecast
Women with different types of double uterus often have concomitant gynecological and extragenital pathologies, complicating the prognosis of the anomaly. Specialists talk about a relatively high incidence of infertility and miscarriage.
The most prognostically unfavorable type of pathology is considered to be a bicornuate uterus with the fusion of the horns in the middle and in the lower third, as well as the presence of an intrauterine septum. With these defects, there is the highest probability of infertility, habitual miscarriage and premature placental abruption. With a rudimentary second uterus, an ectopic pregnancy often develops, fetal growth retardation or abnormal fetal position is detected. The birth of premature and low-weight babies requires emergency resuscitation and a long recovery period.
With an intrauterine septum, bicornuate or saddle-shaped organ, the risk of developing isthmic-cervical insufficiency in pregnant women increases.
To improve the prognosis, it is recommended to detect anomalies early, and to monitor patients during conception planning and throughout pregnancy. In order to detect possible combined defects in the development of the urogenital system, all women with a double uterus should undergo ultrasound examination of the kidneys. During pregnancy, it is recommended to hospitalize the expectant mother during critical periods: from 8 to 12 weeks, from 16 to 18 weeks, from 26 to 28 weeks.
There is no need to perform curettage of the second non-pregnant organ after childbirth. On the fourth day, an ultrasound is performed: if a hematometra is detected, a vacuum aspiration procedure is performed. [ 8 ]
However, for many patients, a double uterus does not become an obstacle to either a full sexual life or to conceiving and giving birth to a baby. However, careful gynecological monitoring during pregnancy should still be mandatory.

