Medical expert of the article
New publications
Disturbance of acid-base balance
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
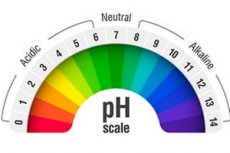
Acid-base disorders (acidosis and alkalosis) are conditions in which the body's normal pH (acid-base) equilibrium is disturbed. A healthy human body strives to maintain a certain pH level in the body to allow biological processes to function normally. When this balance is disturbed, various medical problems can occur.
There are two main types of acid-base imbalance:
-
Acidosis:
- Acidosis is characterized by a decrease in pH (increase in acidity) in the body. It can be caused by a variety of causes including:
- Metabolic acidosis: Usually associated with metabolic disorders and can occur with diabetes, kidney disease, or other medical conditions.
- Respiratory acidosis: Caused by insufficient removal of carbon dioxide from the lungs, which may be due to lung disease or impaired respiratory function.
- Acidosis is characterized by a decrease in pH (increase in acidity) in the body. It can be caused by a variety of causes including:
-
Alkalosis:
- Alkalosis is characterized by an increase in pH (decrease in acidity) in the body. Causes of alkalosis may include:
- Metabolic alkalosis: Related to excess alkaline intake or loss of acid, which can occur, for example, by vomiting or taking large doses of antacids.
- Respiratory alkalosis: Associated with excessive release of carbon dioxide from the lungs, which can occur with hyperventilation.
- Alkalosis is characterized by an increase in pH (decrease in acidity) in the body. Causes of alkalosis may include:
Acid-base imbalance can have different symptoms and complications depending on its type and cause. Treatment of acid-base imbalance is aimed at eliminating the underlying cause and restoring the body's normal pH. Treatment may include drug therapy, dietary adjustments, and other measures, and should be done under the supervision of a physician.
Causes of the acid-base imbalance
Acid-base imbalance can be caused by various reasons and factors that affect the pH level in the body. Here are some of the main causes of acid-base imbalance:
-
Metabolic acidosis:
- Diabetic ketoacidosis: If blood sugar levels are not adequately controlled in patients with diabetes mellitus, acidosis may occur due to the accumulation of ketone bodies in the blood.
- Renal insufficiency: Renal patients with reduced renal function may develop metabolic acidosis due to insufficient renal capacity to remove acid.
-
Metabolic alkalosis:
- Vomiting or gastric procedures: Loss of gastric contents due to frequent vomiting or surgical procedures can lead to loss of acidity and the development of alkalosis.
- Overuse of antacids: Prolonged use of antacid preparations that contain alkalis can cause alkalosis.
-
Respiratory acidosis and alkalosis:
- Lung Disease: Respiratory acidosis can occur with chronic lung disease that reduces the body's ability to remove carbon dioxide (CO2).
- Hyperventilation: Intense breathing or hyperventilation can cause respiratory alkalosis.
-
Loss of acidity through the kidneys:
- Prolonged use of diuretics or diuretics can lead to loss of acidity through the kidneys and alkalosis.
-
Infections and other conditions:
- Sepsis or infections can cause metabolic acidosis.
- Some genetic diseases can affect the metabolic balance of acids and alkalis.
Pathogenesis
The acid-base balance of the body is maintained at a certain level to ensure the normal functioning of physiological processes. This balance is regulated by a number of biological mechanisms, including buffer systems, lungs, kidneys and other organs. Disruption of acid-base equilibrium can occur for a variety of reasons and have a variety of pathogenetic mechanisms. Let us consider some of them:
- Respiratory acidosis and alkalosis: Respiratory acidosis occurs when there is inadequate ventilation of the lungs, resulting in an increase in blood carbon dioxide (CO2) levels and a decrease in pH. Respiratory alkalosis, on the other hand, develops with excessive ventilation, resulting in decreased CO2 levels and increased pH.
- Metabolic acidosisand alkalosis: Metabolic acidosis is usually associated with an increase in blood levels of metabolic acids (e.g., lactate, ketones) or loss of bicarbonates. Metabolic alkalosis, on the other hand, is associated with an increase in blood bicarbonate levels.
- Loss of bicarbonates or chloride: This can occur with vomiting, diarrhea, renal dysfunction, or use of diuretics.
- Renal dysfunction: The kidneys play an important role in maintaining acid-base balance by regulating the excretion of bicarbonates and hydrogen ions into the blood. Renal dysfunction can lead to metabolic acidosis or alkalosis.
- Ketoacidosis: This is a condition in which the body begins to break down fat instead of carbohydrates for energy, which can lead to the accumulation of ketone bodies and metabolic acidosis.
- Lung disease or injury: Damage to the lungs, such as pneumonia or severe chest trauma, can cause respiratory acidosis.
- Medication intoxication: Somemedications, such as aspirin or barium salts, can cause metabolic acidosis.
Symptoms of the acid-base imbalance
An acid-base imbalance (acidosis or alkalosis) can manifest itself with a variety of symptoms, depending on which way the equilibrium is shifted. Here are common symptoms associated with acid-base imbalance:
Symptoms of acidosis (increased acidity in the body):
- Fatigue and weakness: Feeling very tired and weak.
- Shortnessof breath: Difficulty breathing and feeling short of breath.
- Headache: Intenseheadaches and disorientation.
- Tachycardia: Increase in heart rate.
- Diarrhea and vomiting: Several liquid stools and/or vomiting.
- Muscle cramps:Muscle pain and cramps.
- Sleepiness and insomnia: Changes in sleep and wakefulness.
- Poor appetite: Loss of appetite or anorexia.
Symptoms of alkalosis (increased alkalinity in the body):
- Cramps: Muscle cramps and shaking.
- Burning sensation and burning pain in the mouth and throat: This may be caused by changes in the level of carbon dioxide in the tissues.
- Anxiety and Despersion: Feeling anxious and nervous.
- Tachycardia: Rapid heartbeat.
- Numbness and tingling sensation in the extremities: Similar to numbness and tingling in the extremities.
- Rapid and deep breathing: Hyperventilation and rapid breathing.
Symptoms of balance can be varied and can indicate that the body is unable to properly regulate levels of acidity and alkalinity. These disturbances can be caused by a variety of medical conditions such as respiratory disorders, kidney problems, diabetes, and other diseases.
Complications and consequences
A disturbance of the acid-base balance (ABB) in the body can have serious consequences and complications. The body's acid-base balance is maintained by important physiologic mechanisms, and shifts in acidity (acidosis) or alkalinity (alkalosis) can affect multiple organs and systems. Here are some of the possible complications and consequences of impaired GOR:
- Acidosis: Acidosis is characterized by an increased level of acidity in the body. This can lead to symptoms such as weakness, headache, nausea and vomiting. Long-term acidosis can cause damage to organs such as the kidneys, heart, and central nervous system.
- Alkalosis: Alkalosis, on the other hand, is characterized by increased alkalinity in the body. Symptoms of alkalosis can include muscle cramps, insomnia, nausea and vomiting. Long-term alkalosis can also have negative effects on organs and systems.
- Respiratoryacidosis and alkalosis: These types of ALD are related to respiratory function. Respiratory acidosis can occur due to inadequate ventilation and respiratory alkalosis can occur due to excessive ventilation. They can be caused by various conditions such as asthma, chronic obstructive pulmonary disease (COPD), trauma, or other lung diseases.
- Electrolyte deficiencies: A disorder of CSF can lead to loss or retention of electrolytes such as potassium, sodium, and calcium in the body, which can cause heart arrhythmias, muscle cramps, and other problems.
- Renal impairment: Prolonged impairment of CRP may adversely affect renal function and lead to the development of chronic renal failure.
- Neurologic symptoms: Neurologic symptoms such as seizures, insomnia, and altered consciousness may occur.
Diagnostics of the acid-base imbalance
Diagnosing an acid-base imbalance involves several steps, including symptom assessment, arterial or venous blood tests, and other laboratory tests. Here are the basic diagnostic methods:
- Assessment of clinical symptoms: The physician will begin by taking a history and assessing the patient's clinical symptoms such as dizziness, vomiting, abdominal pain, rapid breathing, and other signs. These symptoms may suggest the presence of acidosis or alkalosis.
- Blood pH measurement: The most important test for diagnosing acid-base status is to measure the pH level in arterial or venous blood. The pH of arterial blood is usually measured. The normal pH of arterial blood is about 7.35 to 7.45. Values below 7.35 indicate acidosis and values above 7.45 indicate alkalosis.
- Measurement of the carbon dioxide level (pCO2): To assess the type and cause of acid-base disturbance, the blood carbon dioxide level (pCO2) is measured. An elevated pCO2 indicates respiratory acidosis and a decreased pCO2 indicates respiratory alkalosis.
- Measurement of bicarbonate (HCO3-): Bicarbonate is an alkaline in the blood and its level is also analyzed. A decreased bicarbonate level may indicate metabolic acidosis, and an increased level may indicate metabolic alkalosis.
- Additional laboratory tests: Additional laboratory tests may include measuring electrolytes (e.g., potassium and chlorine levels), analyzing ketone bodies in the urine (if diabetic ketoacidosis is suspected), and other tests to help determine the cause of the acid-base imbalance.
- Investigations to clarify the cause: Depending on the results of the above tests and the clinical picture, additional investigations such as blood glucose levels, kidney function tests and others may be ordered to determine the underlying cause of the imbalance.
Differential diagnosis
Differential diagnosis of acid-base imbalance involves analyzing clinical findings, laboratory tests, and other methods to determine the specific cause and type of disorder. Here are some basic steps and factors that are considered in the differential diagnosis:
- Medical history and medical history: The doctor collects information about symptoms, onset, chronicity, and comorbidities. It is important to find out if there are known risk factors, such as diabetes, kidney or lung disease.
- Clinical Exam: The physician assesses the patient's general condition, including breathing, pulse, skin and mucous membranes. Examination may reveal signs of respiratory or renal dysfunction.
- Blood and urine tests: Laboratory tests such as measuring blood pH and levels of bicarbonates, CO2, electrolytes (e.g., sodium and potassium), ammonium, and lactate help determine the type and degree of acid-base imbalance.
- Blood gas study: A blood gas measurement (from arterial or venous blood) helps determine carbon dioxide (CO2) and oxygen levels, which may indicate a respiratory disorder.
- Ultrasound, X-rays, and other educational tests: Additional tests may be performed to evaluate organs such as the lungs and kidneys.
- Clinical signs and symptoms: Specific clinical signs such as breitotachypnea (deep and rapid breathing), Kussmaul breathing (deep and slow breathing), presence of acetone odor (in ketoacidosis) and other symptoms may be important in the differential diagnosis.
- Clinical Context: The clinician considers the clinical context, including patient data, medical history, and disease features.
Who to contact?
Treatment of the acid-base imbalance
Treatment of acid-base imbalance depends on the type and cause of the imbalance. It is important to make a diagnosis to determine the exact nature of the disorder and to choose the appropriate treatment. Below are some general recommendations for the treatment of acidosis and alkalosis:
Treatment of acidosis:
- Treatment of the underlying disease: The first priority is to identify and treat the underlying disease or condition that caused the acidosis. This may be diabetes, kidney disease, or some other condition.
- Restoration of fluid balance: Patients with acidosis often require restoration of fluid balance to correct dehydration and improve general condition.
- Correction of respiratory disturbances: If the acidosis is due to respiratory disturbances, correction of respiration may be necessary.
- Use of alkalis: In some cases, alkalis such as sodium bicarbonate may be prescribed to eliminate excess acidity in the body.
Treatment of alkalosis:
- Treatment of the underlying disease: As with acidosis, the first priority is to identify and treat the underlying disease causing the alkalosis.
- Correction of respiratory disturbances: If the alkalosis is due to respiratory disturbances (e.g., hyperventilation), correction of respiration may be necessary.
- Elimination of chloride loss: If alkalosis is caused by chloride loss through the stomach or kidneys, chloride replacement may be necessary.
- Discontinuing antacids: If alkalosis is caused by the use of large doses of antacids, it may be necessary to discontinue their use.
Treatment should be carried out by and under the supervision of a physician, as improper intervention can worsen the condition. Following medical advice and treating the underlying disease are important aspects of managing acid-base imbalance.
Forecast
The prognosis for acid-base balance (ABB) disorders depends on many factors, including the type and severity of the disorder, its cause, and the timeliness and effectiveness of medical intervention. In most cases, if the disorder is diagnosed and treated correctly, the prognosis can be favorable.
However, if the disorder is undetected and untreated, or if it is associated with serious illness or injury, the prognosis may be less favorable and depends on the specific situation. Here are some examples of the prognosis depending on the type of disorder:
- Respiratory acidosis or alkalosis: If respiratory acidosis or alkalosis are caused by temporary conditions such as asthma or trauma and are successfully corrected, the prognosis may be favorable. However, if they are associated with chronic lung disease or other chronic conditions, the prognosis will depend on the management of these conditions.
- Acidosis and alkalosis due to metabolic abnormalities: Disorders of CRP caused by diseases such as diabetes or renal failure may require long-term management and treatment. Prognosis will depend on how well the underlying disease is managed.
- Acidosis and alkalosis due to severe infections or trauma: If impaired CSF is associated with serious conditions such as sepsis or severe trauma, the prognosis will depend on successful treatment of the underlying condition. In some cases it may be life-threatening and intensive care is required.

