Medical expert of the article
New publications
Dejerine's syndrome
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Dejerine syndrome refers to a disease that is quite rare. It is based on genetic predisposition. Dejerine syndrome is also called hypertrophic neuropathy. It can be said right away that the disease is incurable, because all diseases caused by various mutations and changes in genes cannot be cured.
The first description of the disease belongs to the French neurologist Dejerine, who initially assumed that the disease had deep roots in genetics. He noted that the disease is transmitted from generation to generation, observed within one family. He also conducted experimental studies that allowed him to conclude that dominant genes are responsible for the transmission of the disease. Thus, in genetic counseling, it is possible to calculate in advance whether a child will be born healthy or will develop Dejerine syndrome.
Unfortunately, there is no way to prevent its development. If the disease is transmitted to the child, it will inevitably develop.
 [ 1 ]
[ 1 ]
Epidemiology
There are currently many types of Dejerine syndromes. However, they all have similar features - they manifest themselves between the ages of birth and 7 years. At the same time, approximately 20% of cases of the disease manifest themselves in the first year of life. In the second year of life, the disease makes itself known in 16% of cases.
Dejerine-Sottas syndrome is the most common. It is registered in approximately 43% of cases. In approximately 96% of cases it results in complete disability, the person is confined to a wheelchair.
The second place belongs to Dejerine-Klumpke syndrome, it occurs in about 31% of cases. The third place is given to Dejerine-Russo syndrome, the frequency of occurrence of which is about 21% of cases. At the same time, Dejerine-Russo syndrome is characterized by the formation of stable symptoms within a year in those patients who have suffered a stroke or other cerebrovascular accident in an acute form.
Pain syndrome develops unevenly. In approximately 50% of patients, pain occurs within 1 month after a stroke, in 37% - in the period from 1 month to 2 years, in 11% of cases - after a 2-year period. Paresthesia and allodynia are registered in 71% of patients.
Causes Dejerine's syndrome
The main cause of Dejerine syndrome is a gene mutation that is transmitted in an autosomal genetic manner. However, numerous genetic factors can influence the development of the pathology. They affect a person and his brain. The main causes of the disease include:
- trauma, damage, other negative effects. This is especially true for cranial nerves. The disease can also be a consequence of concussions;
- fractures of the bones located at the base of the skull;
- inflammation of the meninges, which manifests itself in an acute form. Inflammation can be of various origins. It can be caused by infectious agents, inflammation, allergic reaction. Also, the development of the syndrome can be a consequence of trauma;
- inflammation of the meninges of various origins that has become chronic;
- increased intracranial pressure.
Risk factors
There are certain risk factors that can provoke the disease. People exposed to these factors are more susceptible to the disease than others. Risk factors also include certain diseases that accompany the pathology.
The risk group includes patients suffering from brain tumors. A tumor that puts pressure on the medulla oblongata can be considered a risk factor. This group also includes various tuberculomas, vascular damage, and sarcoidosis. Brain damage occurs as a result of pressure on the brain. Damage to the brain vessels can have different natures. First of all, this concerns hemorrhagic lesions, embolisms, thromboses, aneurysms, malformations.
Also, one of the factors contributing to the development of Dejerine syndrome are such concomitant diseases as polyencephalitis, multiple sclerosis, poliomyelitis. The danger can also be posed by those diseases that are accompanied by a disruption of the normal functioning of the brain, a disruption of its blood supply. First of all, one should be wary of disruptions in the blood flow in the arterial bed. The risk group also includes patients susceptible to disruption of the blood supply to the twelfth nerve, its nucleus, medial loop, pyramid.
Syringobulbia and bulbar paralysis also contribute to the development of the disease. These factors represent a high risk, since they are characterized by constant progression.
Cerebellar tumors of various types can also be considered as a risk factor.
Congenital patients with congenital anomalies of the brain are included in risk groups. If a person with such an anomaly is exposed to infectious, toxic, degenerative agents, the risk of developing the disease increases significantly. Factors such as caustic chemicals, radioactive substances can provoke the development of pathology. They can cause a gene mutation. Therefore, women exposed to toxic, chemical substances, as well as living in a high-radiation zone, can fall into the risk group. The predisposition to the disease in this case increases sharply.
Pathogenesis
The pathogenesis of the disease is caused by a gene mutation. It contributes to the disruption of the structure of the sheaths of the trunk nerves. As the disease develops, excessive growth of the connective sheaths, which are part of the nervous tissue, is observed. As a result, the connective tissue hypertrophies, and mucous substance is deposited between the nerve connections. This leads to a significant thickening of the nerve trunks, spinal roots, and cerebellar tracts. Their shape changes. Degenerative processes affect the nervous tissue and spinal nerves.
Symptoms Dejerine's syndrome
Dejerine syndrome can manifest itself in completely different ways. It is important to understand that there are many varieties of this disease, and each of them manifests itself with absolutely different signs. Therefore, it makes sense to talk about the signs characteristic of each individual type of this syndrome.
However, there are a number of early signs that can generally indicate the likelihood of a child developing a pathology. In the early stages, different types may have many similar features.
First signs
In most cases, the disease is already fully manifested in preschool age. However, its first signs can be suspected almost from the birth of the child. If the child develops more slowly than his peers, this may be the first alarming sign. It is necessary to pay special attention to the child who does not sit at the appropriate age, takes the first step late, begins to move independently.
The child's appearance can also say a lot. Usually, the child's facial muscles are drooping. The arms and legs gradually begin to deform. They become less sensitive, practically do not react to anything. This condition can constantly worsen, until the muscles atrophy.
As soon as the child begins to develop incorrectly, you need to see a doctor. A consultation with a neurologist is necessary.
During the examination, the doctor discovers additional signs that indicate the syndrome. Fibrillary twitching of the muscles is observed. Many tendon reflexes are not manifested. The pupils may be constricted and in most cases do not react to light. The doctor confirms signs of weakening of the facial muscles.
Stages
There are mild (initial) stages, moderate and severe stages. The initial stage is when the first signs of the disease appear. This stage usually occurs in infancy.
The middle stage is a pronounced delay in speech and motor development, various motor disorders, impaired sensitivity, loss of some reflexes, and impaired visual reactions.
Severe stage – sensorineural hearing loss, skeletal deformities, muscle tone disorders, nystagmus. Disease progression. Ends in disability.
Forms
There are a great many varieties of Dejerine syndrome, depending on the type and severity of the lesion. The most common are alternating syndrome, Dejerine-Sotta syndrome, Dejerine-Klumpke syndrome, Dejerine-Rousset syndrome.
 [ 21 ]
[ 21 ]
Dejerine's alternating syndrome
If a child has alternating syndrome, the tongue is the first to be paralyzed. Moreover, not the entire tongue is affected, but only part of it. Hemiparesis develops on the opposite side. Sensitivity to vibration reaches deep layers. The child practically does not distinguish tactile sensations. The cause is thrombosis or occlusion of the basilar artery. This is what disrupts the innervation and blood supply to the medulla oblongata.
Dejerine Klumpke syndrome
In Dejerine-Klumpke syndrome, the lower branches of the shoulder joint are paralyzed. Not the entire limb is paralyzed, but only part of it. Paresis and paralysis of the hands gradually develop. The sensitivity of the corresponding areas is sharply reduced. The condition of the vessels changes. Pupillary reactions are abnormal.
The paralysis gradually spreads to the deep layers of the muscular framework. Severe numbness is observed. First the hands go numb, then the forearms, elbows. In severe cases, even the thoracic nerve can be affected. Numerous ptoses and mioses also develop.
Dejerine Roussy Syndrome
This syndrome is characterized by damage to the perforating arteries. Also damaged are areas around the artery, and those areas of the brain that are innervated by the affected artery. This syndrome is also called chronic pain syndrome, or thalamic (post-stroke) pain syndrome.
This name is explained by the fact that the syndrome is accompanied by intense pain, constant, piercing. The pain is often unbearable. The disease is also accompanied by a feeling of aches, twisting of the whole body. Hyperpathy is also observed, as a result of which some muscles come into excessive tone. However, sensitivity is sharply reduced. Also, the disease is characterized by attacks of panic, unnatural crying, screaming, or laughter.
In this case, damage is predominantly limited to one side. This could be one leg or one arm. In the affected areas, severe pain and a burning sensation are primarily observed. The pain exhausts the patient. It can be aggravated by various factors. Pain can be aggravated by both positive and negative emotions. Pain can also be aggravated by heat, cold, and various movements.
Often the disease is difficult to differentiate, to separate from other diseases. It has many signs similar to other neuralgic lesions. Sometimes it can be finally established only after the pain syndrome has fully formed.
Dejerine Sottas syndrome
Dejerine-Sotta syndrome is a type of disease. The disease is genetic. In the course of this disease, the thickness of the trunk nerves is impaired. The disease can be diagnosed at the earliest stages of pregnancy using genetic counseling. At birth, the child is no different from a healthy child. Then, as it grows and develops, it becomes noticeable that the child is developing very slowly. Poor movements, speech is not formed. The muscles are very relaxed, the child is not able to hold the head, neck, body. Visual reactions are impaired. The child lags very behind his peers in development. Sensitivity decreases progressively, the muscles gradually atrophy. Full development does not occur. Gradually, atrophy passes to the skeletal system. It ends in disability.
Neri Dejerine syndrome
In Neri Dejerine syndrome, the posterior roots of the spinal cord are constantly irritated. The cause of this is osteochondrosis, various tumors that affect the brain and press on it. Hernias, pinching, injuries also contribute to pressure on the roots. In addition, this can occur due to strong bone growths. The main manifestation is severe pain in the place where pressure occurs on the brain and its roots.
In most cases, this syndrome is not the main one, but a concomitant one, with various other pathologies and diseases. For example, it traditionally accompanies osteochondrosis. A distinctive feature is a sharp pain in the lumbar region, and a nagging pain in the neck and head, which does not allow a person to completely lift his head from a lying position. Gradually, this area hardens, sensitivity is gradually lost. Muscle spasm is also observed. Gradually, the limbs undergo pathological changes.
Landouzy Dejerine syndrome
A synonym is myopathy. The name of the disease indicates a weakening of the muscles, which is constantly progressing. In parallel, the development of various pathologies in the muscles, dystrophic processes is observed. We can say that this is not a separate disease, but a whole group of diseases. The shoulder, scapular and facial side are affected. The disease is a genetic pathology, passed from generation to generation.
It develops in several stages. At the first stage, facial weakness develops, as a result of which the facial muscles not only weaken, but also lose shape and become distorted. As a result, the face acquires irregular, distorted features. Most often, the disease can be recognized by a rounded mouth and drooping lower and upper lips.
Gradually, the disease progresses so much that the person can no longer close his mouth. He leaves his mouth open first during sleep, then even during the day. Gradually, muscle weakness affects the muscles of the shoulder girdle.
In rare cases, the pharyngeal muscles and tongue may weaken. But this symptom has no diagnostic value and is not as pronounced as other symptoms.
At the most severe stage, a person develops weakness of skeletal muscles. First, the arms become weak, then the legs. The prognosis is disappointing - disability.
Diagnostics Dejerine's syndrome
Dejerine syndrome can be diagnosed based on the symptoms and clinical manifestations that are characteristic of the disease. In some cases, the picture is so pronounced that the disease can be suspected even based on an examination. But in reality, everything is much more complicated. Other neurological diseases can manifest themselves in a similar way. Therefore, it is important to immediately analyze the existing clinical signs, analyze the data of subjective and objective examination. The final conclusion is made based on laboratory and instrumental studies. It is also necessary to study the medical history, family history.
Tests
The diagnosis of Dejerine syndrome can be confirmed based on the analysis of cerebrospinal fluid, biopsy. As a result of the study of cerebrospinal fluid, a large number of proteins, protein fragments can be detected. They are the distinctive feature that indicates Dejerine syndrome.
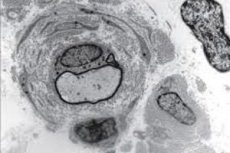
In some cases, this is enough to establish a precise diagnosis. But sometimes doubts arise. For example, if there are few protein fragments in the cerebrospinal fluid, this may indicate other neurological diseases. Therefore, in such doubtful cases, a biopsy is performed. A biopsy requires taking nerve fibers. They are taken from the elbow and calf muscles. Dejerine syndrome is accurately indicated by the presence of hypertrophy of nerve tissue. With this pathology, the sheaths of nerve fibers thicken sharply.
In addition, as a result of studying nerve tissues under a microscope, it can be established that not only the membranes thicken, but the number of fibers themselves is also significantly reduced. Demineralization also occurs. The number of nerve fibers is reduced.
Instrumental diagnostics
But sometimes there are cases when even tests are not enough to be completely sure that a person has Dejerine syndrome. Then special equipment is required. In most cases, computer and magnetic resonance imaging are used. These methods make it possible to detect how damaged the twelfth nerve is. Then, after the results are received, the doctor selects a treatment. Therapy is prescribed by a neurologist or neurosurgeon.
Differential diagnosis
The essence of differential diagnostics is to clearly separate the symptoms of one disease from another that has similar manifestations. In Dejerine syndrome, this is very important, since the further prognosis and treatment depend on it. This disease can often be confused with other neurological diseases, paralysis.
Once the diagnosis has been confirmed, it is necessary to differentiate it from other varieties, that is, to clearly determine what specific type of Dejerine syndrome we are dealing with. A biopsy and analysis of cerebrospinal fluid can help with this.
The presence of Dejerine syndrome is indicated by protein in the cerebrospinal fluid and thickened nerve fibers in a biopsy. The type of syndrome is usually determined by the clinical picture and pathognomonic signs, that is, signs that are characteristic of a particular disease, unique to it, and are its distinctive feature.
Who to contact?
Treatment Dejerine's syndrome
Since the disease is genetic, it is important to understand that it will be impossible to cure it completely and get rid of it. Most likely, the disease will progress, and it will not be possible to stop it by any means. But this does not mean that it is not worth treating. You just need to choose the treatment most carefully and rationally. It can slow down the progression of the disease, can significantly alleviate the patient's suffering.
When selecting treatment, they are guided by the fact that etiological therapy is irrational. Etiological therapy is understood as treatment aimed at eliminating the cause. For a genetic disease, it is impossible to eliminate the cause. Therefore, symptomatic therapy remains, that is, therapy aimed at relieving the symptoms of the disease, alleviating the general condition, the patient's well-being. Treatment regimens can be completely different. Everything depends on which symptom predominates, what worries the patient at the moment. In order to ensure the relief of symptoms and at the same time prevent further progression of the disease, complex therapy is used.
Complex therapy usually includes painkillers, since the syndrome is almost always accompanied by painful sensations. If there is no pain (which happens quite rarely), such drugs can be excluded.
Metabolic therapy, which improves metabolic processes, promotes better tissue nutrition, and removes metabolites, must be present. This type of treatment is mainly aimed at maintaining muscle tissue, since it is very susceptible to degenerative processes and can subsequently atrophy. The main goal of this therapy is to prevent atrophy.
It is also necessary to use drugs to improve nerve conductivity. They allow normalizing metabolic processes in the nervous tissue, restoring or maintaining the sensitivity of nerve endings, and preventing the death of receptors.
In addition to drug treatment, physiotherapy may be additionally prescribed. A course of massage, manual therapy, and various alternative therapies may be needed. Currently, there are many different orthopedic products that make it possible to prevent the development of skeletal diseases. It is also possible to prevent the development of foot deformities. Joint contractures can also be prevented with the help of orthopedic products.
Sometimes treatment can be aimed at eliminating the cause that provoked the disease. Naturally, if it is not a genetic cause. For example, in some cases, although a person has a genetic predisposition, the disease does not manifest itself. But then, as a result of some factor, the disease begins to develop or progress. Thus, the cause can be arterial thrombosis. The damaged artery compresses the adjacent part of the brain, disrupting its blood supply. In this case, it is advisable to try to eliminate the cause - remove the thrombosis. In this case, surgical intervention may be required.
In other cases, supportive, ongoing therapy is required.
Medicines
Medicines are used exclusively to eliminate symptoms. For example, to treat pain syndrome, it is recommended to use cabrazepam at a dose of 3-5 mg / kg of body weight 2-3 times a day.
Ketorolac can also be recommended at a concentration of 60 mg/day, 2 times a day. Trometamol is used at 60 mg/day, 2 times a day, ketonal - 50 mg 1-2 times a day, the maximum daily dose is 100-150 mg.
Vitamins
Vitamins are necessary to maintain the general condition of the body, to normalize the immune system, to protect against infectious and other diseases. Vitamins also help improve the general well-being of the child. The main vitamins that are necessary for the normal functioning of the body (daily dosage):
- B – 2-3 mg
- PP – 30 mg
- H – 7-8 mcg
- C – 250 mg
- D – 20 mcg
- E – 20 mg.
Physiotherapy treatment
Physiotherapy cannot cure Dejerine syndrome. But in some cases, physiotherapy can be used. It is usually used for a specific purpose. Thus, electrophoresis significantly increases tissue permeability and can be used to ensure that medications penetrate tissues faster and more effectively. Some physiotherapy procedures can reduce pain, relax muscles, and relieve spasms. They can significantly improve the overall condition of the body. Physiotherapy also helps relieve pain.
Folk remedies
There are folk remedies that help alleviate the patient's plight. It is impossible to cure Dejerine syndrome, but this does not mean that you should give up and not make any efforts to relieve or reduce the symptoms. Folk remedies help in overcoming the symptoms, relieving pain. They provide significant psychological assistance and support to the patient. The disease cannot be cured, but its progression can be slowed down.
In case of paresis, paralysis, weakening of facial muscles, it is recommended to use oats. Use green oat juice. Take a third of a glass twice a day. It is better to take before meals. The effect is general strengthening.
Paralysis and paresis are relieved by the use of mint and lemon balm. It is recommended to brew them, make a decoction and drink them warm. These herbs are relatively safe, so they can be used in large quantities, but not uncontrollably. About a liter per day is allowed. These herbs can also be added to tea to taste. Drink in unlimited quantities, to taste and mood. Usually they allow muscles to relax, and also normalize the state of the nervous system, have a calming effect.
Mint and lemon balm can also be mixed with mistletoe, approximately in equal proportions, and used as a decoction. In this case, it should be used in limited quantities, approximately 20-30 ml three times a day. This infusion helps eliminate spasms, pain, relax muscles, and calm the nervous system.
Baths with medicinal herbs have a good effect on the body. You can brew a bath from the succession. For this, about 2-3 liters of strong infusion are made separately, then it is poured into a bath of a comfortable temperature. It is recommended to take baths for 20-30 minutes. They allow you to tone your muscles, normalize the activity of the nervous system. Herbs can be combined, alternated. You can use a decoction of coniferous plants: pine, fir, cedar. You can add chamomile, linden, raspberry, nettle.
 [ 31 ], [ 32 ], [ 33 ], [ 34 ]
[ 31 ], [ 32 ], [ 33 ], [ 34 ]
Herbal treatment
If a person has impaired coordination, paresis and paralysis, ephedra herb can be used. It is used in the form of a decoction. Brew about 5 g of the herb in 500 ml of boiling water. You can drink 2-3 tablespoons three times a day.
Also, to normalize the condition of muscles, calm, relieve spasms, pain, use a decoction or infusion of valerian. Alcoholic tincture of valerian can be sold commercially. The method of administration is usually indicated on the packaging.
To prepare a decoction at home, pour about 5 g of the herb into a glass of water and drink this decoction throughout the day. You can also add it to tea.
Chamomile decoction can be used in a similar way. It additionally has an anti-inflammatory effect, normalizes the immune system and metabolism.
It is recommended to use a calendula decoction 1 tablespoon three times a day. It has an anti-inflammatory effect, relieves swelling.
Homeopathy
Homeopathic remedies can also have a positive effect, improve the general condition of the body, and eliminate individual symptoms. Side effects are rare if the dosage and methods of administration are followed correctly. It is important to consider that many substances have a cumulative effect, which means that the effect will only appear after the end of the full course of treatment, or after some time. It is necessary to observe basic precautions: consult a doctor before taking, since some substances may not be compatible with each other or with medications. The consequences can be unpredictable.
For flaccid paralysis, paresis, hyperkinesis, weakening of facial muscles, it is recommended to take Securinega sibirica. About 15 g of crushed leaves and small branches are poured with 250 ml of boiling water. Infuse until cool. Strain, take a third of a glass, twice a day.
- Collection No. 1. For lesions of the medulla oblongata, cerebellum
Take raspberry leaves, currant leaves, valerian, motherwort in a ratio of 2:1:2:1. Take in the form of an infusion, one third of a glass three times a day.
- Collection No. 2. For spastic paralysis
Take the leaves of lemon balm, chamomile, sage, and mint in a ratio of 1:1:2:2. Take in the form of an infusion three times a day, one third of a glass.
- Collection No. 3. For pain syndrome, spasms, paralysis
Take stevia leaves, nettle, common hop cones, and echinacea flowers in a ratio of 2:1:1:1. Take as an infusion three times a day.
Surgical treatment
In some cases, only surgical intervention can help. For example, if the patient has any injury, tumor, it must be removed. Thrombosis or occlusion of arteries may also require surgical intervention.
In case of pathology of blood vessels, minimally invasive intravascular surgical intervention is effective.
If a specific artery is affected, it may require surgery to improve cerebral circulation and normalize the innervation of this area.
But in some cases there are pathologies that cannot be operated. These can be various congenital anomalies, injuries.
Forecast
The course of the disease is always progressive, periods of remission are short. The prognosis is unfavorable. This is primarily due to the fact that the main degenerative processes occur in the nervous system, the brain. As the disease progresses, the ability to work is lost. Ultimately, the patient is confined to a wheelchair or bed.
 [ 39 ]
[ 39 ]

