Medical expert of the article
New publications
Deforming osteoarthritis of the knee joint
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
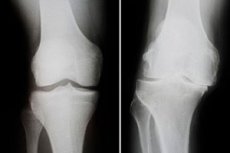
An increasing dystrophic process accompanied by changes in the bones of the knee, cartilage damage and bone-tendon degeneration is deforming osteoarthritis of the knee joint. The pathology is characterized by pain, violations of the function of the knee and its obvious curvature. Treatment of the disease is complex and complicated, sometimes surgical, involving joint endoprosthesis. Among the most frequent complications are ankylosis and progressive instability of the knee joint. [1], [2]
Epidemiology
Deforming osteoarthritis of the knee joint is diagnosed in every tenth person aged 55 and older. At the same time, every fourth of those who get the disease subsequently becomes disabled.
About 80% of patients indicate a decrease in quality of life to a greater or lesser degree.
The duration of normal function of modern types of endoprostheses a decade after surgical intervention is up to 99%, after fifteen years - up to 95%, after twenty years - up to 90%.
According to some reports, deforming osteoarthritis of the knee joint more often affects women, although this information has not been officially confirmed. [3]
Causes of the knee osteoarthritis
The primary form of deforming osteoarthritis is associated with wear and tear of cartilage tissue as part of natural age-related changes. Additional provoking factors can be:
- Excessive body weight;
- Trauma, fractures.
The secondary form of the disease is due to:
- Excessive sports activities on the knee area;
- General excessive physical activity;
- Traumatic injuries of cartilage and ligamentous apparatus, bone fractures;
- Chronic infectious-inflammatory processes that negatively affect hemostasis;
- Metabolic disorders;
- Endocrine disruption;
- Hypodynamia, trophic deficits;
- Obesity;
- Hereditary predisposition (congenital weakness of joint structures);
- Varicosis, other vascular pathologies of the lower extremities;
- Meniscus damage;
- Autoimmune diseases;
- Pathologies that negatively affect the innervation of the lower extremities (head or spinal cord injuries);
- Hereditary connective tissue diseases.
Secondary deforming osteoarthritis is often diagnosed in professional athletes - in particular, runners, skiers, skaters, and cyclists. [4]
Risk factors
- In many patients, deforming osteoarthritis of the knee joint develops after trauma (especially repeated trauma). The provoking traumatic injuries are meniscus injuries, hemorrhages, cracks and fractures, knee dislocations.
- A similar and quite common provoking factor is repeated microtraumas of the knee, for example, during sports training, constant "standing" work, etc.
- Excess weight leads to increased axial load and gradual destruction of the knee joint.
- Inflammatory pathologies such as gouty and rheumatoid arthritis, psoriasis, and spondyloarthritis often cause the development of degenerative-dystrophic intra-articular disorders.
- Another not uncommon "culprit" for the development of deforming osteoarthritis is endocrine disorders, sharp or pronounced fluctuations in hormonal balance, metabolic disorders. Such failures negatively affect the course of repair processes in the knee joint and aggravate pathological changes.
Pathogenesis
Deforming osteoarthritis of the knee joint is a common pathology that is accompanied by a failure of regenerative processes in the joint structures. In turn, this entails the early onset of aging of cartilage tissue, its weakening and thinning. Signs of osteosclerosis of the subchondral bone are detected, cysts and osteophytic growths are formed.
Primary deforming osteoarthritis of the knee affects initially normal cartilage tissue that has an innate tendency toward reduced functional adaptation.
Secondary deforming osteoarthritis occurs as a result of already present cartilage abnormalities. The primary cause of this development may be trauma, inflammatory changes in bone and joint tissues, bone aseptic necrotic processes, metabolic disorders and hormonal imbalance.
The development of deforming osteoarthritis starts against the background of changes in knee cartilage, which provides sliding of bone and joint surfaces. Trophic disorder and loss of elasticity entail dystrophic changes in cartilage tissue, its thinning and resorption. As a result, there is a gradual exposure of bone and articular tissues, sliding is impaired, joint gaps narrow, and the normal biomechanics of the joint is disturbed. The synovial sheath lacks the necessary nutrition and is subjected to constant irritation, compensatory synovitis develops. As the articular gap narrows, the articulation decreases in volume, the posterior wall of the articular bursa bulges due to the accumulation of fluid in it, the so-called Becker's cyst is formed. Further there is a replacement of delicate synovial tissue with coarse connective tissue, and the joint itself is curved. There is an overgrowth of periarticular bone structures, the formation of marginal growths, impaired blood circulation in the joint, the accumulation of underoxidized metabolic products. As a result, the peripheral sensory system suffers, there are persistent and intense pain. Due to the increasing deformation, the function of the involved musculature is disturbed, spasms and hypotrophic disorders occur, lameness appears. The knee joint experiences motor limitations, up to stiffness and ankylosis (complete immobility of the knee).
Symptoms of the knee osteoarthritis
Absolutely any type of deforming osteoarthritis is characterized by the appearance of pain in the knee joint. Pain syndrome makes itself known with joint loading and is significantly relieved without it (for example, during night rest). Pain is caused by the formation of microcracks in the trabecular bone, venous stasis, increased intra-articular pressure, damaging and irritating effect of marginal overgrowths on nearby structures, and spasm of the knee musculature.
The first signs in the form of pain are initially of short duration. They are associated with swelling of tissues, accumulation of fluid in the joint cavity, the development of inflammatory reaction in the synovial membrane. Such short-lived pain sensations occur periodically, at the time of motor activity, and proceed by the type of "jamming" at the moment of pinching the element of damaged cartilage between the surfaces of the joint.
A characteristic sign of deforming osteoarthritis is considered to be the appearance of clicking in the knee joint during its movement. Among other symptoms:
- Limitation of mobility, inability to perform flexion and extension movements;
- Increased pain with prolonged walking and climbing stairs;
- Clicking and crunching in the knee joint;
- Stiffness of movement;
- Decreased joint space;
- The appearance and growth of osteophyte growths;
- Spasm of the periarticular muscles;
- Persistent joint distortion due to degenerative processes in subchondral structures.
In addition to the knees, the disease can affect the joints of the hip, spinal column, fingers. Knee deforming osteoarthritis can be combined with other types of pathology. In this case, we talk about generalized polyosteoarthritis, in which there are numerous changes, including osteochondrosis, spondylosis, periarthritis, tendovaginitis, etc. [5]
Forms
Depending on the clinical and radiologic picture, the disease is divided into the following types:
- Deforming osteoarthritis of the knee joint of the 1st degree is characterized by a moderate decrease in motor ability, a slight implicit narrowing of the joint gap, the appearance of rudimentary marginal overgrowths. The patient may complain of discomfort and "heaviness" inside the knee, which arise or worsen after exercise.
- Deforming osteoarthritis of the knee joint of the 2nd degree is accompanied by restriction of mobility, the appearance of joint crunch during motor activity, slight atrophy of the musculature, obvious narrowing of the articular gap, significant osteophyte formations and bony subchondral osteosclerotic changes. Pain is quite pronounced, but tends to subside at rest.
- Deforming osteoarthritis of the knee joint of the 3rd degree is manifested by pronounced joint deformation, severe motor restriction, disappearance of the joint gap, intense bone curvature, appearance of massive marginal overgrowths, subchondral cystic formations, and tissue fragments. Pain is almost always present, including in a calm state.
Some authors also distinguish the "zero" degree of osteoarthritis, which is characterized by the absence of X-ray signs of pathology.
Complications and consequences
Prolonged and progressive deforming osteoarthritis of the knee joint is often complicated by such pathologies:
- Secondary reactive synovitis - inflammation of the synovial membrane, which is accompanied by an accumulation of joint fluid;
- Spontaneous hemarthrosis - hemorrhage into the knee joint cavity;
- Ankylosis - immobility of the knee due to bone, cartilage or fibrous fusion;
- Osteonecrosis - focal bone necrosis;
- External subluxation of the patella (chondromalacia and instability of the patella).
Patients should realize that deforming osteoarthritis is not just knee pain. In fact, the disease is complex and can lead to disability over time. Most patients will note in the absence of treatment:
- Curvature of the affected leg, shortening;
- Loss of the ability to perform flexion and extension movements;
- Spread of the pathological process to other parts of the musculoskeletal system (hip and ankle joints, spine);
- Disability;
- Constant pain in the knee area (both day and night).
To avoid aggravation of the problem, it is necessary to visit the doctor in time and adhere to all his appointments. In the initial period of pathology, in most cases, the process can be brought under control.
Diagnostics of the knee osteoarthritis
Both family physicians and orthopedic traumatologists are involved in the diagnosis and treatment of deforming osteoarthritis. During examination and questioning, the specialist determines the typical symptoms of degenerative-dystrophic process: palpatory soreness, motor restriction, crepitation, distortion, presence of intra-articular effusion.
Instrumental diagnosis is usually represented by radiologic examination of the knee joint. The most common X-ray signs of deforming osteoarthritis are narrowed joint gap, the presence of marginal growths and subchondral sclerosis. Computed tomography may be recommended when indicated.
Ultrasound diagnostics helps in the detection of cartilage thinning, disorders of the ligamentous-muscular apparatus, periarticular tissues and menisci, inflammatory intra-articular fluid.
Magnetic resonance imaging is particularly valuable in diagnostic terms, helping to detect cartilage, meniscus, synovial and ligamentous-bone changes, to differentiate deforming osteoarthritis from arthritis, tumors and trauma of the knee.
Diagnostic puncture and arthroscopy of the knee joint is often necessary.
Tests include general and biochemical blood tests, and analysis of synovial fluid obtained during puncture.
Recommended Laboratory Diagnostics:
- General clinical blood analysis (leukocytic formula, erythrocyte sedimentation rate, with blood smear microscopy);
- C-reactive protein (an indicator of inflammatory, necrotic or traumatic tissue damage);
- Synovial fluid for the presence of crystals in the smear;
- Chlamydia, gonococcus in the synovial fluid.
Differential diagnosis
All cases of deforming osteoarthritis of the knee joint should be differentiated with other diseases that have a similar clinical picture. Thus, it is mandatory to perform a clinical and biochemical blood test, determine the index of C-reactive protein.
In addition, the doctor may refer the patient for synovial fluid testing - to detect crystals and infection.
Differential diagnosis is made with such diseases:
- Rheumatoid arthritis;
- Gout;
- Chlamydial arthritis, gonorrheal arthritis, psoriatic arthritis;
- Spondyloarthropathy (reactive arthritis, Bechterew's disease, etc.).
Who to contact?
Treatment of the knee osteoarthritis
The treatment of deforming osteoarthritis is carried out step by step, in a comprehensive manner. First of all, it is necessary to relieve pain. To do this, the patient is prescribed nonsteroidal anti-inflammatory drugs and analgesics. The choice of a particular drug depends on both the intensity of the pain syndrome and the presence of concomitant pathologies.
After the pain is eliminated, the doctor proceeds to the possible recovery of the affected knee joint through medication and physical therapy. [6]
Physical therapy treatment may include techniques such as:
- TR-therapy - targeted contact diathermy - consists in transporting radiofrequency energy to the desired tissue zone using a special applicator. The procedure can be carried out in different modes, depending on the depth of localization of the affected tissues. Thanks to this method, eliminate swelling, stimulate lymphatic circulation, normalize the temperature in the pathological focus, improve trophics, reduce muscle spasm, which contributes to accelerated recovery.
- Tissue electrical stimulation - helps to restore blood circulation, slow down cartilage destruction. The procedure is especially effective at the 1-2 stage of osteoarthritis.
- Kinesiotherapy - involves the use of special simulators that help to eliminate muscle spasm, improve metabolism and joint mobility, restore tendon elasticity and microcirculation. During the course of kinesiotherapy, it is important to avoid overloading the affected knee, exclude prolonged walking, lifting heavy objects, jumping and running.
Other popular methods include:
- High-intensity laser therapy;
- Magnetotherapy;
- Ultraphonophoresis (ultrasound treatment);
- Drug electrophoresis (with analgesics, glucocorticoids);
- Phonophoresis (with corticosteroids);
- Therapeutic baths;
- Shockwave therapy;
- Acupuncture; [7]
- Cryotherapy.
Surgical intervention can be prescribed regardless of the stage of the disease, if a comprehensive conservative approach does not bring the expected effect.
Medications
Pain and inflammatory reaction are treated with non-steroidal anti-inflammatory drugs such as Diclofenac, Indomethacin, Nimesil. In severe pain, intra-articular injections of corticosteroids are indicated. It is possible to use Meloxicam, Lornoxicam, as well as topical application of ointments and gels with anti-inflammatory effect.
In deforming osteoarthritis of the initial degree of development, it is appropriate to take chondroprotectors, which include chondroitin sulfate, glucosamine hydrochloride, methylsulfonylmethane, hyaluronic acid or collagen type 2. The above components inhibit destructive processes in cartilage tissue and promote its regeneration. Treatment with chondroprotectors is long-term, from several months and more.
|
Diclofenac |
Anti-inflammatory, analgesic, antiaggregant and antipyretic agent. Usually prescribed 1 ampoule per day intramuscularly, or in tablets (daily dose - 100-150 mg). Possible side effects: headache, dizziness, dyspepsia, increased level of transaminases, skin rash. With prolonged use, thromboembolic complications may occur. |
|
Indomethacin |
Non-steroidal anti-inflammatory drug, a derivative of indolylacetic acid. It is taken orally after a meal, without chewing, with water. The dosage for adults is 25 mg up to three times a day. It is allowed to increase the daily dosage up to 100 mg. Administration of the drug may be accompanied by nausea, abdominal pain, digestive disorders, jaundice. |
|
Nimesil (Nimesulide) |
It is used to eliminate acute pain by 1 packet (100 mg of nimesulide) twice a day after meals. The course of administration should be as short as possible to avoid the development of complications from the gastrointestinal tract and liver. |
|
Meloxicam |
Non-steroidal anti-inflammatory, analgesic, antipyretic drug. Tablets are taken orally after meals, based on a daily dosage of 7.5-15 mg. The average course of treatment is 5-7 days. In the first days, intramuscular injections of Meloxicam are also possible, depending on the intensity of pain and the severity of the inflammatory response. Among possible side effects: nausea, abdominal pain, abdominal bloating, diarrhea. |
|
Artradol |
Sodium chondroitin sulfate preparation. It is administered intramuscularly, a course of 25-35 injections, in a dosage of 100-200 mg (with a gradual increase in dose). The course can be repeated after a 6-month break. Side effects are limited to local manifestations in the area of drug administration. |
|
Teraflex |
Glucosamine and chondroitin preparation, stimulator of tissue repair. Take 1 capsule three times a day. The course of treatment lasts 3-6 months. Teraflex is usually well tolerated, digestive disorders are rarely noted. |
Surgical treatment
The most common surgical method used for deforming osteoarthritis of the knee joint is endoprosthesis, which involves replacing the affected joint with a metal prosthesis - a constructive-anatomical analog. The operation is performed in such cases:
- If there's no gross joint distortion;
- There are no "false" articulations formed;
- No contractures or muscular atrophy.
Patients with intense processes of osteoporosis are not done endoprosthetics, as the fragile bone structure may not be able to withstand the introduction of metal pins, resulting in multiple pathological fractures.
To avoid complications, the need for a prosthesis should be decided as early as possible. The operation should be performed before contraindications arise. Endoprosthetics are most effective when performed on patients 45-65 years of age and weighing less than 70 kg.
Among the less common but organ-preserving surgeries, corrective osteotomy and arthromedullary bypass are the most commonly talked about.
During arthromedullary bypass, the femoral medullary canal is connected to the knee joint cavity using a special shunt - a hollow tube made of metal. As a result of the intervention, medullary fatty substance from the lower third of the femur is transported to the knee joint, which provides additional nutrition and lubrication.
If the patient's lower limb axis is altered and the motor volumes are not severely limited, a corrective osteotomy is performed. The operation consists of crossing the tibia, correcting its axis with further fixation in the necessary position with the help of special plates and screw fasteners. As a result of the intervention, biomechanical processes are normalized, blood circulation and metabolism in the articulation are improved.
Prevention
Compliance with certain recommendations will reduce the load on the knee joint and prevent the development of deforming osteoarthritis:
- Use a support (cane), special bandages and other devices approved by your doctor for knee injuries;
- If necessary, use an orthosis for orthopedic fixation;
- Wear comfortable shoes, if necessary, use orthopedic insoles, inserts, supinators, etc.;
- Maintain a normal weight and avoid obesity;
- Do moderate physical activity, avoiding extremes such as hypodynamia or excessive exercise;
- Avoid injury, use protective equipment (particularly kneepads);
- Consult doctors in a timely manner, do not self-medicate;
- Adhere to a work and rest regime, provide your body with a healthy sleep.
Even a small, but regularly bothering discomfort in the knee area is a reason to consult a doctor (orthopedist, traumatologist, surgeon). If a person has already been diagnosed with deforming osteoarthritis, it is important to do everything possible to curb the progression of the pathological process.
Forecast
The prognosis is determined by the stage and neglect of the pathological process, as well as the age and general state of health of the patient.
With prolonged progression of the disease, secondary reactive synovitis, spontaneous hemarthrosis, osteonecrosis of the femoral condyle, ankylosis, and external subluxation of the patella may develop.
Deforming osteoarthritis of the knee joint can seriously impair the functionality of the affected limb, leading to disability and disability. Through treatment, it is often possible to "curb" the pain syndrome and improve knee function. But, unfortunately, it is not possible to fully restore damaged cartilage tissue in adult patients. In some cases, the doctor may recommend endoprosthesis.

