Medical expert of the article
New publications
Thrombophlebitis of the deep veins of the lower extremities
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
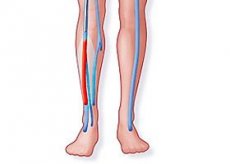
A severe pathology caused by blood clotting in the cross-section of a venule with the formation of a thrombus is referred to by doctors as venous thrombosis. In this article, we will try to consider in more detail thrombophlebitis of the deep veins of the lower extremities: the essence of the problem, the severity of the disease, the possibility of relief and the risk of complications.
ICD-10 code
In the international medical registry, deep vein thrombophlebitis of the lower extremities has its own specific code according to ICD 10, which is designated by the number I80.2, with the name assigned to it “Phlebitis and thrombophlebitis of other deep vessels of the lower extremities”.
Causes of deep vein thrombophlebitis of the lower extremities
Modern science can do a lot. But to prevent the development of the disease and to ensure that the treatment is effective, you should know the causes of deep vein thrombophlebitis of the lower extremities. Only by establishing the source can we talk about the adequacy of the measures taken, which stop not only the consequences, but also the root cause.
The main source of pathology is three criteria known as the "Virokhov Triad":
- The blood clotting level is significantly higher than normal.
- Deterioration of the condition of the walls of the vascular system.
- Congestion and slowing of blood flow.
It is worth noting that there are categories of people whose risk of developing such a disease is significantly higher:
- With age, the likelihood of vascular pathology increases.
- History of complex fractures.
- The period of pregnancy and direct obstetric care. This especially concerns women who have undergone a cesarean section.
- Obesity.
- Frequent and long trips and flights, especially with changes in climate zones.
- Extensive abdominal surgeries.
- Surgical intervention on joints.
- Infectious lesion of the body.
- Bad habits such as nicotine, alcohol, and drugs.
- Taking a number of medications that affect the coagulation rate.
- Vein injury.
- Modern food products are rich in stabilizers, colorants, preservatives, genetically modified substances, and so on.
- Prolonged immobilization, such as bed rest.
- Problems in the functioning of the cardiovascular system.
- The body's tendency to have an allergic response to an external irritant.
- If your professional activity or lifestyle requires you to be on your feet for a long time.
- Sedentary work, when the blood vessels in the back of the thigh are subject to prolonged pressure.
Pathogenesis
The mechanism of the origin and development of the disease – pathogenesis – is quite simple. When the blood flow is suddenly slowed down, a blood clot is formed, which contains red blood cells, a small amount of fibrin and platelets. One part (the leg) of the thrombus is fixed to the wall, while the other is not fixed and can move freely in the flow.
In this case, thrombus formation is progressive, bringing the size of the blood capsule to impressive parameters. The thrombus is located along the length of the blood flow. The first three to four days, this formation is weakly fixed and may break away. But after five to six days, the developing inflammation of the inner wall more reliably fixes the thrombus at the site of attachment.
Symptoms of deep vein thrombophlebitis of the lower extremities
The blockage of these vessels by a blood clot is the most common. Symptoms of deep vein thrombophlebitis of the lower extremities are:
- Increased swelling of the affected leg, as well as local changes in the shade of the epidermis in the area of the thrombus.
- The victim also begins to feel a nagging pain in the calf muscle.
- A burning and heaviness sensation appears.
- Depending on the location of the blockage, swelling can affect either a separate area or the entire lower limb.
But the insidiousness of this pathology is that it can develop asymptomatically for a long time. At the same time, venous insufficiency immediately manifests itself in complications, the consequence of which can be a fatal outcome: the higher the blockage occurs, the more dangerous the detachment of the blood capsule.
First signs
As has already been said above, quite often the patient pays attention to the problem that has arisen too late, when complications are already progressing in the body. But a person who is attentive to himself is still able to recognize the first signs of an impending pathology.
The first thing the patient may see is a slight swelling of the entire limb or a separate area on it. At the same time, depending on the status of the disease (chronic or acute form), the first signs may differ.
As medical statistics show, the pathology in question is diagnosed mainly in people over 20 years of age, and the percentage of female pathology is much higher than male.
 [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ]
[ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ]
Acute deep vein thrombophlebitis of the lower extremities
Doctors differentiate the disease by the nature of its course into acute and chronic. Acute thrombophlebitis of the deep veins of the lower extremities begins with a slight swelling, but a strong pain that spreads along the subcutaneous vein. The pathological process can affect a separate sector (calf, thigh or foot) or the entire leg.
Often the patient experiences an increase in body temperature to 38-39 °C, and sometimes even to 40 °C. The person begins to shiver. A hyperemic strip of red with a bluish tint appears along the affected blood vessel. When palpating, the doctor feels a tight tourniquet under his fingers.
If you look more closely, the specialist will recognize a change in the skin, which becomes more shiny. The swelling can add up to one to two centimeters to the leg.
After two or three days, a network of dilated vessels begins to be recognized on the surface. The patient feels that the injured leg is colder than the healthy one.
If you lift the limb, you feel a decrease in heaviness, the pain weakens, and the internal distension decreases. Gradually, the patient begins to feel general weakness. A deep breath and a coughing fit only increase the intensity of pain symptoms in the leg.
At the same time, a phlebologist, having additional symptoms, is able to specify the problem.
- Bishard's symptom is diagnosed if the patient feels sharp pain when pressing on the inside of the heel.
- The bending of the foot and sharp pain in the calf muscle is Homan's symptom.
- If, when placing a tonometer cuff on the leg (above the knee) and increasing the pressure to 45 - 50 mm Hg, an acute pain syndrome appears (the pressure decreases and the pain goes away), the doctor diagnoses the Opitz-Ramines symptom.
- The reaction to pressure on the middle of the shin is checked in a similar way. Compression indicators are brought to the mark of 80 mm Hg if the patient feels increasing pain symptoms in the calf muscle - Lowenberg's symptom.
- Moses' symptom - if when squeezing the shin with your hands (we move the ring first up and down, then to the side), a person feels pain.
The inflammatory process gradually affects the joint and ligamentous tissues of the knee. Joint mobility becomes painful.
 [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ]
[ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ]
Chronic deep vein thrombophlebitis of the lower extremities
Unlike the acute form of the disease, chronic thrombophlebitis of the deep veins of the lower extremities does not have pronounced symptoms. In the case of a chronic disease, the pain is not so intense and is periodic. Basically, the pain syndrome increases after prolonged stress on the lower extremities: prolonged walking or standing, lifting weights. Rest pain is practically not observed. Edema may be slightly noticeable.
This combination of symptoms does not frighten the patient, so he is in no hurry to see a specialist.
Consequences
Due to changes in living conditions and nutrition, modern man is increasingly faced with the disease that is discussed in this article. This especially affects industrially developed countries. Many people, feeling heaviness in their legs, attribute it to general fatigue, not rushing to see a doctor. But the consequences of such ignoring can be very deplorable.
- A favorable outcome is possible and the blood clot will dissolve on its own. The duration of this process depends on the individual characteristics of the organism, the size parameters of the phlebolith and the diameter of the vessel's flow section.
- Partial clearance of the lumen is possible.
- Overgrowth of the vein passage cavity by the proliferation of connective tissue.
- But the most dangerous of the consequences of deep vein thrombophlebitis of the lower extremities is pulmonary embolism - blockage of the pulmonary artery or its branches by phleboliths. A complication that is dangerous not only for the health, but also for the life of the patient.
- Stroke or heart attack. After originating in a vein, the clot can break away from the mucous membrane and begin its migration, carried by the bloodstream. Depending on which vessel it enters (brain capillaries or coronary arteries), the thrombus can cause a stroke - a rupture, spasm or blockage of one of the brain vessels - or a heart attack.
- Along the blood flow in large vessels there are special valves that help move fluid along the channel from the legs to the heart. Cases of damage or complete elimination of valves at the time of thrombus resorption are quite common. Such development of pathology definitely leads to venous insufficiency. Its appearance results in such symptoms as swelling of the extremities and a feeling of heaviness.
 [ 17 ], [ 18 ], [ 19 ], [ 20 ]
[ 17 ], [ 18 ], [ 19 ], [ 20 ]
Complications
The greatest danger is posed by a detached thrombus. A floating clot can provoke a massive thromboembolism, which leads to the inevitable death of the organism and the person. This is perhaps one of the most severe complications of the disease in question.
Another scenario of development is also possible. For example, complications such as:
- A marked increase in blood flow pressure in the pulmonary artery, the digital values of which are 40 mm Hg and more, which develops pulmonary embolism.
- A similar situation, only thromboembolism of smaller branches of the pulmonary artery. Such a picture of pathology is usually accompanied by breathing problems, which together lead to a heart attack - pneumonia.
- Another complication of the pathology under consideration is chronic venous insufficiency, which turns the patient into an invalid. It develops on the basis of post-thrombophlebitic syndrome.
- One of the consequences of acute thrombophlebitis in the legs is blue phlegmasia, caused by the blockage of almost all large vessels of the lower extremities.
- Most phleboliths are infected and are a source of infection throughout the body. The development of phlegmon, suppuration, etc. is provoked, including foci of sepsis and progression of metastases.
- In the acute form of the disease, unbearable pain appears, the swelling grows almost before our eyes, sometimes increasing the size of the limb by two or three times. If no help is provided, there is a further increase in the cross-section of the subcutaneous veins, the epidermis turns pale, acquiring a purple tint, the temperature indicators of the injured leg drop. A liquid substance with an unpleasant odor begins to be released from the petechiae, which indicates infection of the wounds. Against this background, shortness of breath appears, the heart rate increases sharply. This entire pathological picture, if emergency measures are not taken, leads to the development of sepsis, hypovolemic shock, and in some cases to gangrene.
Diagnosis of deep vein thrombophlebitis of the lower extremities
A consultation with a qualified doctor will allow you to somewhat narrow down the set of tools necessary for the correct diagnosis of the disease. Diagnosis of deep vein thrombophlebitis of the lower extremities is a set of studies that allow you to clearly determine the disease, excluding other pathologies.
- Initial examination by a specialist.
- Duplex scanning is an ultrasound examination session with a parallel black and white image of the state of the vessels, with moving blood flow. Such clarity makes it possible to identify the sites of blockages and vascular insufficiency. If there are no blockages, but there are clearly visible parietal thickenings, this indicates occlusive thrombosis. It does not pose a particular danger and does not threaten to break off. But if the thrombus has a tail attached to the wall and a head that moves freely in the blood flow. Such blockage is called floating thrombosis - it is very dangerous for the health, and sometimes even the life of the patient. At the same time, there is a high probability of the transition of the first type of pathology to the second. This can happen if adequate therapeutic measures are not taken against the background of further growth of the clot.
- Radiocontrast phlebography is an X-ray of the lower extremities that allows examining the patient's deep veins. The procedure is performed using a radiocontrast substance injected into the venous system. The most informative study. It is prescribed if there are doubts about the objective reliability of the duplex examination. This is especially relevant in the case of a clot localized in the groin area.
- If answers to all questions are not received, the doctor may prescribe additional examination in the form of magnetic resonance imaging (MRI) or computed tomography - angiography.
- A test is performed to determine the level of D-dimer in the blood. If it is higher than normal, this confirms the presence of a thrombus in the body.
- If a specialist has reason to suspect pulmonary artery thrombophlebia, they prescribe a chest X-ray. Most often, they use scintigraphy with a radioactive marker. Only on the basis of this study and the results of duplex scanning can we talk about the presence or absence of pulmonary embolism.
- In addition, the following may be prescribed: electrocardiogram (ECG) and echocardiography (ECHOCG).
- Monitoring of blood pressure values is mandatory.
 [ 23 ], [ 24 ], [ 25 ], [ 26 ], [ 27 ]
[ 23 ], [ 24 ], [ 25 ], [ 26 ], [ 27 ]
Tests
When establishing a diagnosis, one cannot do without laboratory test results. The main tests that are necessary to obtain a complete picture of the pathology are clinical blood tests. The doctor is interested in the leukocytosis index, as well as the ESR level.
It would also be desirable to tell:
- Analysis of C-reactive protein - a glycoprotein produced by the liver and related to the components of the acute phase of inflammation. Its prolonged high values indicate an inflammatory process affecting the walls of blood vessels.
- Obtaining a thromboelastogram is a method of graphically recording the processes of coagulation and fibrinolysis occurring in the blood.
- Determination of the prothrombin index level allows one to assess the state of the blood coagulation system.
But, as sad as it may sound, the volume of analyses performed is sometimes limited by the capabilities of the laboratory of the institution where the patient is being examined.
 [ 28 ], [ 29 ], [ 30 ], [ 31 ], [ 32 ]
[ 28 ], [ 29 ], [ 30 ], [ 31 ], [ 32 ]
Instrumental diagnostics
Having received the results of laboratory tests, it is quite difficult to diagnose the disease. The most informative for making the diagnosis in question is instrumental diagnostics. Modern medicine offers doctors a whole range of various tools that allow not only to visualize the problem, but also, having processed the data, to issue detailed indicators of the patient's body condition. With the help of innovative methods, a specialist gets a complete picture of the condition of the subcutaneous deep veins and valves, characteristics of the flow section of the bed and other components.
Such methods of modern medicine include:
- Ultrasound angiography of the extremities is a fairly fast and informative diagnostic method. Its essence lies in the ability of cells to receive and reflect ultrasound waves. It is performed using a contrast agent injected into the bloodstream.
- Phleboscintigraphy - the study is carried out using radionuclide isotopes. The method is highly informative and shows high accuracy in determining the location and nature of the pathology.
- Ultrasound Dopplerography is a method of examination based on the Doppler effect, the essence of which is that a moving liquid reflects waves with a variable frequency that hit it. This shift in the readings of the incoming and reflected wave is directly proportional to the speed of blood flow.
- Phlebography is a method of examining the patient's venous system using a contrast iodine-containing substance; the blood filling of large veins is recorded.
- Multispiral computed tomography.
- Magnetic resonance imaging. The last two methods are the most innovative and informative. But due to their high cost, they are prescribed only if other methods have not provided an unambiguous diagnosis.
- A chest X-ray is ordered if doctors suspect that a pulmonary embolism is developing in the patient's body.
Timely diagnosis, at the early stages of development, and correct establishment of the disease make it possible to carry out the most effective therapy.
Differential diagnostics
As practice shows, a number of diseases can have similar symptoms. Therefore, only having received a complete clinical picture of the pathology and the results of various studies, can we talk about making the correct diagnosis. Differential diagnostics allows, based on the available results, to determine the disease, excluding those that are similar in symptoms.
Having such a clinic, when conducting an examination, the doctor must exclude the following pathologies:
- Cellulite is a degenerative-dystrophic disorder of the dermis and subcutaneous fat.
- Rupture of a synovial cyst (Baker's cyst), the symptom of which is the appearance of a formation filled with synovial fluid behind the knee joint, which an inexperienced person may mistake for swelling.
- Lymphedema is swelling of the lymph - accumulation of fluid in the lymphatic vessels.
- Stretching or tearing of muscle tissue, with associated symptoms.
- Compression of a blood vessel from the outside: by a neoplasm or enlarged lymph nodes.
Who to contact?
Treatment of deep vein thrombophlebitis of the lower extremities
Depending on the differentiation of the diagnosis and the severity of the disease, the doctor raises the question of the patient's medical examination or outpatient management of the problem. Treatment of deep vein thrombophlebitis of the lower extremities involves the use of special ointments, after which compression bandaging or wearing special compression stockings is mandatory.
Not the least important place is given to therapeutic physical training, as well as precisely selected physiotherapeutic procedures.
Such patients are recommended to undergo spa treatment in balneological centers or specialized mud baths.
But if floating thrombosis is diagnosed, surgery will most likely be prescribed. A vascular surgeon will perform the most effective operation for this clinical picture:
- Removal of dangerous phlebolith.
- Ligation of the affected venule.
- Vein plication - a method of surgical prevention of pulmonary embolism.
- Reconstructive surgery for arteriovenous bypass grafting.
- Installation of a cava filter - a medical device implanted into the flow section of a blood vessel in order to trap blood clots carried by the bloodstream.
Medicines
The protocol of medical therapy depends on the differential affiliation of the pathology. The occlusive nature of the disease is stopped conservatively. The choice of medicine is determined by the pathogenesis of the problem. Therefore, the first thing the doctor does is prescribe drugs to the patient that belong to the group of anticoagulants, that is, agents that reduce coagulability, which is a therapeutic and preventive measure against the formation of blood clots. Basically, this is heparin and its derivatives.
The drug is used intravenously and subcutaneously. Intramuscular administration is not recommended due to the risk of hematoma formation.
The starting dose for intravenous administration is 5000 IU. The drug is used after dilution in isotonic NaCl solution. Repeated injection is performed every four to six hours. If necessary, the dosage can be doubled.
This drug is contraindicated in cases of individual intolerance to the components of the drug, hemorrhagic diathesis, bleeding of any nature, impaired kidney and liver function, leukemia, etc.
This medicine is used only in a hospital setting, under constant supervision of a doctor, as there is a high risk of bleeding.
Modern pharmacology offers low-molecular heparins, which are more convenient to use. The patient can make injections independently, and there is no overdose. Such drugs do not cause complications. These include: fragmin, warfarin, fondaparinux, fraxiparin, clexane, sodium idraparinux, coumadin.
Ointment for thrombophlebitis
It is worth noting right away that self-prescribing medications is not recommended. Only a specialist can prescribe the necessary ointment for thrombophlebitis. This can be a medicine made on the basis of heparin: hepanol or heparin ointment, troxevasin. Such an ointment, when applied externally, has an anti-inflammatory and analgesic effect. Penetrating into deep tissues, it prevents the formation of clots and increased blood clotting.
The drug is applied to the sore spot in a thin layer with a little rubbing. This procedure is repeated two or three times a day. To increase the effectiveness of the therapy, tightening bandages with ointment applied to the bandage are applied. It is advisable to do this at night, placing a folded blanket or pillow under the sore limb. The duration of the treatment is two weeks.
The treatment protocol for the disease in question also includes non-steroidal anti-inflammatory ointments: Nise, Indovazin, Nurofen gel, Diclofenacol gel.
These ointments block the production of prostaglandins, suppressing the development of inflammation, while they have analgesic and anti-edematous properties.
The medicine is carefully applied to the affected area. The procedure is repeated two to three times a day. They are strictly prohibited for use as compresses. The duration of therapy is from seven days to two weeks.
It should be clarified that the ointments under consideration for thrombophlebitis are less effective than their use in the case of superficial inflammation. Therefore, they are often used in tandem with tablets taken orally.
Folk remedies
We should not brush aside the experience of our ancestors. Traditional medicine can be very effective, but under one condition: the recipe that the patient plans to use to relieve the problem must be approved by his attending physician. This is the only way to avoid a situation where the treatment does more harm than good.
We are ready to offer several recipes that will significantly improve the situation:
- To prepare a decoction that is drunk throughout the day, take a tablespoon of dried and crushed verbena flowers. Pour a glass of just boiled water into the grass and leave until cool. Strain and take.
- Applications with bodyaga are also effective. The composition is prepared by infusing two tablespoons of powder and 0.5 liters of boiling water. Infuse. Compresses using the resulting tincture should be done in the morning and evening, holding on the affected area for about an hour and a half.
- Prepare a mixture by taking equal amounts of: plantain leaves, raspberry roots, chamomile flowers, white willow bark, horse chestnut fruits and rue flowers. Grind and mix all ingredients. Take two tablespoons of the mixture and pour into 0.5 liters of boiling water. Place the infusion in a dark place, where it will be infused for 24 hours. Take it in the morning and before bedtime, 150 mg.
 [ 37 ], [ 38 ], [ 39 ], [ 40 ], [ 41 ]
[ 37 ], [ 38 ], [ 39 ], [ 40 ], [ 41 ]
Leeches for deep vein thrombophlebitis
Hirudotherapy has not lost its relevance with the advent of new technologies and treatment methods. Leeches for deep vein thrombophlebitis are used for any type of disease. Modern statistics show fairly high results in the use of leeches in therapy, up to complete recovery.
For greater efficiency, they are placed on both sides of the affected area (a couple of centimeters from the vein). The distance between the worms is 5-6 cm. They are not placed directly under the knee because in addition to the veins, lymph nodes are also concentrated there. Usually, 6 to 15 bloodsuckers are needed for one session.
It is strictly forbidden to carry out this procedure on a patient with a developing purulent process.
Herbal treatment
Folk recipes for the disease in question should be used only as auxiliary means of therapy, in parallel with the main treatment. Herbal treatment is acceptable. It is assumed that they can be used as decoctions taken internally, as well as lotions and applications locally.
In such a situation, herbs with anti-inflammatory, analgesic and anticoagulant effects are used. Tinctures of both individual medicinal plants and their collections are effective. The most frequently used herbs in the recipe for deep vein thrombophlebitis are: wormwood, chamomile, flax seeds, plantain, sweet clover, rue, marsh cudweed, horse chestnut, lilac, calendula, St. John's wort, sage, marshmallow root.
Homeopathy
Modern alternative medicine allows for replacement therapy of many diseases. It also finds its response in the treatment of the disease discussed in this article. It is worth noting right away that homeopathy requires the abolition of other methods in its treatment, which is unacceptable in the complex treatment of deep vein thrombophlebitis, which often includes both surgical and therapeutic treatment.
A homeopathic doctor prescribes several medications, which are taken alternately every 14 days.
Orally, the following can be prescribed: peonia plus, venoflebin, edas 120, venosan, esculus compositum and iov venum. For local treatment, ointments applied to the dermis are used: edas 203 or venoflegel.
Many are confident that even long-term use of homeopathic medicines does not harm the body and does not provoke the development of an allergic reaction.
Such drugs are presented on the modern market in the form of injection solutions, granules and ointments. It is the solutions that are considered the most effective when administered intradermally.
In addition to the drugs that work directly on the problem that has arisen, drugs that improve liver function are usually prescribed in parallel, which is important in the current situation. This may be one of the drugs: artrosan, edas 919, solvency, artris clinic.
Medicines of this group are taken half an hour before or after meals. If the medicine is prescribed in the form of granules, they are placed under the tongue until completely dissolved. They should not be washed down with water.
During homeopathic treatment, you should avoid drinking coffee, strong tea, alcohol, and various spices and herbs.
Surgical treatment
Surgical intervention is also used in the treatment of this disease. But surgical treatment is recommended only in the case of diagnosing a severe form of thrombosis, when there is a high probability of its detachment, migration, and also when there is a risk of cell necrosis. In this case, the operation is called thrombolyticectomy.
Surgical intervention is usually performed through a small incision (up to 1 cm), which classifies this procedure as low-trauma. Innovative techniques allow the surgeon to monitor the progress of the operation on a special monitor, the sensor from which passes along with the instrument to the work site. The patient undergoes the procedure under spinal anesthesia. After the operation, the patient spends two to five days in the hospital.
There are several types of surgical intervention:
- If the patient has contraindications to the use of anticoagulants, a cava filter is implanted. It is placed in the affected blood vessel, allowing free blood flow. This innovative method allows preventing the formation of phleboliths and their migration in the future. The disadvantage of this method is the fact that if the thrombus breaks off and blocks the filter itself, the blood flow deteriorates sharply. Which requires emergency surgery.
- The inferior vena cava is sutured if it is not possible to implant a filter. And also in case of multiple thrombi or relapse of the disease. In this case, a "clip" (a special clamp) is applied to the affected area of the vessel and sutured. This allows you to partially block the channel, leaving a certain lumen for blood flow. The disadvantage is the deterioration of blood outflow from the veins of the lower limb.
- Endovascular catheter thrombectomy. This procedure involves clearing the vessel of phleboliths and returning the vessel to normal blood flow. The essence of the process is the introduction of a flexible tube into a narrow incision, through which the thrombus is extracted or crushed. It is prescribed in case of ineffective therapeutic treatment, the presence of oncological pathology and the impossibility of installing a cava filter. The disadvantage of the procedure is the high risk of relapse.
After performing surgery (any of these), you should wear a compression bandage or stockings. However, for the first three days, you are not allowed to remove them at all, since there is a high probability of new phleboliths forming.
Diet for deep vein thrombophlebitis of the lower extremities
The products that are on our table play an important role in preventing the disease or the patient's quickest recovery. This is especially true when the problem already exists and there is a need to stop it. The diet for deep vein thrombophlebitis of the lower extremities comes down to some recommendations given by a vascular disease specialist.
Every day, a person's diet should include at least one of these products: ginger root, melon or watermelon, cinnamon, onion or garlic. It is advisable to consume these products fresh, but you should not ignore their processing in a certain dish.
It is desirable if the overwhelming majority of the dietary products are plant components. Less often - lean meats and fish. At the same time, it is necessary to ensure that the daily menu is complete and balanced in fats, carbohydrates and proteins.
You need to remove from your diet:
- Fish, fish products, seafood.
- Meat of animals and poultry.
- Bananas.
- Products of the legume family.
- Black currant.
Prevention
Almost any disease can be prevented, but to achieve this, you need to make certain efforts. Prevention of deep vein thrombophlebitis of the lower extremities is divided into primary, which, in principle, should reduce the risk of developing this pathology, and secondary - reducing the likelihood of worsening the situation or relapses after the disease has been diagnosed.
Primary activities:
- Healthy lifestyle.
- Giving up bad habits.
- Emotional stability. Conflicts and stress should be avoided.
- Avoid putting excessive strain on your legs.
- Avoid hypodynamia. Movement, within reasonable limits, is life.
- If you suspect a pathology, seek early consultation with a doctor.
- Drink enough fluids.
- Reconsider your eating habits.
Secondary:
- As prescribed by your doctor, take blood thinning medications.
- Use a tight bandage on the affected area: an elastic bandage or a special stocking.
- A set of special exercises.
- Visiting balneological resorts or specialized mud baths.
Forecast
Analyzing statistics and monitoring the development of pathology, it is very problematic to make an unambiguous prognosis. If the disease was recognized at an early stage of development, then timely adequate treatment leads the patient to complete recovery.
If the process is started, then, as the same statistics show, approximately every fifth case develops into pulmonary embolism. If emergency aggressive anticoagulant therapy is not performed, 10 to 20% of patients diagnosed with pulmonary embolism die. If therapy is performed, the risk of mortality decreases by 5 to 10 times.
In modern society, due to a sedentary lifestyle, diet, constant stress, deep vein thrombophlebitis of the lower extremities is not uncommon. It brings many unpleasant moments to its owner. At the same time, ignoring the problem can negatively affect the functioning of the entire body as a whole, leading to serious complications, and sometimes even death. Therefore, you should not ignore the problem, it must be solved as soon as possible. But self-medication is also unacceptable. Trust this process to a qualified specialist. Only in this case can you count on a positive result.

