Medical expert of the article
New publications
Coronary circulation
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The coronary circulation (or coronary circulation) is the system of blood vessels that supplies blood and oxygen to the muscles of the heart, called the myocardium. Myocardium is the heart muscle tissue that makes up the walls of the heart and allows it to contract and pump blood throughout the body.
The coronary vessels, called coronary arteries, are responsible for supplying blood to the myocardium. They are located on the surface of the heart and within its tissues.
Coronary arteries
These are the vessels that supply blood to the myocardium (heart muscle). Coronary arteries are located on the surface and inside the heart and play an important role in supplying the heart muscle with the oxygen and nutrients it needs to function properly. The major coronary arteries are listed below:
-
Left Coronary Artery (LCA):
- Left Anterior Descending Artery (LAD): This branch of the LAD runs down the front side of the heart and provides blood supply to the anterior and superior myocardium.
- Left Circumflex Artery (LCx): The LCx originates from the LCA and provides blood supply to the posterior and left lateral side of the myocardium.
-
Right Coronary Artery (RCA):
- The right coronary artery begins on the right side of the aorta and provides blood supply to the right side of the myocardium and the back of the heart.
These coronary arteries branch out and form a network of small vessels and arteries that penetrate the myocardium and supply its cells with oxygen and nutrients. Coronary arteries are critical to normal heart function, and their blockages or bottlenecks can cause heart problems, including angina (chest pain) and myocardial infarction (death of part of the heart muscle).
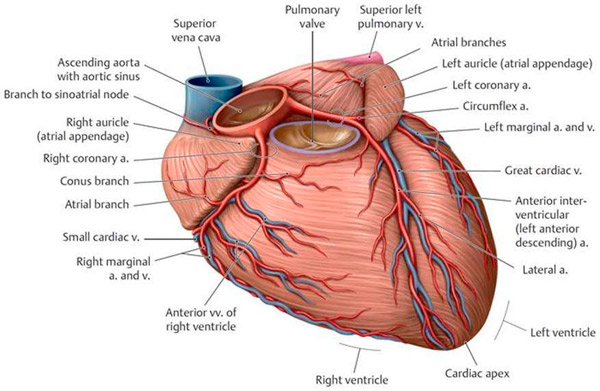
Coronary veins
This is a network of veins that is responsible for collecting and draining waste blood from the heart muscle (myocardium) into the right atrium of the heart. They play an important role in blood circulation and provide oxygen and nutrients to the heart.
The major coronary veins include:
- Great Cardiac Vein: This vein runs along the anterior wall of the left ventricle of the heart and collects blood from the anterior part of the myocardium.
- Small Cardiac Vein: This collects blood from the lower right ventricle and the upper right ventricle and upper right atrium.
- Middle Cardiac Vein: This runs along the back wall of the heart and collects blood from the back of the myocardium.
The coronary veins merge within the heart to form the Coronary Sinus, which drains into the right atrium. It is important that these veins ensure the efficient collection and drainage of waste blood, because the proper functioning of the coronary veins not only provides oxygen to the heart, but also removes metabolic waste products and waste products that are produced in the myocardium during its work.
Coronary vein disease and coronary vein disease can lead to serious heart problems such as coronary heart disease (CHD), angina and myocardial infarction. These conditions may require medical intervention, including angioplasty and coronary artery bypass grafting procedures, to restore normal blood flow to the heart.
Functions of coronary vessels
Coronary vessels, also known as coronary arteries, perform important functions in the body related to supplying blood and oxygen to the heart muscle (myocardium). Here are the main functions of the coronary vessels:
- Oxygen and nutrient delivery: The coronary vessels are responsible for delivering oxygen and nutrients to the myocardium (heart muscle). The heart muscle needs a continuous supply of oxygen and energy to do its job of contracting and pumping blood throughout the body.
- Blood flow regulation: The coronary vessels are able to dilate and constrict according to the needs of the myocardium. This regulation of blood flow allows the supply of oxygen and nutrients to be adapted to the heart's activity level.
- Ensuring proper heart function: The coronary vessels provide an adequate blood supply to the heart itself, including its own myocardial cells, so that the heart can contract effectively and maintain blood flow.
- Protection against atherosclerosis: Healthy coronary vessels are able to contain the development of atherosclerosis (accumulation of cholesterol and other substances on the walls of the arteries). However, they can fall victim to atherosclerotic processes, which can lead to coronary artery obstruction and coronary heart disease.
The coronary vessels are critical to the health and function of the cardiovascular system. Any impairment of their function, such as stenosis (narrowing) or blockage, can lead to serious cardiac problems including angina pectoris, myocardial infarction and heart failure. Therefore, it is important to maintain healthy coronary vessels, follow a healthy lifestyle and control risk factors such as high blood pressure and cholesterol levels.
Coronary blood flow is critical for normal heart function. When the heart contracts, it needs enough oxygen and nutrients, which are supplied through the coronary arteries. If the coronary arteries become narrow or blocked, this can lead to myocardial ischemia (lack of blood supply), which can cause angina (chest pain) or myocardial infarction (death of part of the heart muscle).
Physiology of the coronary circulation
Includes processes that ensure normal blood supply to the myocardium (heart muscle). Blood flow in the heart muscle is somewhat different from that of other organs and tissues in the body because of its special function and high energy requirements. Here are the key aspects:
- Autoregulation: Coronary arteries have autoregulatory mechanisms that allow them to automatically adjust their diameter and blood flow in response to changes in myocardial oxygen and nutrient needs. When the myocardium needs more blood supply, the arteries dilate, providing more blood and oxygen. At rest, the arteries may narrow.
- Diastolicperiod: The main blood supply to the myocardium occurs during the diastolic phase of the cardiac cycle, when the heart is relaxed and the chambers are filled with blood. At this point, the arteries can receive more blood and oxygen because they are not compressed by the myocardium.
- Arteriovenousanastomoses: Arteriovenous anastomoses exist in the myocardium, which are connections between arteries and veins. They can serve as reservoirs of blood and provide additional blood supply under conditions of increased stress on the heart.
- Autonomic nervous system: Sympathetic activation (activation of the stress response) can increase blood flow to the myocardium, increasing cardiac output and dilating the coronary arteries. However, with strong sympathetic activation, coronary arteries may also narrow.
- Endothelium and Nitric Oxide: The endothelium (inner layer of the vascular wall) of the coronary arteries produces nitric oxide, which helps dilate the arteries and maintain a normal blood supply to the myocardium.
These physiological mechanisms allow the heart to receive sufficient oxygen and nutrients at different times of activity and rest, ensuring that it functions effectively as the body's blood pump.
Regulation of coronary circulation
Exercised by coordinating multiple physiologic and biochemical mechanisms to ensure adequate blood supply to the myocardium (heart muscle) under various conditions. The major regulatory mechanisms include:
- Autoregulation: Coronary arteries are able to automatically adjust their diameter in response to changes in blood pressure and myocardial needs. When the myocardium needs more blood supply, the arteries dilate to provide additional blood flow.
- Metabolic regulation: When the myocardium is more active, such as during exercise, levels of metabolic products such as adenosine and acylcaffeine increase in the myocardium. These products can dilate the coronary arteries, increasing blood flow where it is most needed.
- Sympathetic Nervous System: Stimulation of the sympathetic nervous system can cause constriction or dilation of the coronary arteries. Sympathetic activation, such as in response to stress or physical activity, can increase blood flow to the myocardium by dilating the coronary arteries.
- Platelet adhesion and coagulation: In the case of coronary artery injury, platelet adhesion and coagulation mechanisms may be activated to prevent bleeding and restore the integrity of the vascular wall.
- Endotheliumand Nitric Oxide: The endothelium (inner layer of the vascular wall) of the coronary arteries produces nitric oxide, which is a molecule that helps dilate blood vessels and reduce their contraction.
These mechanisms work closely together to maintain a normal blood supply to the myocardium under different conditions. Coronary blood flow is regulated to ensure adequate blood supply to the heart muscle and maintain its performance.
Coronary circulation disorder
Coronary artery disease, also known as coronary artery disease (CAD) or coronary heart disease (CHD), occurs when the supply of adequate oxygen and nutrients to the heart muscle (myocardium) is restricted or interrupted due to problems with the coronary arteries. This can cause a number of serious symptoms and complications. Below are some of the main aspects of coronary circulation disorders:
- Angina(stable and unstable): Angina is chest pain that usually occurs with exercise or stress and improves at rest or after taking nitroglycerin. Stable angina usually occurs with some activity and is predictable in nature, while unstable angina can occur at rest and is often indicative of a more serious problem with the coronary circulation.
- Myocardial infarction: A myocardial infarction (heart attack) occurs when one of the coronary arteries becomes completely blocked and the blood supply to part of the heart muscle is cut off. This is an extremely serious condition that requires immediate medical attention.
- Angina without pain (silent heart attack): Some people may have a myocardial infarction without significant chest pain. Instead, they may experience malaise, fatigue, back pain, neck pain, jaw pain, or stomach pain.
- Chronic CoronaryHeart Disease: This condition is characterized by chronic impaired coronary blood flow, which can lead to persistent symptoms such as fatigue, shortness of breath, and chest pain.
- Arrhythmias and heart rhythm disorders: Lack of oxygen to the heart can cause arrhythmias and heart rhythm disorders, which can be life-threatening.
- Heart failure: Prolonged impairment of coronary circulation may lead to deterioration of heart function and development of heart failure.
Treatment for coronary artery disease depends on the extent and severity of the problem. This may include drug therapy, angioplasty and coronary artery bypass procedures, and lifestyle changes including diet and physical activity. Regular medical follow-up and adherence to your doctor's recommendations play an important role in managing coronary artery disease.
Coronary circulation disorder on ECG
Can show up on an electrocardiogram (ECG) in a variety of ways, and the characteristic changes depend on which parts of the myocardium (heart muscle) have been subjected to ischemia (insufficient blood supply). Here are some of the typical ECG changes that may indicate impaired coronary blood flow:
- ST segment:
- ST-segment elevation: One of the most characteristic signs of coronary artery disease is an ST-segment elevation on the ECG. It can indicate an acute coronary event such as a myocardial infarction.
- ST-segment depression: Occasionally, changes in ST-segment depression may also be seen, which may also be an indicator of ischemia.
- Changes in T: The ECG may show changes in the shape and amplitude of the T claws, which may indicate impaired coronary blood flow.
- ST-segment depression: A fall in ST-segment level below the basal line may be a sign of ischemia, especially during exercise or stress.
- Asymptomatic changes: Some patients may have ECG changes that are not accompanied by symptoms. These changes may be detected during regular physical examination or monitoring.
- Changes in the leading rhythm: A coronary circulation disorder can also affect the leading rhythm of the heart, which can lead to arrhythmias or blockages.
It is important to realize that the presence of ECG changes alone is not always a definite diagnosis. Additional testing, including angiography (contrast x-ray of the coronary arteries) and other techniques, is often required to make an accurate diagnosis and determine the severity of coronary artery disease. If you have symptoms associated with coronary artery disease or if an ECG shows abnormalities, be sure to consult your physician for further evaluation and to determine the best treatment.
Acute coronary artery disease
This is a situation in which there is an acute and inadequate supply of oxygen and nutrients to the heart muscle (myocardium) due to obstruction in the coronary arteries. This condition is usually due to atherosclerosis (buildup of cholesterol and other substances in the arteries) or thrombosis (formation of a blood clot) in the coronary arteries. Acute coronary artery disease can take several forms:
- Unstable angina (unstable angina): This is a condition in which the blood supply to the myocardium is temporarily impaired, usually due to the formation of a blood clot or narrow narrowing in the coronary arteries. This can cause severe chest pain that usually does not go away at rest and may be accompanied by other symptoms such as shortness of breath and loss of consciousness.
- Myocardial infarction (heart attack): This is a more serious condition in which there is a complete or partial cessation of blood supply to the myocardium, resulting in the death of part of the heart muscle. Symptoms include severe chest pain, pain that may spread to the left arm, neck or back, shortness of breath, nausea and vomiting.
- Syndrome of acute coronary artery obstruction without myocardial infarction (unstable angina without infarction): This is a condition in which there is acute obstruction in a coronary artery but no necrosis of myocardial tissue has yet occurred. Symptoms may be similar to unstable angina, but more severe.
Any acute coronary bleeding disorder requires urgent medical attention. Treatment may include the use of medications to thin the blood and dilate the coronary arteries, angioplasty procedures (widening of narrowed arteries) or coronary artery bypass surgery. Prompt medical attention and timely treatment are critical to prevent serious complications and reduce the risk of myocardial infarction.
Treatment of coronary circulatory insufficiency
Treatment of coronary artery disease (coronary artery disease) may include a variety of drug and non-pharmacologic methods. The goal of treatment is to reduce symptoms, improve quality of life, and prevent complications. Here are some of the remedies and methods that can be used for coronary artery disease:
- Blood pressure medications:
- Beta-adrenoblockers: Reduce heart rate and decrease the workload of the heart.
- Calcium antagonists: May help dilate coronary arteries and reduce heart contractility.
- Angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor antagonists (ARBs): Improve blood flow and may help reduce the workload on the heart.
- Nitrates: Vasodilators, such as nitroglycerin, can help dilate the coronary arteries and improve blood flow to the myocardium. They are used to relieve angina attacks.
- Antithrombotic therapy: Drugs such as acetylsalicylic acid (aspirin) and anticoagulants can help prevent blood clots from forming in the coronary arteries.
- Lowering cholesterol: Statin drugs are used to lower "bad" cholesterol (LDL) and prevent atherosclerosis.
- Medications to manage diabetes mellitus: If the patient has diabetes mellitus, blood glucose levels should be strictly monitored.
- Lifestyle recommendations: Include a low salt and low fat diet, physical activity, smoking cessation and stress management.
- Rehabilitation after myocardial infarction: Rehabilitation programs can help patients regain physical activity, control risk factors, and strengthen the heart.
- Interventional procedures: This may include angioplasty (widening narrowed coronary arteries with a balloon) or coronary artery bypass grafting (grafting new blood vessels to bypass areas of narrowed arteries).
Treatment of coronary insufficiency should be individualized by a physician based on the clinical characteristics of each patient. It is important to follow the doctor's recommendations and undergo regular medical check-ups to monitor the condition of the heart and prevent complications.

