Medical expert of the article
New publications
Congenital hypothyroidism: causes, pathogenesis, consequences, prognosis
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
A disease caused by genetic factors and associated with thyroid insufficiency is congenital hypothyroidism. Let's consider the features of this pathology, treatment methods.
A complex of clinical and laboratory signs that occur from birth due to deficiency of thyroid hormones is congenital hypothyroidism. According to the International Classification of Diseases of the 10th revision ICD-10, the disease belongs to category IV Diseases of the endocrine system, nutritional disorders and metabolic disorders (E00-E90).
Thyroid diseases (E00-E07):
- E02 Subclinical hypothyroidism due to iodine deficiency.
- E03 Other forms of hypothyroidism:
- E03.0 Congenital hypothyroidism with diffuse goiter. Goiter (nontoxic), congenital: NEC, parenchymatous. Excludes: transient congenital goiter with normal function (P72.0).
- E03.1 Congenital hypothyroidism without goiter. Aplasia of thyroid gland (with myxedema). Congenital: atrophy of thyroid gland, hypothyroidism NEC.
- E03.2 Hypothyroidism due to drugs and other exogenous substances.
- E03.3 Postinfectious hypothyroidism.
- E03.4 Thyroid atrophy (acquired) Excludes: congenital thyroid atrophy (E03.1).
- E03.5 Myxedema coma.
- E03.8 Other specified hypothyroidisms.
- E03.9 Hypothyroidism, unspecified, Myxedema NEC.
The thyroid gland is one of the organs of the endocrine system, performing many functions responsible for the proper functioning and development of the entire body. It produces hormones that stimulate the pituitary gland and hypothalamus. The main functions of the gland include:
- Control of metabolic processes.
- Regulation of metabolism: fats, proteins, carbohydrates, calcium.
- Formation of intellectual abilities.
- Body temperature control.
- Retinol synthesis in the liver.
- Lowering cholesterol levels.
- Growth stimulation.
From birth, the organ affects the growth and development of the child's body, especially the bones and nervous system. The thyroid gland produces the hormone thyroxine T4 and triiodothyronine T3. Deficiency of these substances negatively affects the functioning of the entire body. Hormonal deficiency leads to slower mental and physical development, growth.
With congenital pathology, the newborn gains excess weight, has problems with heart rhythm and blood pressure. Against this background, energy decreases, intestinal problems and increased bone fragility appear.
Epidemiology
According to medical statistics, the prevalence of congenital hypothyroidism is 1 case per 5,000 infants. The disease is approximately 2.5 times more common in girls than in boys. As for the secondary form, it is most often diagnosed after 60 years. About 19 out of 1,000 women have a diagnosis. While among men, only 1 out of 1,000 is sick.
At the same time, the total number of the population with a deficiency of thyroid hormones is about 2%. The danger of the pathological disease is in its blurred symptoms, complicating the diagnostic process.
Causes congenital hypothyroidism
Genetic abnormalities are the main factor that provokes thyroid insufficiency. Possible causes of the disease also include:
- Hereditary predisposition – the disorder is closely associated with gene mutations, so it can develop in utero.
- Hormonal imbalances – occur due to decreased sensitivity of the thyroid gland to iodine. Against this background, the transport of useful substances necessary for hormone synthesis may be disrupted.
- Pathologies of the hypothalamus – the center of the nervous system regulates the functioning of the endocrine glands, including the thyroid gland.
- Decreased sensitivity to thyroid hormones.
- Autoimmune diseases.
- Tumor lesions of the thyroid gland.
- Reduced immunity.
- Drug overdose. Taking antithyroid drugs during pregnancy.
- Viral and parasitic diseases.
- Treatment with radioactive iodine preparations.
- Iodine deficiency in the body.
In addition to the above, there are many other causes of congenital pathology. In most cases, the cause of the disease remains unknown.
 [ 8 ]
[ 8 ]
Risk factors
In 80% of cases, dysfunction of the thyroid gland is caused by malformations of its development:
- Hypoplasia.
- Dystopia (displacement) into the retrosternal or sublingual space.
The main risk factors for congenital hypothyroidism include:
- Iodine deficiency in the female body during pregnancy.
- Exposure to ionizing radiation.
- Infectious and autoimmune diseases suffered during pregnancy.
- Negative impact of medications and chemicals on the fetus.
In 2% of cases, the pathology is caused by mutations in the genes: PAX8, FOXE1, TITF2, TITF1. In this case, the baby has congenital heart defects, cleft lip or hard palate.
About 5% of cases of the disease are associated with hereditary pathologies that cause disruptions in the secretion of thyroid hormones or their interaction with each other. Such pathologies include:
- Pendred's syndrome.
- Thyroid hormone defects.
- Organization of iodine.
In other cases, factors that can provoke hypothyroidism are:
- Birth injuries.
- Tumor processes in the body.
- Asphyxia of the newborn.
- Brain development disorders.
- Pituitary aplasia.
The action of the above factors leads to the development of resistance syndrome. That is, the thyroid gland can produce a sufficient amount of thyroid hormones, but the target organs completely lose sensitivity to them, causing symptoms characteristic of hypothyroidism.
Pathogenesis
The mechanism of development of thyroid gland abnormalities is caused by decreased biosynthesis and decreased production of iodine-containing hormones (thyroxine, triiodothyronine). The pathogenesis of congenital hypothyroidism due to problems with the production of thyroid hormones is associated with the action of various pathological factors at different stages:
- Iodine storage defect.
- Failure of the process of diiodination of iodinated thyronines.
- The transition of mono-iodothyronine and diiodothyronine to triiodothyronine and thyroxine and other hormones.
The development of the secondary form of the disease is associated with the following factors:
- Thyroid stimulating hormone deficiency.
- Decreased concentration of iodides in the thyroid gland.
- Secretory activity of the epithelium of the organ follicles, reduction of their number and size.
A polyetiological disease provokes a disruption of metabolic processes in the body:
- Lipid metabolism – slowing down the absorption of fat, inhibiting catabolism, increasing the level of cholesterol in the blood, triglycerides and β-lipoproteins.
- Carbohydrate metabolism – slowing down the processes of glucose absorption in the gastrointestinal tract and reducing its utilization.
- Water exchange – increased hydration capacity of mucin and disruption of colloid hydrophilicity leads to water retention in the body. Against this background, diuresis and the amount of chlorides excreted decrease. Potassium levels increase and the amount of sodium in the heart muscle decreases.
The above-mentioned metabolic pathologies lead to pathologies in the development of the brain and central nervous system.
 [ 9 ]
[ 9 ]
Symptoms congenital hypothyroidism
In most cases, symptoms of congenital thyroid dysfunction become apparent within a couple of months after birth. However, some babies show the first signs of the disease right away.
Symptoms of genetic pathology include:
- The newborn's weight is more than 4 kg.
- Long-term jaundice after birth.
- Blue discoloration of the nasolabial triangle.
- Facial swelling.
- Half-open mouth.
- Changing the timbre of the voice.
If the above symptoms remain without medical attention, they begin to progress. After 3-4 months, hypothyroidism manifests itself with the following symptoms:
- Disturbance of appetite and swallowing process.
- Peeling and paleness of the skin.
- Dry and brittle hair.
- Tendency to constipation and flatulence.
- Low body temperature, cold extremities.
There are also later, but obvious signs of the disease that develop a year after the birth of the child:
- Delay in physical and mental development.
- Late appearance of teeth.
- Low pressure.
- Change in facial expression.
- Enlarged heart.
- Rare pulse.
The above clinical manifestations complicate the diagnostic process, therefore early screening is indicated to detect the disease. The procedure is performed on all children within a week after birth.
 [ 10 ]
[ 10 ]
Complications and consequences
Reduced thyroid function is characterized by partial or complete hormone deficiency. The disease is dangerous due to serious developmental disorders in the newborn. The consequences and complications affect all organs of the baby's system, for the normal functioning of which the thyroid gland is responsible:
- Formation and growth of the skeleton and teeth.
- Cognitive abilities, memory and attention.
- Assimilation of vital microelements from breast milk.
- Functioning of the central nervous system.
- Lipid, water and calcium balance.
Congenital hypothyroidism leads to the following problems:
- Delayed development of the brain, spinal cord, inner ear and other structures.
- Irreversible damage to the nervous system.
- Delay in psychomotor and somatic development.
- Delay in weight and growth.
- Hearing loss and deafness due to tissue swelling.
- Loss of voice.
- Delay or complete cessation of sexual development.
- Enlargement of the thyroid gland and its malignant transformation.
- Formation of secondary adenoma and “empty” sella turcica.
- Loss of consciousness.
Congenital hormone deficiency in combination with developmental disorders leads to cretinism. This disease is one of the most severe forms of psychomotor developmental delay. Children with this complication lag behind their peers physically and intellectually. In rare cases, endocrine pathology leads to hypothyroid coma, which is a fatal risk in 80%.
Who to contact?
Prevention
Congenital hypothyroidism develops during pregnancy and in most cases for reasons beyond the woman's control (anomalies in the development of fetal organs, gene mutations). But despite this, there are preventive measures that can minimize the risk of having a sick child.
Prevention of hypothyroidism consists of comprehensive diagnostics both during pregnancy planning and during gestation.
- First of all, it is necessary to determine the level of thyroid hormones and the concentration of specific antibodies to thyroglobulin and thyroid peroxidase. Normally, antibodies are absent or circulate in an average amount of up to 18 U/ml for AT-TG and 5.6 U/ml for AT-TPO. Elevated values indicate the development of autoimmune inflammatory processes in the thyroid gland. Elevated antibodies to thyroglobulin increase the risk of oncological degeneration of organ tissues.
- If the disease was diagnosed before pregnancy, then treatment is carried out. Therapy begins with taking synthetic hormones and other drugs to restore normal hormone synthesis and restore thyroid function.
- If the pathology is detected after conception, the patient is prescribed maximum doses of thyroid hormones. Treatment lasts until the deficiency of thyroid hormones is replenished.
- Hypothyroidism can develop due to iodine deficiency. To normalize iodine balance and prevent deficiency of this substance in the body, the following remedies are recommended:
- Iodomarin
An iodine preparation with the active substance - potassium iodide 131 mg (pure iodine 100/200 mg). It is used to treat and prevent thyroid diseases. The microelement is essential for the normal functioning of the organ. Replenishes iodine deficiency in the body.
- Indications for use: prevention of thyroid diseases caused by iodine deficiency in the body. Prevention of iodine deficiency in people who need increased consumption of this substance: pregnant women, lactating women, children and adolescents. Prevention of goiter formation in the postoperative period or after drug therapy. Treatment of diffuse nontoxic goiter, diffuse euthyroid goiter.
- Method of application: the dosage depends on the patient's age and indications for use. On average, patients are prescribed from 50 to 500 mg per day. Preventive administration is long-term - 1-2 years in courses or continuously. In especially severe cases, iodine deficiency prevention is carried out throughout life.
- Side effects: develop with incorrectly selected dosage. Possible transition of latent hyperkeratosis to manifest form, iodine-induced hyperkeratosis, various allergic reactions. Overdose has similar symptoms.
- Contraindications: hyperthyroidism, intolerance to iodine preparations, toxic thyroid adenoma, Duhring's dermatitis herpetiformis. Use of the drug during pregnancy and lactation is not prohibited.
Iodomarin is available in tablet form in bottles of 50, 100 and 200 capsules.
- IodineActive
Replenishes the lack of iodine in the body. When there is a deficiency of this microelement, it is actively absorbed, and when there is an excess, it is excreted from the body and does not enter the gland. The drug is prescribed for the treatment and prevention of diseases associated with iodine deficiency in the body.
IodActive is contraindicated for patients with hypersensitivity to its components. The drug is taken 1-2 capsules once a day, regardless of food intake. The duration of treatment is determined by the attending physician.
- Iodine balance
An inorganic iodine compound that replenishes iodine deficiency in the body. Normalizes the synthesis of the main hormones of the thyroid gland. Reduces the formation of inactive forms of thyroid hormones. 1 capsule of the drug contains the active substance potassium iodide 130.8 mg or 261.6 mg, equal to 100 or 200 mg of iodine, respectively.
The active component restores and stimulates metabolic processes in the central nervous system, musculoskeletal, cardiovascular and reproductive systems. Promotes the normalization of intellectual and mnestic processes, maintains homeostasis.
- Indications for use: prevention of iodine deficiency states during gestation and lactation. Postoperative period after thyroid surgery. Prevention of goiter, complex treatment of euthyroid syndrome in newborns and adult patients.
- Method of administration: the daily dosage is determined by the attending physician, individually for each patient. Most often, patients are prescribed 50-200 mg per day. If the medicine is prescribed to newborns, then for ease of use, the tablets are dissolved in 5-10 ml of boiled warm water.
- Side effects: allergic reactions, tachycardia, arrhythmia, sleep and wakefulness disorders, increased excitability, emotional lability, increased sweating, gastrointestinal disorders.
- Contraindications: hyperthyroidism, Duhring's dermatitis, solitary thyroid cysts, nodular toxic goiter. Hyperthyroidism not of iodine deficiency etiology, thyroid cancer. Not prescribed for patients with congenital lactase and galactase deficiency.
Iodbalance is available in tablets for oral use.
- Another important preventive measure is a diet with sufficient iodine. During pregnancy, the level of thyroid hormones in the female body decreases sharply. Without additional supply of this microelement to the body, there is a risk of developing hypothyroidism.
Nutritional recommendations:
- Use iodized salt regularly.
- Products that contribute to the formation of goiter should be heat treated: broccoli, cauliflower and Brussels sprouts, millet, mustard, soybeans, turnips, spinach.
- Eat foods rich in vitamin B and E: nuts and olive oil, dairy products, eggs, meat, seafood.
- Include foods with beta-carotene in your diet: pumpkin, carrots, fresh potato juice.
- Replace coffee with green or black tea. The drink contains fluorides, which regulate thyroid function.
All the above recommendations are very important, and every woman planning to become a mother in the near future should know about them. The thyroid gland of the child is laid down at 10-12 weeks of intrauterine development, so the mother's body must contain a sufficient amount of nutrients and be ready to replenish them.
Forecast
The outcome of the congenital form of hypothyroidism depends on the timely diagnosis of the pathology and the time of the start of hormone replacement therapy. If treatment was started in the first months of life, then the intellectual abilities and psychophysical development of the child are not impaired. Treatment of children over 3-6 months allows to stop developmental delays, but existing intellectual disabilities will remain forever.
- If the pathology is caused by Hashimoto's disease, radiation therapy or absence of the thyroid gland, then the patient will have to undergo lifelong therapy.
- If hypothyroidism is caused by other diseases and disorders of the body, then after eliminating the causative factors, the patient's condition will normalize.
- In the case of a disease caused by medications, hormone synthesis is restored after discontinuation of medication.
- If the pathology is latent, i.e. subclinical, then treatment may not be required. But the patient needs to visit a doctor regularly to monitor the general condition and identify signs of disease progression.
If the disease was diagnosed late, the time for starting replacement therapy was missed or the medications were never started, the prognosis for congenital hypothyroidism worsens. There is a risk of developing severe complications of the disease: mental retardation, cretinism and disability.
 [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ]
[ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ]
Disability
According to medical statistics, disability in congenital hypothyroidism is 3-4%. Partial or complete loss of working capacity is observed in advanced stages of the disease and in severe forms of pathology that interfere with a full life.
A patient with thyroid dysfunction becomes hormone-dependent, which has a negative impact not only on health but also on lifestyle. In addition, certain stages of the disease are complicated by concomitant pathologies, which further aggravates the patient's condition.
To establish disability, the patient is referred to a medical social examination and a medical advisory commission. The main indications for undergoing a medical commission are:
- Hypothyroidism grade 2 or 3.
- Endocrine cardiomyopathy.
- Parathyroid insufficiency.
- Pronounced mental changes and disorders.
- Pericardial effusion.
- Decreased performance.
- The need to change working conditions.
To confirm disability, the patient must undergo a number of diagnostic procedures:
- Hormonal blood tests for TSH, TG.
- Electrolyte and triglyceride analysis.
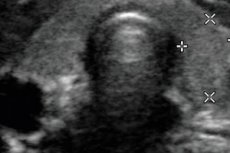
- Ultrasound and electromyography.
- Study of antibodies to thyroglobulin.
- Blood sugar and cholesterol levels.
Based on the results of the tests, the patient receives a disability certificate.
Disability has several categories, each of which has its own characteristics:
Degree |
Features of violations |
Restrictions |
Disability group |
Prohibited work |
I |
Mild somatic disorders. Increased fatigue and drowsiness. Minor decrease in psychomotor development. Growth retardation. Hormone levels are normal or slightly elevated. |
There are no restrictions on life activities |
Limitation on the VKK line |
|
II |
Moderate somatic disorders. Fatigue and drowsiness. Swelling. Blood pressure lability. Neurosis-like symptom complex. Neuropathy, growth retardation. Mild dementia. Hormone levels are moderately reduced. |
I degree of restrictions:
|
Group III |
|
III |
Severe somatic disorders. Bradycardia and myopathy. Sexual dysfunction. Long-term constipation. Hypothyroid polyserositis. Mental retardation. Severe hormonal disorders. |
II degree of restrictions:
|
II group |
Incapacity |
IV |
Severe somatic disorders. Severe pathologies of the cardiovascular system. Gastrointestinal disorders. Disorders of the urinary system. Neuropsychiatric pathologies. Growth retardation. Severe or moderate mental retardation. Significant hormonal disturbances. |
III degree of restrictions:
|
Group I |
Incapacity |
Congenital hypothyroidism is a serious pathology of the endocrine system, which without timely medical care threatens numerous complications and deterioration in the quality of life. In severe forms of the disease, disability is a necessary measure to alleviate the patient's condition and improve his quality of life.

