Medical expert of the article
New publications
Thyroid gland
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The thyroid gland (glandula thyroidea) is an unpaired organ located in the anterior region of the neck at the level of the larynx and upper trachea. The gland consists of two lobes - the right (lobus dexter) and left (lobus sinister), connected by a narrow isthmus. The thyroid gland lies quite superficially. In front of the gland, below the hyoid bone, are paired muscles: the sternothyroid, sternohyoid, omohyoid and only partly the sternocleidomastoid muscle, as well as the superficial and pretracheal plates of the cervical fascia.
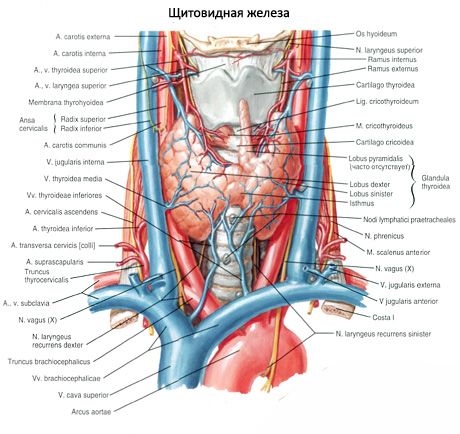
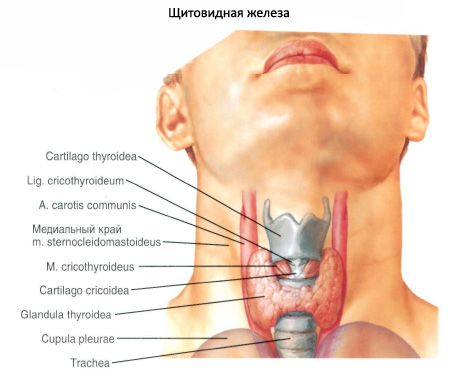
The posterior concave surface of the gland embraces the lower parts of the larynx and the upper part of the trachea from the front and sides. The isthmus of the thyroid gland (isthmus glandulae thyroidei), connecting the right and left lobes, is usually located at the level of the II or III tracheal cartilage. In rare cases, the isthmus of the gland lies at the level of the I tracheal cartilage or even the cricoid arch. Sometimes the isthmus may be absent, and then the lobes of the gland are not connected to each other at all.
The upper poles of the right and left lobes of the thyroid gland are located slightly below the upper edge of the corresponding plate of the thyroid cartilage of the larynx. The lower pole of the lobe reaches the level of the V-VI cartilage of the trachea. The posterolateral surface of each lobe of the thyroid gland is in contact with the laryngeal part of the pharynx, the beginning of the esophagus and the anterior semicircle of the common carotid artery. The parathyroid glands are adjacent to the posterior surface of the right and left lobes of the thyroid gland.
From the isthmus or from one of the lobes, the pyramidal lobe (lobus pyramidalis) extends upward and is located in front of the thyroid cartilage, which occurs in approximately 30% of cases. This lobe sometimes reaches the body of the hyoid bone with its apex.
The transverse size of the thyroid gland in an adult reaches 50-60 mm. The longitudinal size of each lobe is 50-80 mm. The vertical size of the isthmus ranges from 5 to 2.5 mm, and its thickness is 2-6 mm. The mass of the thyroid gland in adults from 20 to 60 years old is on average 16.3-18.5 g. After 50-55 years, there is some decrease in the volume and mass of the gland. The mass and volume of the thyroid gland in women is greater than in men.
The thyroid gland is covered externally with a connective tissue membrane - a fibrous capsule (capsula fibrosa), which is fused with the larynx and trachea. In this regard, when the larynx moves, the thyroid gland also moves. Connective tissue partitions - trabeculae - extend from the capsule into the gland, dividing the gland tissue into lobes, which consist of follicles. The walls of the follicles are lined from the inside with cubic-shaped epithelial follicular cells (thyrocytes), and inside the follicles there is a thick substance - colloid. The colloid contains thyroid hormones, consisting mainly of proteins and iodine-containing amino acids.
The walls of each follicle (there are about 30 million of them) are formed by one layer of thyrocytes located on the basal membrane. The size of the follicles is 50-500 µm. The shape of the thyrocytes depends on the activity of synthetic processes in them. The more active the functional state of the thyrocyte, the higher the cell. Thyrocytes have a large nucleus in the center, a significant number of ribosomes, a well-developed Golgi complex, lysosomes, mitochondria and secretory granules in the apical part. The apical surface of the thyrocytes contains microvilli immersed in a colloid located in the cavity of the follicle.
The glandular follicular epithelium of the thyroid gland has a selective ability to accumulate iodine more than other tissues. The concentration of iodine in thyroid tissues is 300 times higher than its content in blood plasma. Thyroid hormones (thyroxine, triiodothyronine), which are complex compounds of iodinated amino acids with protein, can accumulate in the colloid of follicles and, as needed, be released into the bloodstream and delivered to organs and tissues.
Thyroid hormones
Thyroid hormones regulate metabolism, increase heat exchange, enhance oxidation processes and the consumption of proteins, fats and carbohydrates, promote the release of water and potassium from the body, regulate growth and development processes, activate the activity of the adrenal glands, sex and mammary glands, and have a stimulating effect on the activity of the central nervous system.
Between the thyrocytes on the basement membrane, as well as between the follicles, there are parafollicular cells, the tops of which reach the lumen of the follicle. Parafollicular cells have a large round nucleus, a large number of myofilaments in the cytoplasm, mitochondria, the Golgi complex, and a granular endoplasmic reticulum. These cells contain many granules of high electron density with a diameter of about 0.15 μm. Parafollicular cells synthesize thyrocalcitonin, which is an antagonist of parathyroid hormone, a hormone of the parathyroid glands. Thyrocalcitonin is involved in the exchange of calcium and phosphorus, reduces the calcium content in the blood and delays the release of calcium from the bones.
Regulation of thyroid function is provided by the nervous system and the thyroid-stimulating hormone of the anterior pituitary gland.
Embryogenesis of the thyroid gland
The thyroid gland develops from the epithelium of the foregut as an unpaired median outgrowth at the level between the first and second visceral arches. Up to the fourth week of embryonic development, this outgrowth has a cavity, which is why it is called the thyroglossal duct (ductus thyroglossalis). By the end of the fourth week, this duct atrophies, and its beginning remains only in the form of a more or less deep blind opening on the border of the root and body of the tongue. The distal section of the duct divides into two rudiments of the future lobes of the gland. The forming lobes of the thyroid gland shift caudally and take their usual position. The preserved distal section of the thyroglossal duct turns into a pyramidal lobe of the organ. The reducing sections of the duct can serve as rudiments for the formation of accessory thyroid glands.
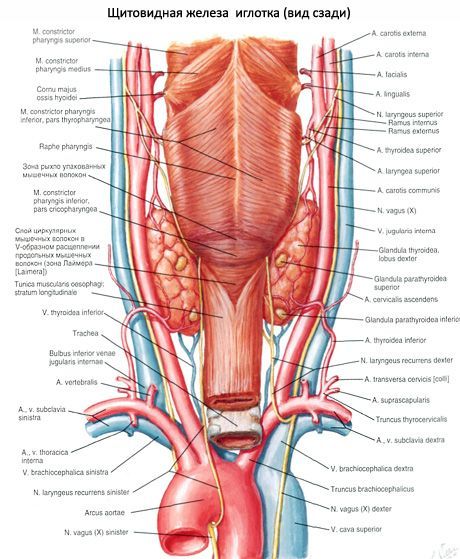
Vessels and nerves of the thyroid gland
The right and left superior thyroid arteries (branches of the external carotid arteries) approach the upper poles of the right and left lobes of the thyroid gland, respectively, and the right and left inferior thyroid arteries (from the thyrocervical trunks of the subclavian arteries) approach the lower poles of these lobes. The branches of the thyroid arteries form numerous anastomoses in the capsule of the gland and inside the organ. Sometimes the so-called inferior thyroid artery, which originates from the brachiocephalic trunk, approaches the lower pole of the thyroid gland. Venous blood from the thyroid gland flows through the superior and middle thyroid veins into the internal jugular vein, and through the inferior thyroid vein into the brachiocephalic vein (or into the lower part of the internal jugular vein).
The lymphatic vessels of the thyroid gland flow into the thyroid, prelaryngeal, pre- and paratracheal lymph nodes. The nerves of the thyroid gland depart from the cervical nodes of the right and left sympathetic trunks (mainly from the middle cervical node, follow the course of the vessels), as well as from the vagus nerves.
Age-related features of the thyroid gland
The thyroid gland in a newborn is much larger than in a fetus. During the first year of life, there is some decrease in the mass of the thyroid gland, which reaches 1.0-2.5 g. Before puberty, the size and mass of the thyroid gland gradually increase (up to 10-14 g). In the period from 20 to 60 years, the mass of the organ does not change significantly, remains almost constant and is equal to an average of 18 g. Some decrease in the mass and size of the organ due to age-related atrophy occurs in old age, but the function of the thyroid gland in old age often remains intact.
 [ 1 ]
[ 1 ]

