Medical expert of the article
New publications
Calculous chronic prostatitis
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
In clinical practice, when there are stones in the prostate gland during inflammation (in Latin calculus – stone), calculous prostatitis is diagnosed. Although this type of prostatitis is not distinguished in ICD-10, and prostate stones are classified as a separate subcategory.
Epidemiology
The prevalence statistics of calculous prostatitis are unknown, and stones in the prostate gland are accidentally detected by ultrasound in 7.4-40% of cases and in almost 70% of elderly men with benign prostatic hyperplasia. [ 1 ]
In chronic pelvic pain, the detection of stones is, according to some data, about 47%. [ 2 ]
Category IIIA prostatitis (chronic prostatitis/chronic pelvic pain syndrome with signs of inflammation) accounts for more than 90% of all cases of chronic inflammation of the prostate gland.
Causes calculous prostatitis
Prostatoliths, prostatic concretions or prostate stones are divided into endogenous and exogenous, depending on their etiology.
Prostate stones can be divided into primary or endogenous stones (occurring in the acini of the prostate gland) and secondary or external stones (caused by reflux of urine into the prostate). [ 3 ], [ 4 ]
Endogenous stones, often multiple and often asymptomatic, often occur with age (in the sixth decade) and are caused by obstruction of the ducts of an enlarged prostate or chronic inflammation. They are detected during endoscopic examinations in deeper structures of the prostate gland or its diverticula.
Exogenous stones occur primarily around the prostatic urethra (the part of the urethra enclosed by the prostate gland) and are thought to be a consequence of urethroprostatic (intraprostatic) reflux of urine and crystallization of salts contained in it. Their occurrence is not correlated with age and may be secondary to chronic urinary tract infection.
As a rule, the stones themselves do not cause symptoms, and the causes of calculous prostatitis are associated with the fact that most stones (78-83%) contain cells and entire colonies of bacteria - a source of infection of the prostate gland, causing not just chronic prostatitis, but chronic calculous prostatitis. [ 5 ]
According to clinical data, patients with prostate stones are more often diagnosed with category IIIA prostatitis (according to the NIH classification) - chronic pelvic pain syndrome with signs of inflammation, as well as category IIIB - chronic pelvic pain syndrome without signs of inflammation. More information in the material - Prostatitis: types.
Risk factors
The list, which includes the most probable risk factors for the development of chronic calculous prostatitis, reflects the various points of view existing in modern urology regarding the role of infection and its connection with prostatic stones as a result of the lithogenic process of calcification of the prostate gland.
So, the risk of calculous inflammation of the prostate is increased:
- in case of circulatory disorders in the pelvic area (this is a problem for those who have sedentary work and move little), which leads to ischemia and deterioration of the trophism of the glandular tissue;
- in case of stagnation of prostatic secretion in the parenchyma of the gland (due to the lack of regular sex);
- if there are chronic infections, primarily Chlamydia trachomatis, Trichomonas vaginalis, Mycoplasma, Ureaplasma urealyticum, gram-negative bacteria (Escherichia coli, Pseudomonas aeruginosa, Pseudomonas spp.) and gram-positive bacteria (Enterococcus faecalis, Staphylococcus aureus, Staphylococcus haemolyticus, Staphylococcus epidermidis); [ 6 ], [ 7 ]
- in mature and elderly men due to degenerative changes in the gland tissue (caused by a decrease in testosterone levels and an increase in dihydrotestosterone levels);
- with an increase in the size of the prostate (its benign hyperplasia);
- due to existing prostate adenoma; Stones are a pathophysiological phenomenon that occurs during the aging process, mainly after 50 years of age. Moore and Kirby et al., [ 8 ], as part of their proposed hypothesis regarding external stones, concluded that prostatic hypertrophy causes chronic inflammation of the prostate, which affects stone formation.
- against the background of diffuse changes in the prostate gland;
- in case of narrowing of the prostatic urethra;
- in case of dysfunction of the detrusor of the bladder or a spasmodic state of its neck, that is, when there are urination disorders of a neurogenic nature;
- for urolithiasis;
- due to disturbances in mineral metabolism, in particular calcium and phosphorus;
- if disturbances in general metabolism lead to acidosis with an increase in urine pH.
Pathogenesis
Although the formation of prostatic stones, as researchers suggest, may be a late stage of such a pathological process as calcification (calcinosis) of the prostate gland, the exact mechanism of development of calculous prostatitis - its pathogenesis - is still unclear. This is the result of not only different approaches to the causes of inflammation (in particular, as a complication of chronic prostatitis), but also the obvious combined influence of many factors present in specific patients.
According to some foreign studies, [ 9 ], [ 10 ] more than 83% of prostatic stones consist of calcium phosphate in the form of hydroxyapatite; almost 9% - of calcium carbonate and only about 4.5% - of calcium oxalate. There are also stones of mixed composition.
Also, the identification of the connection between the presence of stones in the prostate and its inflammation was facilitated by the clarification of the main protein components of prostatic stones. Thus, amyloid bodies (corpora amylacea) of the prostate secretion were found in them; lactoferrin (a protein of cellular immunity that stimulates phagocytosis); calprotectin produced by leukocytes; myeloperoxidase (antimicrobial factor of neutrophils), α-defensin (immune peptide of neutrophils); calcium-binding proteins (S100 A8 and A9), as well as keratin and the remains of exfoliated epithelial cells.
Thus, prostatic stones play an important role in the pathogenesis of prostatic inflammation, and their formation appears to be the result of inflammation-induced calcification.
In this case, chronic congestive calculous prostatitis, i.e. congestive, is classified as non-bacterial prostatitis. And stagnation of prostate secretion can be associated with its difficult removal from the gland acini when endogenous stones form in them, blocking the excretory ducts.
Symptoms calculous prostatitis
The first clinical report of urinary symptoms associated with prostate stones was published in the late 19th century. [ 11 ] Today, it is generally accepted that prostate stones occur proportionally with age, without causing any specific symptoms. [ 12 ]
In some cases, calculous prostatitis does not manifest itself in any way, and the first signs of the disease, especially in the initial stage, can be felt in the form of discomfort in the scrotum and perineum with periods of minor pain.
In general, the symptoms of calculous prostatitis are similar to the clinical manifestations of ordinary chronic prostatitis, [ 13 ] and are:
- burning during or after urination;
- difficulty at the very beginning of urination;
- dysuria (pain and increased frequency of urination);
- incomplete emptying of the bladder after urination, accompanied by urine leakage;
- aching pain above the penis, in the scrotum or under it, in the pelvic area (including rectal) and lower back;
- pain during or after sexual intercourse.
The intensity of symptoms is individual. More information in the materials:
Complications and consequences
Prostate stones and inflammation can have consequences and complications such as;
- urethral obstruction;
- enuresis;
- decreased libido or impotence;
- sclerotic changes in the prostate parenchyma;
- development of inflammation of the seminal vesicles (vesiculitis);
- recurrent bacteriuria.
Diagnostics calculous prostatitis
Prostate stones are detected by transrectal ultrasound (TRUS). Recently, as the adoption of TRUS has increased, more studies have been conducted on prostate stones, and some reports have been made on the shape and composition of the stones. However, the incidence of stones, the mechanism of their formation, their relationship with benign or malignant prostate lesions, and the clinical significance of stones are not yet known.
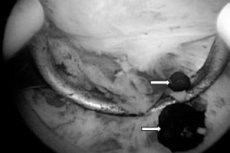
Experts note such echographic signs of chronic calculous prostatitis as discrete, multiple small echoes, usually diffusely distributed throughout the gland, while the white spots of the stones are hyperechoic, and the inflammation zone appears as a hypoechoic area.
Instrumental diagnostics can also be carried out using pulsed wave Dopplerography, urethroscopy, urethrocystography, and magnetic resonance imaging of the prostate.
The following tests are prescribed: a general blood test, urine tests (clinical, biochemical and bacterial culture), prostate secretion analysis, and a urethral smear.
Differential diagnosis
Differential diagnosis should exclude the presence of interstitial cystitis, neurogenic bladder dysfunction, tuberculosis or bladder carcinoma.
Who to contact?
Treatment calculous prostatitis
Prostate stones, which are usually asymptomatic, usually do not require specific treatment. However, the most problematic cases of prostate stones are associated with chronic inflammation of the prostate. In this case, antibiotic treatment in combination with prostatitis treatment may result in resolution of symptoms. However, since prostate stones infected with bacteria are a source of constant inflammation, meticulous removal of prostate stones is the preferred treatment for chronic bacterial inflammation of the prostate. Lee and Kim analyzed the efficacy of oral antibiotics in 64 patients with chronic bacterial prostatitis and reported that the cure rate with pharmacotherapy was 63.6% in patients without stones and 35.7% in patients with stones.
Drug treatment includes a course of antibacterial drugs from the fluoroquinolone group (Ciprofloxacin, Cephalexin, Ofloxacin, Levofloxacin), the tetracycline antibiotic Doxycycline, etc. According to some studies, the cure rate after using fluoroquinolones ranges from 63% to 86%. [ 14 ], [ 15 ] See - Chronic prostatitis: antibiotic treatment.
Anticholinergic drugs Tolterodine (Detrol, Detruzin, Urotol) help reduce the frequency of urination - 1-2 mg twice a day. The drug can cause headaches and dizziness, increased heart rate, dry mucous membranes, urinary retention, peripheral edema.
In chronic calculous prostatitis against the background of benign prostatic hypertrophy, a drug from the 5-α-reductase inhibitor group is used: Finasteride (Prosteride, Proscar) - 5 mg per day (one tablet); Dusteride (Avodart) - 0.5 mg per day (one capsule); duration of administration is six months. Side effects include erectile dysfunction and decreased fertility.
Pain is relieved by such medications as No-shpa or Ibuprofen (and other NSAIDs). Suppositories for prostatitis are used locally. And vitamins A, C and E are prescribed to reduce oxidative stress of prostate cells.
Read more:
Physiotherapy treatment – detailed in the publications:
Acupuncture significantly reduces overall pain, urinary symptoms and quality of life in men with chronic prostatitis and chronic pelvic pain syndrome.[ 16 ]
For this disease, homeopathy offers such remedies as Sabal serrulata, Pulsatilla, Kali bichromium, Baryta carbonica, Conium Maculatum, Chimaphilla umbellate, Causticum, Lycopodium clavatum.
In the absence of positive results from conservative therapy, when patients continue to experience difficulty urinating or chronic pain, surgical treatment is performed:
- removal of prostatoliths – transurethral ultrasound, electromagnetic or laser lithotripsy;
- removal of part of the prostate (transurethral resection);
- transurethral electrovaporization (evaporation) of the prostate;
- laser enucleation prostatectomy;
- removal of the entire gland (open prostatectomy).
Prostate stones are asymptomatic in most cases, but in some cases, a large prostate stone protruding into the urethra causes severe lower urinary tract symptoms such as urinary obstruction. In such cases, prostate stones can be removed using a transurethral endoscope.
Folk treatment involves taking warm baths with decoctions of medicinal plants (chamomile flowers, sage herb, peppermint, sage, thyme and cinnamon) also have antimicrobial activity) [ 17 ] and taking pumpkin seed oil internally (pumpkin seed oil can inhibit testosterone-induced prostatic hyperplasia and therefore may be useful in the treatment of benign prostatic hyperplasia). [ 18 ] Transperineal phonophoresis has been shown to be effective in the treatment of chronic non-bacterial prostatitis using pumpkin seed oil as a binding medium. [ 19 ]
Saw palmetto (Serenoa repens) is widely used in many Asian, African and European countries. In compositional analysis, sterols and free fatty acids were detected in the berries of S. repens. Initial studies suggested that the efficacy of S. repens may be similar to that of pharmaceutical inhibitors such as finasteride. These preliminary findings prompted investigations into the mechanism, utility and efficacy of this herb in in vitro assays and clinical trials. Several studies have investigated the use of S. repens for the treatment of symptoms associated with BPH [ 20 ], [ 21 ] and chronic prostatitis. [ 22 ]
A pollen extract called Cernilton is purported to be useful for a variety of urological conditions. Anecdotal evidence and references from texts indicate potential anti-inflammatory properties and potential for Cernilton in treating symptomatic pain relief and urinary dysfunction, which are often present in both chronic prostatitis and BPH. [ 23 ] And in vitro studies show various experiments with this particular extract, including histopathological analysis of its effects on cell proliferation, apoptosis, serum cytokines, and testosterone. [ 24 ], [ 25 ] Quite a few clinical trials of pollen extract are also listed in the literature; however, five are in Japanese and one is in German. [ 26 ] While many of these studies report the efficacy of pollen extract and suggest its usefulness for chronic prostatitis and chronic pelvic pain syndrome, the data from these studies have not been summarized due to unavailability and translation of the articles.
One study found quercetin to be effective in treating symptoms of chronic prostatitis (P=0.003) compared to placebo. Although this is the only clinical trial to examine the effects of quercetin on relieving symptoms of prostatitis, the positive result supports the need for further research, including cost analysis of quercetin therapy in this patient population.[ 27 ]
One study found that the multi-herbal formula WSY-1075 (25% C. fructus, 25% A. gigantis radix, 25% L. fructus, 10% C. parvum cornu, 10% G. radix rubra, and 5% C. cortke) had antimicrobial, anti-inflammatory, and antioxidant effects in the treatment of chronic bacterial prostatitis.[ 28 ]
Prevention
There are currently no methods developed to prevent chronic calculous prostatitis. However, it is recommended to lead a healthier lifestyle and not neglect physical exercise – to avoid congestion in the prostate gland.
Forecast
Calculous prostatitis has a very favorable prognosis, although getting rid of chronic pelvic pain is a serious medical problem.

