Medical expert of the article
New publications
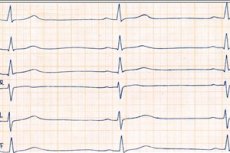
Types of bradycardia
Last reviewed: 08.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
There may be no subjective sensations of slowing of the heart rate, and if they are present, then regardless of its type, they manifest themselves in the same way. The allocation of different types of bradycardia is important not so much for patients as for the doctor in the context of determining the treatment tactics.
This deviation of the heart rate from the reference value is classified according to different criteria. Thus, according to the reasons causing bradycardia, the following are distinguished:
- physiological, which is a variant of the norm;
- pharmacological or medicinal, arising as a side effect from taking medications, often incorrectly;
- pathological, manifested as a result of heart disease (intracardiac) and damage to other organs (extracardiac), which can indirectly provoke a slow heartbeat (sometimes drug-induced is not singled out as a separate type). [ 1 ]
Pathological bradyarrhythmias are also classified by more specific causes of occurrence. They are toxic, endocrine, neurogenic, medicinal, myogenic (based on organic lesions of the heart muscle).
Bradycardia is interpreted as absolute, that is, determined constantly, in any body position and patient condition, the presence or absence of previous physical and mental stress, as well as relative, caused by certain circumstances - injuries, diseases, medications, stress, physical exertion.
In some patients, the causes of slow heartbeat remain unclear even with all the research available at the present level. Such patients are diagnosed with idiopathic bradycardia. It can also be observed constantly or periodically. If, in addition to the slowing of the pulse, nothing else bothers the person, then treatment in this case is not required. [ 2 ]
According to the localization of the source of disturbances, sinus bradycardia is distinguished, associated with a decrease in the activity of the pacemaker cells of the sinus node, which do not produce the required number of impulses per minute while maintaining their rhythm and coordination. Such work of the myocardium is quite often an individual feature, a normal variant that does not cause hemodynamic disturbances, and does not require therapeutic measures. [ 3 ]
The sinus (sinoatrial) node may work as it should. In this case, the cause of the slow pulse is a blockade of the nerve fibers that transmit electrical impulses. Transmission can be disrupted in various areas from the atria to the ventricles (atrioventricular blocks) and in the area between the sinoatrial node and the right atrium (sinoauricular block). The transmission of electrical impulses can be partially blocked when they are conducted, but more slowly or not all, and also completely, which is a lethal threat.
Bradycardia (bradyarrhythmia) can be compensated, which means the body's ability to cover this deviation without pathological consequences. It is an accidental finding. Drug therapy is not required in such cases, you just need to know about this feature of your body and periodically monitor your condition. [ 4 ]
A decompensated condition requires medical attention because the symptoms of a slow heart rate, insufficient blood volumes entering the systemic circulation, and associated hypoxia bother the patient, and self-compensation is no longer possible.
Physiological bradycardia
This type of slow heartbeat is considered a normal variant caused by the influence of certain physiological conditions. Such physiological features are inherent in trained people accustomed to regular and significant physical activity. Functional bradycardia is observed in this category of the population at rest and is expressed in a slowdown in heart rate, sometimes very significant. A trained heart, accustomed to working under overload conditions, ensures normal hemodynamics, for example, during night sleep with rare shocks, since it contracts powerfully and strongly, pushing out a large volume of blood with one shock.
This type of heart function may be constitutional and genetic in nature and may be observed in members of the same family. These people are usually naturally well-developed physically and, as a result, lead an active lifestyle.
Bradycardia of athletes and a genetically determined feature of the body reflects the powerful work of a well-trained heart during rest and is expressed in relative hypotension of the sympathetic part of the autonomic nervous system against the background of dominance of the vagus nerve activity. Such autonomic imbalance is characterized by stability. However, detection of a slow pulse in people with such features requires examination to exclude intracardiac lesions.
Slow heart rate can be caused by age-related changes and hormonal imbalances: rapid physical growth during adolescence, pregnancy, and aging of the body.
Reflex bradycardia is also physiological. It occurs as a reaction to a decrease in body temperature or stimulation of the vagus nerve - artificially induced by pressing on the carotid artery or on the eyes, during chest massage in the area located above the heart.
Drug-induced bradycardia
A decrease in the activity of the sinoatrial node may occur as a result of a course of treatment with certain medications. Most often, this type of cardiotoxic effect is caused by: β-blockers, calcium antagonists, cardiac glycosides, opiates. The development of an undesirable effect usually occurs with incorrect dosing, self-medication, failure to comply with the recommended duration of the course of treatment. If the drug causes slow heart function, it is necessary to discuss with the doctor a dose adjustment or replacement (cancellation) of the drug.
In addition to medications, a cardiotoxic effect in the form of bradycardia can develop in heavy smokers, alcoholics, and with various infections and poisonings. [ 5 ]
Vertical bradycardia
A slow pulse can be determined in one body position, and in another - correspond to the norm. Usually, when a patient is diagnosed with irregular heartbeat, the pulse is counted in different positions - standing, lying down, when changing positions.
Vertical bradycardia is diagnosed when the patient's pulse slows down while standing or walking. If the patient lies down, his heart rate returns to normal. This feature is referred to as sinus bradyarrhythmia. It is more common in children. Severe bradycardia manifests itself with characteristic symptoms, mild and moderate bradycardia can proceed with unnoticeable symptoms and be a normal variant.
The vertical position of the electrical axis of the heart on the cardiogram, like any other, can be combined with any heart rhythm.
Horizontal bradycardia
Slowing of the heart rate in the lying position occurs quite often and, in most cases, is an individual feature of a given organism. A person has bradycardia when lying down, while in a standing position, on the move or under load, the pulse rate increases. If such changes are not accompanied by pathological symptoms of cerebral hypoxia, then there should be no cause for concern.
Slowing of the pulse during sleep is quite acceptable. Nocturnal bradycardia is typical for trained people, when the heart compensates for the lack of physical activity by slowing the pulse. Rare powerful impulses are quite enough to ensure normal blood flow. This condition is also called rest bradycardia. It can be observed not only when the patient is sleeping, but also when he is simply resting in a relaxed state.
Neurogenic bradycardia
This form of slow heart muscle function accompanies extracardiac diseases that cause hypertonicity of the vagus nerve. [ 6 ]
Direct irritation of the vagus nerve is caused by neuroses, tumors of the mediastinum or brain, meningitis, cholelithiasis, inflammatory diseases of the stomach and intestines, inflammation of the middle ear, acute widespread glomerulonephritis, hepatitis and hepatosis, severe infectious diseases. These extracardiac pathologies can be accompanied by rare contractions of the heart muscle. Vagal bradycardia is often found in children and adolescents and is one of the manifestations of vegetative-vascular dystonia. It is accompanied by sleep disorders, severe fatigue, capriciousness, poor appetite.
Hypertonicity of the vagus nerve, caused by any reasons, provokes the development of weakness of the sinoatrial node and sinus bradyarrhythmia at any age. Clinically, this condition is manifested by non-specific symptoms - low blood pressure, general weakness, dizziness, sweating, shortness of breath, temporary disturbances of consciousness, in more severe cases, hypoglycemia and Morgagni-Adams-Stokes syndrome may develop.
Neurogenic bradycardia can develop in acute myocardial infarction, affecting the cardiomyocytes located along the inferior wall of the heart muscle.
The dominance of the vagus nerve tone is also manifested by physiological bradycardia, however, if it has a pathological origin, then without treatment the condition will progress. Therefore, when a slow pulse is detected even in trained people, it is recommended to undergo an examination to exclude organic intra- and extracardiac pathologies.
Systolic bradycardia
Any disturbance of the contractile activity of the heart affects such an indicator of its work as the amount of arterial blood ejected by the heart muscle in one contraction (systolic volume). Therefore, the expression systolic bradycardia is not correct. It may mean that with a moderate degree of decrease in the number of heart contractions, the body can turn on a compensatory mechanism in the form of an increase in systolic volume. At the same time, organs and tissues do not experience hypoxia, since the amount of arterial blood ejected by powerful but rare strokes is enough to ensure normal hemodynamics in a particular person.
However, this compensatory mechanism is not activated in everyone. In many, the systolic volume does not change, and with a decrease in heart rate, hypoxia and symptoms of insufficient blood supply gradually develop.
Also, with prolonged tachyarrhythmia, the duration of the diastolic period of the heart's work is shortened, causing a decrease in the volume of blood filling the ventricles. Over time, this reduces the systolic volume and the value of the minute volume of blood circulation, which provokes the development of signs of bradycardia.
Respiratory bradycardia
Moderate slowing of the pulse during exhalation is typical for childhood and puberty, people with hypertonicity of the autonomic nervous system. At the same time, during inhalation, the pulse rate in patients with respiratory arrhythmia increases.
The pathogenesis of such an anomaly of the respiratory rhythm is not associated with organic intracardiac disorders. Respiratory arrhythmia does not lead to the development of blood flow disorders and does not cause the development of constant dyspnea, cardiogenic shock and edema. The heart rhythm remains sinus, normal, only an increase in the length of the RR interval corresponding to exhalation is observed on the electrocardiogram. Respiratory bradycardia is not classified as a true arrhythmia. It can be called sinus in the diagnosis, since the heart maintains a normal sinus rhythm (impulses are emitted by the sinoatrial node).
Respiratory bradycardia may be observed constantly in some people, and periodically in others. It is manifested by a slowing of the pulse on exhalation, sometimes completely stopping, and an acceleration on inhalation, especially if it is deep.
It proceeds asymptomatically, the presence of undesirable symptoms of hypoxia will most likely indicate the presence of some cardiac or extracardiac pathology. Often accompanies neurocirculatory dystonia. Usually noticeable manifestations of accelerated pulse on inspiration, as well as hyperhidrosis, cold hands and feet, some discomfort behind the sternum, a feeling of lack of air.
In children and adolescents, respiratory bradycardia is often associated with intensive growth, in expectant mothers - with changes in hormonal levels, increased stress on the body. In these categories of the population, the symptoms of respiratory bradycardia disappear on their own after some time.
The alarm should be raised in cases where an accidentally detected slowing of the pulse associated with the respiratory cycle is accompanied by serious discomfort - severe weakness, symptoms of hypoxia, pre-fainting and fainting conditions. [ 7 ]
Arrhythmia and bradycardia (bradyarrhythmia)
The human heart works automatically, never stopping, throughout life. A rare slow pulse (bradycardia), as well as a frequent one - the heart pounds, jumping out of the chest (tachycardia), unscheduled impulses (extrasystoles) or freezing halfway (blockades) are types of anomalies of the rhythmic work of the heart muscle (arrhythmia).
Sometimes the heart rhythm is disturbed in everyone - during emotional outbursts, physical stress. Many have deviations from standard indicators, but do not feel them. Rhythm failures occur for various reasons and, accordingly, have different consequences. Physiological changes are not dangerous, and the most noticeable and common disorder is accelerated heartbeat or tachycardia. Slow rhythm and other disorders are not so noticeable, especially in the embryonic state. If an electrocardiogram or home tonometer shows the presence of any kind of arrhythmia, it is worth consulting a cardiologist and following his advice on further actions.
The term bradyarrhythmia is a complete synonym for bradycardia, therefore everything that has already been and will be said about a slow heart rate concerns this formulation of the diagnosis.
Extrasystole and bradycardia
Extrasystoles are extraordinary impulses that occur outside the cardiac rhythm in ectopic foci of hyperactivity located in any section of the conduction system outside the sinoatrial node (atria, ventricles, atrioventricular node). These impulses are transmitted through the myocardium, causing its contractions at the moment of relaxation of the atria and ventricles, when they are filled with blood. An extraordinary extrasystolic ejection of blood has a volume below the norm, in addition, the next ejection also has a lower volume. Frequent extrasystoles can lead to a significant decrease in hemodynamic parameters.
In bradycardia, when the activity of the sinus node decreases or the conduction of impulses is disrupted, passive ectopic non-sinus rhythms arise, which have a substitutive nature, exciting cardiac contractions. Their protective function in the absence of impulses of the main pacemaker is beyond doubt. New impulse centers begin to function independently, getting out of the control of the sinus node. The reasons for this are all the same factors that lead to the development of bradycardia. [ 8 ]
Subjectively, extrasystole is perceived as a push of the heart into the inner wall of the chest. Such sensations arise due to active contraction of the ventricular muscles after their relaxation. Patients may complain of a feeling that the heart is tumbling or turning over, and hear its uneven work. Some patients do not notice extrasystole at all, but may note a feeling of fear, fear of death, sweating attacks, weakness, discomfort in the chest, and inability to inhale. People with neurocirculatory dystonia have a hard time with extrasystole. [ 9 ]
Atrial extrasystole is functional in most cases and is practically not detected in serious heart lesions. Whereas the activation of cardiomyocytes – pacemakers of the atrioventricular node and, especially, the ventricles of the heart (idioventricular rhythms) is characteristic of serious heart pathologies and is manifested by symptoms of bradycardia corresponding to the severity of the underlying disease. In patients with long-term recorded atrioventricular rhythm, resistant heart failure, frequent attacks of angina pectoris, and fainting at the height of the Morgagni-Adams-Stokes syndrome develop. [ 10 ]
Ventricular extrasystole and bradycardia
In more than 2/3 of episodes, ectopic foci of hyperactivity are formed in the muscular layer of the ventricles. Idioventricular rhythm impulses arise. The most dangerous is ventricular extrasystole, which developed against the background of heart disease.
With pronounced bradycardia, significant circulatory disorders are observed, requiring resuscitation measures. Life-threatening conditions develop:
- ventricular paroxysmal tachycardia – attacks of increased contraction rate of these parts of the heart muscle (up to 200 beats/min), the consequence of which is acute ventricular failure, arrhythmogenic shock;
- ventricular fibrillation or a similar condition, flutter, in which myocardial contractions are ineffective and blood practically does not enter the systemic circulation;
- ventricular asystole – cessation of cardiac activity, coma.
Idioventricular rhythm, the source of which is located in the ventricular myocardium, in combination with atrial asystole, in most cases indicates a pre-mortem condition.
Atrial fibrillation and bradycardia are a dangerous combination, especially in cases where the pulse is rare and not rhythmic. In such cases, patients are recommended to implant a pacemaker.
With atrial fibrillation, the heart "churns" the blood, increasing its viscosity. At this point, blood clots - emboli - form in the left atrium, which can travel through the bloodstream to the brain and cause thrombosis of the cerebral arteries, their blockage or rupture, and to the lungs - and block the pulmonary artery. Patients with atrial fibrillation are prescribed blood-thinning drugs, such as cardio-aspirin or cardio-magnyl. [ 11 ]
Bradycardia and asystole
Cardiac arrest, complete absence of its electrical activity, and, as a result, cessation of blood flow in the body's vessels is asystole. It can be temporary - after a very short stop, blood circulation resumes. Asystole lasting up to three seconds is felt as dizziness, up to nine - loss of consciousness occurs. If blood circulation stops for a quarter of a minute - you can die. An ambulance usually does not have time to arrive.
The causes of primary asystole are ischemic heart disease and cardiac conduction disorders. A slow pulse precedes cardiac arrest.
Secondary develops in different conditions. Cardiographic rhythms that indicate approaching cardiac arrest are ventricular fibrillation or absence of pulse in ventricular tachycardia; absence of pulse with preserved electrical conductivity. [ 12 ]
Angina and bradycardia
A long-term and quite pronounced slow heartbeat is complicated by insufficient oxygenation of organs and tissues, including the heart muscle, which must work day and night without stopping. The heart suffers from hypoxia, cardiomyocytes die and ischemic foci are formed. Bradycardia contributes to the development of such a form of ischemic heart disease as angina pectoris or angina pectoris, as it was called earlier because attacks are felt as sudden pain, pressure on the chest, as if something heavy has fallen on it, preventing breathing (large toad). Rare heart contractions lead to a decrease in the volume of blood pumped by the heart.
Symptoms of angina pectoris combined with bradycardia indicate the body's inability to regulate the blood circulation process independently. In the absence of medical care, the body's condition worsens, ischemic areas increase, the heart loses its ability to work, and the entire body suffers. If at first the symptoms of angina pectoris appear during the patient's actions associated with a certain amount of stress, later the attacks begin to bother during rest as well. [ 13 ]
The clinical picture of angina is sudden attacks of severe pain, accompanied by a feeling of heaviness in the chest, inability to take a deep breath, distension of the chest, pain can radiate to the left arm, under the shoulder blade, to the jaw, there is a feeling of severe weakness, shortness of breath - the legs simply do not hold up, the skin turns pale, the heart works intermittently. There may be nausea, and in a severe attack - vomiting.
In the initial stages, the symptoms are not clearly expressed and may not all be present. The main symptom is a sudden attack of severe pressing or bursting pain. [ 14 ] Seeing a doctor at the first signs of developing pathology will help get rid of it in the shortest possible time; in severe stages, implantation of a pacemaker may be necessary.
Bradycardia and heart blocks
The non-sinus type of slow heartbeat is associated with the occurrence of obstacles to the passage of impulses, blockade of electrical impulses in different areas of the nerve fibers of the cardiac conduction system.
The causes of cardiac conduction disorders are different – organic heart lesions, intoxication with toxic substances and medications. Blockades sometimes occur in completely healthy people. [ 15 ]
The impulse transmission can be interrupted at any section of conduction. The main generator (pacemaker) is the sinus (sinoatrial, sinoatrial) node, which generates electrical impulses with the highest frequency. The atrioventricular or atrioventricular node that follows it can replace the sinoatrial node if necessary and generate impulses, but with a lower frequency of ten to twenty beats. If the nodes fail, the nerve fibers of the His bundle and/or the Purkinje fibers are activated, but they generate rare impulses corresponding to pronounced bradycardia.
However, even if the sinus node generates impulses with the required frequency, they will not reach their destination due to obstacles on the way (blockades). Transmission is blocked at different levels: between the sinoatrial node and the atria, from one atrium to another. Below the atrioventricular node, the conduction defect may be in different areas, and conduction may also be impaired at the level of any leg of the His bundle.
Complete atrioventricular block (grade III) is the most dangerous. These sections of the heart begin to work independently of each other, becoming excited and relaxed at a frequency determined by the ectopic foci that have arisen in them. Complete disorganization of the electrical activity of the myocardium occurs. [ 16 ]
Milder degrees of blockade: the first, when the impulses still reach the end point, but with a slight delay, and the second, when not all impulses reach the end point.
Milder forms are characterized by asymptomatism, pronounced blockade bradycardia is characterized by symptoms of insufficient blood supply, primarily to the brain, and attacks of hypertension, angina pectoris, and heart failure that cannot be controlled with medication may be added.
Bradycardia and left ventricular hypertrophy
Oxygen-rich blood is ejected into the aorta from the left ventricle. This section of the heart provides oxygenation of the organs and tissues of the entire body. Hypertrophy (increase in size, thickening of the walls) often develops in completely healthy individuals who regularly train the heart muscle and thereby cause an increase in the weight and volume of the intensively working organ, the so-called athlete's heart. Due to this, the volume of arterial blood ejected into the bloodstream increases and the pulse slows down, since there is no need for frequent ejections. This is a natural process that does not cause hemodynamic disturbances. [ 17 ]
Left ventricular hypertrophy may develop to compensate for pathological processes that impede blood ejection into the aorta and to overcome vascular resistance. Aortic anomalies, valve defects, hypertrophic cardiomyopathy, arterial hypertension, atherosclerosis, and other organic myocardial lesions may be accompanied by hypertrophic changes in the left ventricle.
These diseases often develop asymptomatically for a long time, manifesting themselves only by a slowing of the pulse. Bradycardia itself does not lead to hypertrophic changes, but is rather a symptom of them.
Therefore, a low pulse, especially a constant one, is a serious reason for a thorough examination. Such a non-invasive diagnostic procedure as an ultrasound of the heart can see changes in the structure of the myocardium at early stages. [ 18 ]
Pacemaker migration and bradycardia
In case of disorders of the sinoatrial node automatism or blockades of electrical impulses, other centers of automatism, localized outside the main source of impulses, begin substitution activity to excite the myocardium. Bradycardia contributes to the emergence of passive ectopic rhythms and complexes, one of which is the migrating or sliding rhythm (migration of the pacemaker). This phenomenon consists of a gradual movement of the impulse source from the sinoatrial node to the atrioventricular node, and then in the opposite direction. Each cycle begins in a new place: from the sinoatrial node, different structural elements of the atria, from the atrioventricular node. The most common shift of the pacemaker is: sinus → atrioventricular and back. The impulse generator shifts gradually, which on the cardiogram looks like various modifications of the P wave figure, reflecting the contraction of the atria. [ 19 ]
Migrating rhythm can be observed in healthy individuals with dominant vagal tone.
Heart diseases can also cause the formation of a migratory rhythm: sick sinus syndrome, inflammation of the heart muscle, ischemic disease, rheumatic defects. Cardiological complications after infectious diseases can also provoke the appearance of this phenomenon.
Paroxysmal bradycardia
Slow pulse is often registered against the background of a stressful situation in children prone to developing affective-respiratory attacks. At risk are children who have had pathological births, severe infectious diseases and intoxications, and those suffering from somatic diseases. Pathological pregnancy of the mother and pedagogical neglect of the child increase the likelihood of attacks.
The diagnosis of paroxysmal bradycardia is not correct; pediatricians like it to differentiate these attacks from other forms of slow heart function.
In some children, any minor excitement can lead to the development of an affective-respiratory attack. The development of the paroxysm occurs according to the following scheme: the first phase of the so-called white attack (the child's skin turns very pale) begins with a quiet muttering, the parasympathetic division of the autonomic nervous system is activated. Then the automatism of the sinus node is disrupted and the pulse rate decreases significantly, blood pressure may fall. The child becomes quiet, goes limp and loses consciousness. Convulsions may occur. All this happens very quickly, literally in a few seconds. Bradycardia can lead to an attack of asystole.
Children with heart pathologies may develop cardiac conduction block of varying degrees. Attacks are generally preceded by stressful situations – fear, rage, strong excitement, but sometimes the provoking factor cannot be determined.
Even after one such attack, a child must be shown to a cardiologist and thoroughly examined for various pathologies.
Bradycardia in the morning
Morning slowing of the pulse can be physiological. At night the heart works slowly, there is no load and increased need for oxygen, therefore morning bradycardia, while the body has not yet switched to the daytime rhythm, should not bother, if it is not accompanied by symptoms of hypoxia, pronounced arrhythmia - either acceleration of the heart rate up to flickering, or a noticeable slowing and stopping of the pulse. Some may experience attacks of sudden fear of death, dizziness, convulsions, wheezing when breathing, shortness of breath.
Expressed symptoms in the morning after a night's rest, not provoked by worries, even if the condition normalizes during the day, should be a reason to consult a doctor. Self-medication in this case is dangerous. [ 20 ]
Transient bradycardia
Acute transient disturbance of heart rhythm towards slowing down can be caused by temporary external reasons (fright, strong excitement). This condition often occurs in children and appears as a result of holding the breath.
In early childhood (up to three years), bradycardia attacks are observed in children before bedtime, especially after a day filled with emotional outbursts and experiences (attending a play, a children's party, an entertainment complex). Before bedtime, emotions fade and this leads to a slowdown in cardiac activity.
Such transient attacks are not accompanied by pronounced symptoms, maximum weakness, drowsiness, sometimes fainting, [ 21 ] and, as a rule, their causes are obvious. They are more common in children, but can also appear in hyper-emotional adults.
If transient bradycardia is accompanied by symptoms indicating a hemodynamic disorder and is not caused by external factors, then you should consult a doctor.
Cerebrovascular bradycardia
Against the background of pronounced bradycardia, oxygen starvation of the brain develops, and it consumes a lot of oxygen, the lack of which leads to dizziness, fainting and convulsions. These are standard manifestations of pronounced bradycardia, complications of which can be acute cerebrovascular accidents. [ 22 ]
There is also a feedback. Slowing of the heart rate can be part of the symptom complex of cerebral catastrophes: ischemic and hemorrhagic stroke, thrombosis of the cerebral arteries. Cerebrovascular bradycardia is one of the symptoms of post-stroke stupor or coma.

