Medical expert of the article
New publications
Bacterial and non-bacterial flora in the smear
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
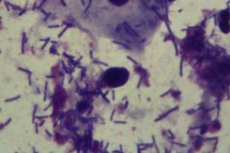
The normal microflora of the female genital tract is characterized by species diversity with a predominance of anaerobic microorganisms. Aerobes, which need air for active life, are found in small quantities in a smear on the flora. An increase in their content indicates a violation of the vaginal environment, an imbalance of beneficial and harmful bacteria.
Typical representatives of anaerobes include Doderlein's bacilli, or lactic acid bacteria, which maintain an acidic environment in the vagina that is destructive to pathogens. A large number of lactobacilli help to restrain the penetration and reproduction of other, non-useful anaerobes, which are suitable for an environment without air access, gardnerella, as well as coccal microflora, which constantly lives on the human body. Activating and multiplying, pathogenic microflora in the fight for food begins to suppress the growth and reproduction of useful lactobacilli, which is not prevented even by the introduction of the latter from the outside in the form of medicinal suppositories.
The coccal flora in the smear, the representatives of which have a spherical shape, can be presented in all the richness of its species. Normally, cocci together with other opportunistic and neutral microorganisms in the vagina are present in a total volume of no more than 5%. But with a weakening of the immune defense, excessive passion for intimate hygiene, the use of drugs that negatively affect lactobacilli, the balance of microorganisms in the vagina is disturbed.
In the fight for survival, some pathogens themselves begin to destroy the lactic acid flora. Thus, enterococci found in a smear, as the most aggressive anaerobes, can significantly reduce the number of Doderlein bacilli.
Most often, smears reveal fecal enterococci, which can enter the vagina as a result of insufficient intimate hygiene or during sexual intercourse. The bacteria is found in 25% of women, but with an insignificant number of bacterial cells it does not pose a danger. When the immune defense is weakened, enterococci are capable of not only actively multiplying, but also destroying beneficial microflora.
Moreover, settling in the vagina, they can move towards the urinary system, causing inflammatory processes with severe pain syndrome. At the same time, it is not so easy to detect enterococci due to their similarity to streptococcal infection, and it is even more difficult to cure. They are sensitive to a small group of antibiotics, and even those usually only reduce the number of bacteria.
Streptococci and staphylococci are gram-positive microorganisms that constantly live on our skin and mucous membranes, and sometimes penetrate into the body, so it is not surprising that these bacteria are found in small quantities in the normal microflora of the vagina. They are classified as aerobic and facultative anaerobic bacteria that can live both in the air (oxygen is not harmful to them, as for true or obligate anaerobes) and without it.
An increase in the number of streptococci and their predominance over the beneficial lactic acid bacilli of Doderlein against the background of moderate leukocytosis (leukocytes no more than 50 in the field of vision) indicates an imbalance of microflora (dysbacteriosis of the vagina). This condition in itself is not considered a full-fledged disease, but it can cause the proliferation of other pathological microflora (gardnerella, fungal flora), i.e. the development of bacterial vaginosis, in which gardnerella and other anaerobes predominate, and the number of lactobacilli is extremely small, and candidiasis (a disease of fungal origin).
It is important to understand that a streptococcal vaginal infection is not dangerous in itself, either for a woman or for her sexual partner with normal immunity. But it can be dangerous for the fetus if the woman is pregnant. Infection can occur both when the infection is introduced through the placenta (and these are pathologies of the child's development, often miscarriages at different stages), and during passage through the birth canal (inflammatory diseases of the lungs, brain, blood poisoning).
The situation is identical when staphylococcus is detected in a smear on flora. This is also a representative of opportunistic microflora. If its content in the vaginal environment is less than 1%, there is no need to worry. And a slight increase in the number of bacteria without an increase in the number of leukocytes is not considered a cause for concern, so staphylococcal infection should be considered only in conjunction with the count of the number of leukocytes.
An excess of opportunistic coccal microflora without an increase in the level of leukocytes indicates a pathology of a non-inflammatory nature - vaginal dysbacteriosis. But an increase in the content of leukocytes indicates an inflammatory disease, the progression of which can be judged by the degree of leukocytosis.
Staphylococcus aureus and hemolytic staphylococcus are considered the most dangerous in terms of the development of purulent-necrotic processes. The latter is much less common than other types of staphylococcus. However, otolaryngologists often encounter Staphylococcus aureus when diagnosing otitis, purulent forms of tonsillitis, and some other infectious diseases of the ear, throat, and nose.
An active staphylococcal infection in the vagina can be suspected by the presence of purulent discharge of a yellowish or greenish color, but a visual assessment is not enough to make a definitive diagnosis.
The fact is that the activation and proliferation of opportunistic coccal microflora may be evidence of the penetration into the body and parasitism of pathogenic bacteria transmitted sexually. In this case, purulent discharge may also be detected, but the pathogen will be different, which means that the approach to treatment should be different, not to mention the prevention of infection.
Another representative of coccal flora is gonococcus. This is a gram-negative round bacterium from the genus Neisseria gonorrhoeae. Unlike streptococci, staphylococci and enterococci, which are opportunistic microorganisms, gonococcus is considered a true parasite. Gonococci should not be present in a smear of flora at all, because they are not permanent residents of our body. If they are found, then we are talking about a sexually transmitted infection.
Gonococcus is the causative agent of an STI called "gonorrhea", which is characterized by purulent inflammation, most often in the genitourinary system. Similar to enterococci, in the vaginal environment these bacteria are quite resistant to various influences, easily adapt to changing living conditions and quickly develop resistance to antibiotics. But outside the body they die even with moderate heating or drying of the nutrient substrate, are afraid of soapy water and most antimicrobial agents.
If the body is able to cope with opportunistic microflora on its own by producing neutrophils and other immune system cells, then pathogenic flora in a smear is a great danger, and it is impossible to cope with it without outside help. Even after being absorbed by neutrophils, gonococci remain viable and can multiply.
We have examined representatives of the coccal microflora that can be found in smears in women, but in reality, even in a normal vaginal environment, about 100 varieties of microorganisms coexist, having different shapes and sizes.
In addition to spherical bacteria, elongated microorganisms, i.e. rod-shaped, can be found in vaginal discharge. This shape is typical of bacilli, which include Doderlein's rods.
But the rod-shaped flora in a vaginal smear may be more diverse, which is not an optimistic symptom. The detection of a small number of small rod-shaped organisms in the discharge of the genitals can hardly be considered a cause for concern, especially if there are no symptoms of malaise. But abundant small rod-shaped flora may be evidence of gardnerellosis or vaginal dysbacteriosis.
Gardnerella, as a representative of opportunistic facultative anaerobes, is found quite often in a smear on the flora, considering that strong immunity is only a dream for many of us due to constant stress, poor nutrition, chronic diseases and other negative external and internal factors.
Small rod-shaped bacteria do not pose a particular danger, but they can undermine the body's defenses, creating an environment for the reproduction and growth of chlamydia, gonococci, and trichomonas. Gardnerellosis itself is not a sexually transmitted infection. Bacteria can be detected even in those who are not sexually active, but have been exposed to factors that have weakened the general and/or local immunity. In men, the disease is usually asymptomatic, and women are diagnosed with bacterial vaginosis, which is accompanied by the corresponding symptoms: scanty discharge (white, yellowish or transparent), with an unpleasant fishy odor.
The phrase "clue cells" is often used in connection with gardnerellosis. This is the phrase used to describe a somewhat unusual disease that some doctors are trying to actively treat, while others are actually ignoring. Clue cells are particles of flat epithelium with small rod-shaped microflora attached to them called gardnerella.
Key cells in a smear test are direct evidence of bacterial vaginosis caused by rod-shaped microflora (gardnerella). In men, such cells on the penis can only be detected after sexual contact with a woman who has active gardnerella in her vagina. With weakened immunity, gardnerella joins other flora of the penis and can cause bacterial balanoposthitis (inflammation of the head of the penis), especially if bacteria accumulate under the foreskin due to poor or irregular intimate hygiene.
In addition to Doderlein and gardnerella bacilli, the normal vaginal microflora also includes other bacilli that differ in the size and shape of the rods, but are still smaller than lactobacilli. Polymorphic rod-shaped flora is always present in the smear, but it is dangerous only when its concentration is high, because actively multiplying, they begin to suppress the beneficial rod-shaped microflora.
Sticks of different sizes and shapes can provoke the development of various diseases of non-inflammatory (dysbacteriosis) and inflammatory nature, while a woman's vaginal discharge increases (white, gray, greenish, have a sour smell), itching, discomfort during urination, pain during sexual intercourse, discomfort in the lower abdomen appear. These symptoms are similar to a fungal infection (candidiasis), which causes an erroneous diagnosis during self-diagnosis. A smear test allows you to avoid such errors in diagnosis, and accordingly in treatment.
The rod-shaped microorganisms that can be found in humans include E. coli. This is a gram-negative bacterium, most strains of which are harmless, and some are even beneficial. Living in the intestines, they produce vitamin K and help fight pathogenic bacteria.
But E. coli is only useful for the intestines, and when it gets into other organs it can cause various inflammatory diseases (peritonitis, prostatitis, colpitis, vaginitis) or complicate the course of existing infections, so E. coli in a smear on the flora is considered a bad symptom. Normally, this microorganism should not be present in the vagina or urethra, which is possible only if the hygiene of the genitals is observed.
Corynebacteria, which are rod-shaped gram-positive anaerobes, can also be found in a smear of the flora of a healthy woman. It should be said that this bacterium has several varieties, among which there are safe and pathogenic. In the vagina, corynebacteria normally coexist with other microorganisms, and an increase in their number is observed only with dysbacteriosis. They themselves are usually not the cause of a violation of the biocenosis, but actively multiplying on the soil prepared by other pests, they displace beneficial lactobacilli. Corynebacteria are isolated in 60-70% of cases of urogenital infections, although in themselves, being representatives of opportunistic microflora and living in the body of a healthy person in decent quantities, they are not capable of provoking a serious disease.
But corynebacteria found in a throat or nasal smear no longer seem harmless, because some of its species are the causative agents of a severe and dangerous disease - diphtheria, and other non-diphtheria strains (diphtheroids) can cause acute inflammatory diseases of the upper respiratory tract - pharyngitis, otitis, lymphadenitis.
Diphtheroids can also be detected in a vaginal smear, and in small quantities they are not dangerous. They are often found in the vaginal epithelium of little girls, and in the nasopharynx they, along with staphylococci, make up the bulk of the microflora.
Diphtheroid flora in a smear is dangerous if it, together with other pathogens, prevails over beneficial lactobacilli. If there are enough lactobacilli in the vagina, the concentration of opportunistic microflora is unlikely to increase to a critical level. In the respiratory tract, diphtheroids can only multiply against the background of a noticeable decrease in immunity, together with staphylococci and other inhabitants of the respiratory system.
Sometimes the results of a smear test can be a bit confusing. For example, the phrase "coccobacillary flora in a smear" can be confusing, because we know that cocci are round bacteria, and bacilli are rod-shaped microorganisms. So what are coccobacilli?
Coccobacilli are a group of bacteria whose shape is intermediate between a sphere and a rod. These are bacteria of an oval, slightly elongated shape, which include Haemophilus influenzae (found in throat and nose swabs during influenza), Gardnerella (we wrote about them above), Chlamydia (the causative agent of chlamydia), Aggregatibacteria actinomycetemcomitans (causes severe inflammation of the gums).
We will dwell in more detail on coccobacilli parasitizing the genitals. If many doctors consider gardnerellosis a minor infection, then you can’t say the same about chlamydial infection, although a long absence of pronounced symptoms of the disease may predispose to it. But doctors know how dangerous chlamydia is.
Chlamydia is not so easy to detect in a smear on flora, because these bacteria have some properties of viruses. They penetrate a living cell and parasitize inside it, after which the cell becomes non-viable, and the bacteria changes its place of residence. Under a microscope, bacteria can be seen only when the biomaterial is exposed to special staining reagents, but there is a high probability of a false result. The most reliable method for determining chlamydia is considered to be PCR analysis, therefore, if chlamydia is suspected, doctors prescribe this rather expensive but reliable study.
The danger of chlamydia is that the infection causes severe inflammatory processes and often occurs in a chronic form, significantly weakening the body. Moreover, long-term inflammation causes the formation of adhesions in the vagina and narrowing of the urethral canal, which causes infertility in women and men.
Another danger is the spread of infection to the uterine area, the development of inflammatory and dysplastic processes, which further reduces the chance of getting pregnant and carrying a child, but increases the risk of cancer. In both women and men, chlamydia can spread to the urinary system, joints, liver, peritoneum, etc., causing serious, severe and long-term inflammation.
In pregnant women, chlamydia can cause ectopic pregnancies, miscarriages, fetal growth retardation, and early delivery. Infection of a child during childbirth can lead to otitis and conjunctivitis, and if the bacteria remain in the body, problems with the heart, nervous system, and digestive system are possible. For girls, infection with chlamydia at an early age can lead to infertility in the future.
Unusual flora in smear
Chlamydia is an insidious infection that can be asymptomatic for a long time, and if symptoms appear (in the form of yellowish discharge, burning during urination, slight itching in the genital area), they are slightly expressed, and they can also disappear after a couple of weeks, which does not mean recovery. Similarity to viruses in behavior makes it difficult to detect chlamydia, but another bacterium, leptothrix, can “hint” at their presence.
Leptothrix is a special type of gram-negative bacteria that have an unusual shape - in the form of thin threads resembling a hair, which is why the microorganisms are named. Initially, these bacteria were classified as fungal microflora, but later it was decided that these microorganisms are more similar in their properties to bacteria, in particular lactobacilli, which explains the lack of changes in the acidity of the internal environment of the vagina when leptothrix is detected.
Leptortix in a smear on flora is detected in the form of chains of different lengths (from 5 µm to 75 µm). They get along well with lactobacilli and at the first stages of the disease do not cause noticeable symptoms, so they can be detected accidentally during a gynecological examination.
The infection is not sexually transmitted, and when bacteria are detected in men, it is not accompanied by any pathological symptoms.
Women usually have no complaints in the first half of the cycle. They appear in the second half of the cycle and are reduced to increased vaginal discharge (white or transparent, similar in consistency to water, odorless and lumpy), the appearance of itching and burning in the genital area and vagina, which occasionally intensify during urination. At the same time, a gynecological examination does not show any noticeable hyperemia or swelling of the vaginal walls.
At first glance, such bacteria do not seem dangerous, because we are not talking about an inflammatory process. But its ability to produce lactic and some other acids during active reproduction can increase the acidity of the vagina, and this is as bad as its decrease. With increased acidity of the internal environment, damage to the cells of the mucous membrane and nerve endings is possible, which can cause incomprehensible pain in the vagina (vulvodynia).
In addition, leptothrix, the appearance of which is associated with improper treatment of thrush and a decrease in local immunity, is often a signal of other infections, since it is often combined with a fungal infection (candidiasis), chlamydia, trichomoniasis, and gardnerellosis.
Another bacterium, leptotrichia, is similar in structure to leptothrix, but the symptoms will be somewhat different: discharge becomes abundant, acquires a grayish tint and an unpleasant odor, in addition to itching and burning in the vagina, there is also pain during intercourse, and studies show an increase in vaginal pH, i.e. a decrease in its acidity. That is, we are dealing with one of the varieties of bacterial vaginosis, which requires appropriate treatment.
In addition, one of the rare varieties of leptotrichia can cause various pregnancy complications in expectant mothers. Such flora in a smear can cause inflammation of the fetal membranes, inhibition of its development, premature birth, sepsis in weakened mothers, etc.
Actinomycetes have some similarity with leptothrix and leptotrichia in their structure. These facultative anaerobes, which can live both in and out of air, look like the thinnest rods with thickened edges, forming threads of different lengths (up to 50 microns). Due to their ability to form a developed mycelium (similar to mushrooms), they were also initially classified as fungal microflora, but it turned out that these microorganisms have more similarities with bacteria.
This fairly common type of bacteria can be found in soil, including sand (up to 65% of all microflora), in water (tap, spring, from springs), and on plants. It has no difficulty in penetrating the human body during meals or hygiene procedures, but this does not mean that a person will get sick. The fact is that actinomycetes are not able to penetrate healthy skin and mucous membranes. Another matter if there was an injury to the skin.
Actinomycetes in a smear on flora in small quantities can be detected in healthy people, but with a normal protective function of the skin, this does not matter. But with damage to the skin or mucous membranes against the background of weakened immunity, the development of a non-specific inflammatory process is quite possible. So women begin to complain of pain in the lower abdomen of various localizations, a sharp increase in temperature to 40 degrees (most patients).
Most often, the inflammatory process involves the appendages. At first, it is a simple inflammation. Then, infiltrates appear in the form of seals, fistulas with purulent discharge may form, multiple adhesions in the pelvic area, and problems with conception arise.
Despite the fact that actinomycosis is not diagnosed very often, the consequences of the disease are far from attractive, so even a small increase in the number of these unusual bacteria should alert doctors, especially since conventional anti-inflammatory therapy (antibiotic therapy, the use of sulfanilamide drugs, surgical treatment) only give short-term results, and thermal physiotherapy only worsens the situation. Only complex treatment taking into account the clinical picture, the characteristics of the disease and the individual characteristics of the patient's body gives positive results in the treatment of this resistant infection.
Non-bacterial flora in smear
When considering the different types of flora in a smear, it is worth noting that coccal, rod-shaped and filamentous bacterial microflora are not the only ones possible in the female vagina. Other microscopic organisms can also penetrate there, such as fungi and trichomonads - single-celled parasites that cannot be classified as bacteria, viruses or fungi.
Trichomonas is a pathogenic, i.e., pathogenic microflora, so its detection in a smear on the flora does not bode well. The disease itself, provoked by trichomonas, is called trichomoniasis and is classified as a venereal disease. It is clear that the infection is transmitted sexually, and the disease is considered very contagious, so if trichomonas is detected in one of the sexual partners, the other must also be examined.
Trichomoniasis is one of the most common STIs. This is due to the high level of contagiousness and often insufficient attention to it from doctors and patients. Trichomonas themselves are very active microorganisms, prone to moving quickly, preferring a moist environment without air access, so they feel very comfortable in the female vagina or urethra (in men, the disease usually affects this part of the genital organ).
The following symptoms indicate trichomoniasis in women:
- foul-smelling, frothy vaginal discharge that can range in color from white or grayish to yellow or green,
- The discharge may contain pus and be accompanied by itching and burning in the genital area.
Painful urination, aching pain in the lower abdomen, discomfort during intercourse can also be symptoms of STIs in women. In men, the disease can proceed without pronounced symptoms or be accompanied by pain during urination, signs of inflammation of the prostate, itching and burning after ejaculation, purulent and mucous discharge from the urethra, frequent urination.
It should be said that for most men and some women the disease does not have any obvious symptoms for a while. Sometimes such a latent course can last for years, while the person remains a source of infection all this time.
But even the latent course of the disease does not bode well, because it can cause infertility in men and problems with pregnancy in women, increases the likelihood of developing other sexually transmitted infections and HIV. Although the treatment of the disease is generally not difficult (a single dose of antibiotics is enough), the main thing is to detect it in time, which is easiest to do when examining smears from the vagina and urethra.
In almost all cases, the vaginal microflora is distinguished by a noticeable diversity of life forms. In other words, a smear reveals mixed flora, which contains various bacteria, fungi, and in some cases, microorganisms occupying an intermediate position (the same trichomonads).
Yeast fungi of the genus Candida are found in a smear on the flora in most women. They are considered representatives of opportunistic microflora and live in small quantities on our body (in the oral cavity, large intestine, vagina), without causing symptoms of the disease. The ability of fungi to actively reproduce usually occurs against the background of long-term antibiotic therapy or a noticeable decrease in immunity (general or local).
It is important to remember that any microscopic wound on the skin or mucous membrane is already a serious flaw in the protective shell of our body, because it is a breeding ground for opportunistic and pathogenic microflora. This is one of the main factors in reducing local immunity. And stress, any chronic diseases, frequent infections, uncontrolled use of certain drugs, immunosuppressant therapy, etc. can undermine the general immunity.
The detection of mycelium (mycelium in the form of a developed network of threads) or spores (reproductive cells of fungi) in a smear on flora indicates that the infection has begun to multiply intensively. Despite the fact that both fungi and bacteria have the ability to form spores, the expression "spores in a smear on flora" is most often used in relation to fungal microflora. If bacterial spores are one of the types of existence of a bacterial cell, allowing it to survive in unfavorable conditions, then fungal spores are cells that serve for their reproduction. It is clear that in the second case there is a greater danger than the inactive existence of a microorganism.
Candidiasis, or thrush, is the most common fungal infection in humans, caused by oval or round microorganisms from the genus of yeast-like fungi Candida. These fungi in the process of life form numerous threads of pseudomycelium, formed simultaneously by both mother and daughter cells (unlike true mycelium, they are formed by budding, not division), and blastospores (asexual reproductive cells of yeast fungi, the so-called buds), which are found in a smear on the flora during its examination. This feature is characteristic of all yeast fungi, but most often we are talking about Candida fungi.
Candidiasis is a disease that is diagnosed in two cases: with active reproduction of fungi or with the detection of their pathogenic strains, which even in small quantities can provoke the disease, suppressing local immunity. Candidiasis of the oral cavity and vagina is quite easy to detect using a smear from the corresponding area.
Fungal infection of the genitals is more often diagnosed in women, because the vagina creates optimal conditions for the reproduction of microorganisms: warm and humid, and it is only necessary to slightly correct the internal environment of the vagina towards alkalization, as the fungi begin to actively reproduce and spread to healthy areas. In women, fungal infection causes candidal vulvovaginitis, in men - balanitis or balanoposthitis, characterized by tissue inflammation (hyperemia against the background of minor edema) and the appearance of a white cheesy coating with a sour odor (in women in the form of vaginal discharge). Patients may also experience excruciating itching, burning in the genital area, pain during intercourse or urination.
In case of oral candidiasis, the tongue is the first to be covered with a white coating, the skin of which acquires a bright red or burgundy hue and may burn a little when eating food with a strong taste. The coating is quite easily removed from the tongue, so taking material for examination (smear or scraping) is not particularly difficult.
Conditionally pathogenic flora in a smear, which includes many bacteria and fungi (for example, fungi that cause thrush), is considered a symptom of the disease only if it is actively multiplying, which is determined quantitatively. But the detection of pathogenic strains even in small quantities is a cause for concern and a more serious examination, because a disease caught at an early stage of development is easier to treat and causes less harm to health. However, given the fact that many conditionally pathogenic microorganisms live on our body constantly and it is impossible to completely get rid of them, a large role is given to maintaining immunity, which is an important point in the prevention of various infections.


 [
[