Medical expert of the article
New publications
How to restore and treat the flora in the smear?
Last reviewed: 08.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The flora in the smear is not a pathology, so it is not the flora itself that needs to be treated, but the deviations in its composition, changes in the concentration of the existing components and the consequences of this. Since the main useful and unhealthy part of the internal environment of the vagina, urethra, oral cavity are bacteria, the question of how to treat the flora in the smear looks trivial, because the vast majority of us know that antibiotics exist for this. It would seem that go to the pharmacy, ask for an antibiotic and the problem is solved. But the question is not this, but how to determine an effective drug and its necessary dosage. In addition, it is not a fact that fungal microflora does not also act underground in the body along with bacteria, the treatment of which is carried out with completely different drugs.
Before you start treating the microflora in a smear, you need to figure out whether everything is so bad? Only a specialist doctor can understand and explain what the test results show, who then either offers additional studies or relies on the results obtained and prescribes a specific treatment, which ideally should consist of two points:
- destruction of pathogenic or excessively proliferated opportunistic microflora,
- restoration of the normal internal environment of the body, in particular the intestines and vagina,
- restoration and maintenance of general and local immunity.
Following only one or two of these points will not give good and lasting results, unless we are talking about dysbiosis, when it is often limited to prescribing only those drugs that normalize the microflora.
If we are talking about a bacterial infection, the treatment of which cannot be done without the use of antibiotics, it is very important to do not only a microbiological examination of the smear, but also to determine the type of infection, as well as its sensitivity to antibiotics (the most popular analysis in this regard is the polymerase chain reaction method or PCR analysis).
Recently, many strains of bacteria already known to us have appeared that either do not respond to antimicrobial agents or have developed their own defense system against them, so treatment prescribed at random without taking into account the specific strain of the pathogen may be a shot in the dark. After all, even the generally prescribed broad-spectrum antibiotics are not designed to destroy all types and strains of bacteria. Well, there is no such universal medicine yet, and it is practically impossible to create one, given that new and new mutated strains regularly appear.
As for the fungal infection, at first glance it would be possible to do without a smear, because the symptoms of candidiasis are quite specific - white plaque, cheesy discharge, itching. But thrush in different people can also have slightly different manifestations, and white plaque with or without itching is characteristic not only of a fungal infection. So here, too, it is best to let specialists sort out the diagnostic issues.
If the diagnosis is finally established, then along with hygiene measures, it will be necessary to carry out treatment procedures using antifungal drugs. It is also necessary to understand that even those infections that are not STIs can be transmitted sexually, especially if the partner has damaged genital skin or mucous membranes, so it is worth abstaining from sexual intercourse during treatment. After all, what one or two bacteria cannot do, their "army" can do, especially if the sexual partner cannot boast of strong immunity.
As we can see, the treatment of flora in a smear and the approach to its prescription are much more complicated than simply smearing a broken knee with brilliant green. At the same time, different types of infection require an individual approach to the choice of drugs, not to mention the fact that the requirements for the treatment of opportunistic microflora and STIs differ significantly.
Treatment of coccal flora in smear and not only
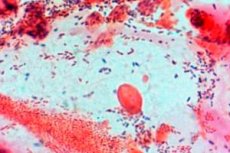
Needless to say, most infectious diseases of the respiratory and genitourinary systems are associated with the activation of opportunistic microorganisms living on the skin of our body? Most of them are spherical bacteria called cocci, and among them, streptococci and staphylococci come to the fore, individual strains of which cause most of the infectious diseases known to us. Not only that. Coccal flora can also be detected in diseases caused by other pathogens, so the question of what to treat coccal flora in a smear with, if necessary, is quite logical and relevant.
The infection localization site in women can be the external and internal genitals. And if removing the infection from the surface of the genitals is not difficult, then treating the vaginal microflora and bacteria that penetrate into the uterine area is more difficult, because regular hygiene procedures and treating the surface with antiseptics will not help here.
The most optimal method of treating vaginal opportunistic coccal microflora is considered to be the use of vaginal tablets and suppositories with an antibiotic. During pregnancy, doctors may prefer rectal suppositories due to the proximity of the rectum and female reproductive organs. Gynecologists have many drugs in this area at their disposal: Polizhans, Terzhinan, Metronidazole, Clindacin, Clarithromycin, Fluomizin, Trichopolum, Sintomycin, Klion-D, Hexicon (suppositories with a strong broad-spectrum antiseptic), etc.
The list of drugs is quite large and there is no point in listing them all, because when prescribing treatment, doctors focus not only on the action of antimicrobial agents, but also on the nature of the infection, the characteristics of the patient's body, her condition, so all prescriptions are strictly individual. Friends and advertising in the media are not the best advisers in this matter, because the infection needs to be cured, not treated, as often happens with self-medication.
Since coccal flora in a smear for diseases of the genital area is very rarely present in proud solitude (usually we are talking about mixed microflora, including fungal infection), most drugs for the treatment of gynecological diseases are combined, i.e. they contain a topical antibiotic and an antifungal agent. This is a very important point, because we already know that with antibiotics alone it is possible to destroy bacteria, but it is impossible to cope with fungi. Combined drugs include Terzhinan, Polizhans, Neo-Penotral, Klion-D, Gynomax and some others.
Usually, local application of antibiotics helps kill two birds with one stone: destroy the infection and relieve inflammation. But if the inflammatory process is severe, it makes sense to prescribe drugs containing steroids (the same "Terzhinan" in addition to two strong antibiotics neomycin and ternidazole contains the antifungal component nystatin and the glucocorticosteroid prednisolone). If the inflammation does not subside, doctors additionally prescribe systemic antibiotic therapy with drugs that are relevant in each specific case.
Most antimicrobial drugs used in gynecology have a broad spectrum of action, so they are used to treat mixed infections, which include cocci, harmful rods, coccobacilli, fungi, and even STI pathogens, including the parasite trichomonas. But the prevalence of one or another form of microorganism requires doctors to select an appropriate treatment regimen, and sometimes a combination of different drugs.
If we are talking only about the activation of a fungal infection, and other indicators of opportunistic and pathogenic microflora remain normal, there is no point in prescribing drugs with an antibiotic, which, along with pathogens, can also destroy beneficial lactobacilli. In this case, it is more logical to turn to simple antifungal agents such as Pimafucin, Clotrimazole, Fluconazole, Flucostat, which are also available in vaginal forms and in tablets.
A very important role in the treatment of vaginal infections is given to medical and hygienic procedures. It is not enough to keep the external genitalia clean, it is also very important to clean the vagina, which is most conveniently done by douching. This procedure helps to remove microorganisms from the vagina that have already died under the influence of antibiotics and antimycotics and reduce the number of living ones. Especially if for this purpose you use not only anti-inflammatory folk remedies (infusions of chamomile, St. John's wort, calendula, yarrow, etc.) and a soda solution, but also pharmacy antiseptics (Chlorhexidine, Miramistin, Chlorophyllipt, a weak solution of potassium permanganate, etc.).
How much needs to be taken into account just to prescribe the first point of complex treatment, which is aimed at destroying pathogenic microbes. But this is not enough. By destroying pests, potent drugs significantly thin out the ranks of useful lactobacilli, and if their volume is not returned to the required 95%, the results of the treatment will be short-lived. It is not for nothing that popular wisdom says that a holy place is never empty, and the place of lactobacilli will soon again be occupied by actively multiplying opportunistic microflora.
After antibiotic or antifungal therapy, the gynecologist takes a repeat smear to assess the effectiveness of the treatment. If the patient has not taken any measures to restore the beneficial microflora of the vagina, it may not be comforting at all.
To avoid this, even during antibiotic therapy, which usually lasts 5-7 days, or immediately after it, you need to take care of restoring the microflora by introducing lactobacilli into the vagina in the form of vaginal preparations and creating conditions for their normal functioning and reproduction.
There are various medications for restoring vaginal microflora: "Atsilak", "Laktozhinal", "Biosporin Femina", "Gynoflor", "Laktonorm", "Vaginorm", "Vagilak" and others. But if the patient was prescribed systemic antibiotic therapy, then most likely it is necessary to restore the intestinal microflora by taking the appropriate medications ("Bifidumbacterin", "Lactobacterin", "Laktovit", "Narine", etc.).
When considering how to restore flora in a smear, we must not forget that any infection is a blow to the body's immune system. And with a weakened immune system, even a sufficient number of lactobacilli cannot always cope with pathogenic competitors. If lactobacilli can somehow keep opportunistic microflora within limits, then to combat pathogens, a joint effort of both local (lactobacilli) and general immunity is required.
Thus, we have come to the need for the third point of treatment of gynecological infections, i.e. restoration of the body's defenses through immunostimulants of plant and synthetic origin and systemic probiotics, which will take care of general immunity, while vaginal preparations for restoration of microflora will provide local immunity.
As for the treatment of urogenital infections in men, the treatment regimen may differ significantly depending on the location of the infection. If we are talking about infectious balanitis or balanoposthitis, which affect the exposed parts of the male genital system (the head and foreskin of the urethra), then preference is given to local drugs (antiseptics and ointments/gels with antibiotics). Systemic antibiotic therapy is prescribed only for severe inflammation that does not go away despite local treatment.
In case of urethral infection, access to the site of its dislocation is limited, so internal administration of antibiotics is necessary in most cases. But this is not the end of the treatment. In addition, to remove pathogens from the site of inflammation, urethral lavage with local antiseptics is used, for which special attachments are provided.
The point about restoring the beneficial microflora of the genitals for men is not relevant for obvious reasons, but it is still worth increasing the body's resistance to infections. And here there are no purely male or female drugs.
ENT infections are treated by an otolaryngologist, who should prescribe effective drugs for the treatment of diseases of the ear, throat, nose, based on the localization of the lesion, the pathogen, i.e. the flora detected in the smear, the characteristics of the patient's body. The fact remains that bacterial infections are treated with antibiotics, and fungal infections - with antifungal agents. Antiseptics can be used in any case for gargling or irrigating the throat, washing the nose and ear, treating wounds on the skin and mucous membranes.
Treatment of STIs
If active opportunistic flora in a smear is considered to be the result of a decrease in general and/or local immunity, then sexually transmitted infections (STIs) are most often the result of indiscriminate sexual contact. Innocent people (wives, husbands, lovers) who, although they had contact with only one sexual partner, got the infection from their unfaithful partner may also suffer.
It should be said that immunity is not a decisive factor in STIs, because this type of infection has the ability to survive in difficult conditions and at the same time have a detrimental effect on immune cells. The survival of the species is also facilitated by the high contagiousness of the infection, which easily changes its location, passing from one person to another. In connection with the latter fact, it is necessary to understand that seeking help from one patient should be accompanied by examination and treatment of all his sexual partners, as well as preventive treatment of those who were in close household contact with the infected.
When prescribing optimal treatment regimens, doctors always rely on the nature of the pathogen. After all, it has been proven experimentally that not all antibiotics are equally effective against gonorrhea, trichomoniasis, chlamydia and syphilis, the pathogen of which is pale treponema (it can be detected by examining a scraping from the surface of a specific rash). In a regular smear with subsequent analysis for the pathogen, chlamydia, gonococci, trichomonas are detected, to combat which various therapeutic regimens are used.
Thus, the drugs of choice for the treatment of gonorrhea are cephalosporins (ceftriaxone) and fluoroquinolones (ciprofloxacin, ofloxacin). Spectinomycin, cefotaxime, ceruroxime, lomefloxacin and norfloxacin can be used as alternative drugs, but the effectiveness of treatment may be somewhat lower, which is very undesirable.
For the treatment of urogenital chlamydia, a drug from the macrolide series, azithromycin, and the tetracycline antibiotic doxycycline are used. Erythromycin, ofloxacin, roxithromycin, and spiramycin can serve as alternatives.
Metronidazole is usually used to treat trichomoniasis. Alternative drugs that should be prescribed if metronidazole is ineffective are representatives of the same group (imidazole derivatives): tinidazole and ornidazole.
In this case, various treatment regimens may be prescribed, from a single high-dose antibiotic treatment, which is used to treat gonorrhea and trichomoniasis, to a 7-day course (for chlamydia and trichomoniasis). Treatment regimens and drug dosages are prescribed individually, taking into account the severity of the disease, the characteristics of the patient's body and his condition. In addition to antibiotic therapy, they also include the restoration of vaginal microflora for women and strengthening the immune system for patients of either gender.
Let us remind you once again that treatment of STIs involves examination and treatment (if necessary) of all sexual partners of the patient. It is very important to abstain from sexual contact during treatment to prevent the spread of infection and infecting other people.
Treatment of unusual infections and leukocytosis
As we have already mentioned, the contents of the smear may include microorganisms that many people have heard little about or even did not suspect their existence. This may be even more frightening than the mention of streptococcal, staph and other common infections. In fact, everything is not so scary and is quite treatable.
If the flora in the smear contains such microorganisms as leptothrix or leprothrichia, the need for treatment is determined primarily by the presence of inflammation. In its absence, doctors can only suggest taking a course of immunostimulants, which should prevent the development and spread of infection. At the same time, it is very important to pay attention to other components of the internal environment, for example, the presence of a concomitant infection (usually candidiasis or STIs).
Treatment of elevated leukocytes in a smear on flora against the background of an existing infection, which indicates the nature of the inflammatory process, involves the appointment of:
- antibiotics of the penicillin or cephalosporin series, macrolides, aminoglycosides (locally and/or systemically),
- antifungal agents (or combination drugs) to prevent candidiasis as a consequence of antibiotic therapy,
- immunostimulants and immunomodulators,
- means for restoring normal microflora.
That is, the treatment regimen is no different from the treatment of other infections. At the same time, the treatment of leptotrichosis does not cause any particular difficulties and has a favorable prognosis if the disease is not advanced.
Unlike leptotrichosis, actinomycosis caused by actinomycetes presents certain difficulties both in diagnostics, because these unusual bacteria are often found in smears (especially from the nose and throat), without causing symptoms of the disease, and in treatment. In order to make a final diagnosis, the doctor has to prescribe additional studies (scrapings, punctures, pus culture, etc.), which last more than one day, although in 2-3 days individual actinomycetes are capable of creating entire colonies.
A special approach is also necessary for the treatment of this disease. The most important thing in the treatment of the disease is to increase the body's defenses by intramuscular injection of a special drug (actinolysate), stimulating phagocytosis and the production of antibodies to fight the infection. It is almost impossible to cope with actinomycetes using antibiotics alone, so they are prescribed mainly to destroy the concomitant infection. If necessary, surgical opening of the fistulas is performed.
The particular danger of actinomycosis is that the infection can spread to other organs and, in the absence of appropriate treatment, lead to death.


 [
[